ChiroMed: Sciatic Nerve Compression After Injury
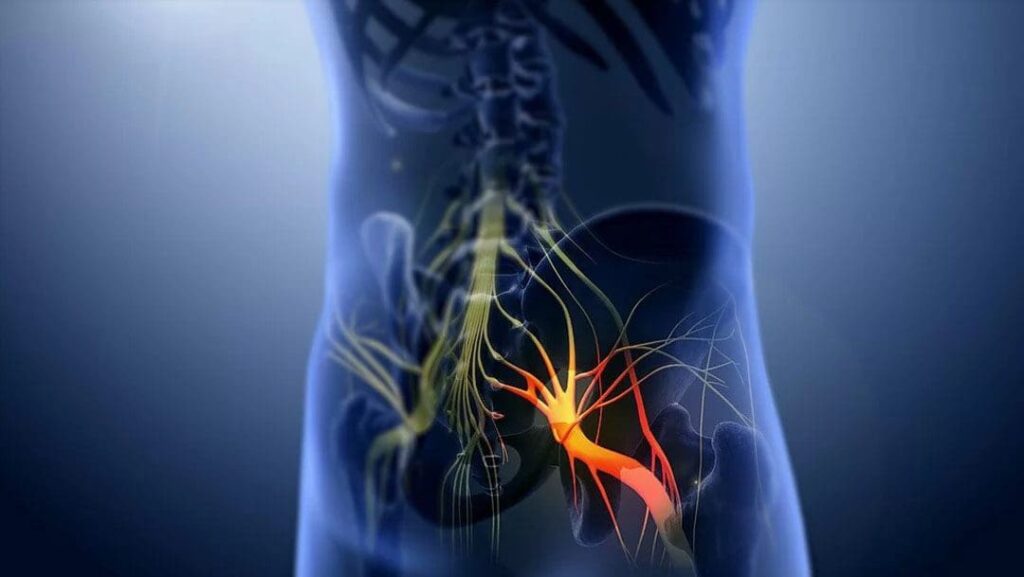
What’s really happening when the sciatic nerve is “under pressure”
When the sciatic nerve—or the lumbar nerve roots that form it—is compressed, pinched, or crushed, the nerve’s structure is physically altered. At first, the insulating layer (myelin) is disturbed, which slows or blocks signals. If pressure continues, the inner fiber (axon) can be damaged, and symptoms shift from “pins-and-needles” to numbness and weakness. In short: force + time = deeper nerve injury (Menorca et al., 2013; NCBI Bookshelf, n.d.). PMC+1
Why does that cause pain, tingling, and weakness?
- Mechanical squeeze: Pressure deforms the nerve and disrupts normal electrical conduction.
- Ischemia (low blood flow): Compressed microvessels reduce oxygen and nutrients, worsening function.
- Inflammation and swelling: Edema inside tight tunnels raises pressure further, feeding the cycle.
Over time, this can progress from a reversible conduction block to axon damage with longer recovery (NCBI Bookshelf, n.d.; Verywell Health, 2023). NCBI+1
How injuries trigger sciatic pain
After a lift, twist, fall, or collision, structures that share space with the nerve can swell or shift:
- Disc bulge or herniation and spinal stenosis narrow the path for nerve roots.
- Bone spurs linked to osteoarthritis can crowd the exit for nerves.
- Deep-gluteal muscle tension can irritate the nerve as it travels through the buttock.
These changes explain radiating leg pain, tingling, and weakness—classic sciatica patterns (Mayo Clinic, 2023; Penn Medicine, n.d.). Mayo Clinic+1
Crush-type trauma (for example, a heavy object on the limb) may directly injure the sciatic nerve or create dangerous pressure in the leg compartments—an emergency because blood flow and nerve function can rapidly fail (Horton & Mendez, 2024; PhysioWorks, n.d.). Horton Mendez+1
The spectrum of nerve damage
Clinicians often describe three overlapping grades (you can think of them as insulation only → wire damaged → wire cut):
- Neurapraxia (mild) – Myelin/insulation injury → temporary signal block.
- Axonotmesis (moderate) – Axon disrupted → weakness and sensory loss until fibers regrow.
- Neurotmesis (severe) – Nerve continuity lost → often needs surgery.
(Menorca et al., 2013). PMC
Typical symptoms—and urgent red flags
Common: shooting leg pain, tingling or numbness down the leg or foot, and weakness (trouble pushing off or lifting the foot). A clinic test called the Straight-Leg Raise can reproduce leg pain when a nerve root is irritated (Penn Medicine, n.d.). Penn Medicine
Get urgent help now if you notice new/worsening leg weakness, foot drop, saddle numbness, or bladder/bowel changes—these can signal severe compression needing immediate care (ADR Spine, 2025). adrspine.com
“Double-crush”: why treating one spot may not be enough
A single nerve can be irritated at more than one location (for example, at the spine and through the deep-gluteal region). Two smaller squeezes can add up to big symptoms. Effective care addresses all contributing sites (Southwest Wound Care, n.d.). Southwest Regional Wound Care Center
How providers confirm what’s wrong
- Focused exam: strength, sensation, reflexes, and nerve-tension signs (e.g., Straight-Leg Raise).
- Imaging: MRI for disc/stenosis; MR neurography in select cases to map peripheral nerve injury.
- Electrodiagnostics (EMG/NCS): measure signal speed/strength to help grade injury and track recovery.
These steps make sure the plan fits the cause and severity (Penn Medicine, n.d.; MedStar Health, n.d.). Penn Medicine+1
What recovery aims to do (and how chiropractic fits)
Goal 1: Reduce pressure.
Goal 2: Restore blood flow and calm inflammation.
Goal 3: Rebuild motion, strength, and control so the nerve isn’t re-compressed during daily life.
The ChiroMed-style, integrative plan
Spinal manipulation/mobilization (when appropriate).
Restores joint motion and alignment to unload irritated nerve roots. Providers choose gentle, targeted methods that fit your presentation. (Penn Medicine, n.d.). Penn Medicine
Soft-tissue therapy.
Releases muscle guarding and improves nerve gliding in the deep-gluteal and hamstring regions. Skilled therapists avoid positions/pressures that aggravate nerve symptoms and tailor dosage to calm irritation (AMTA, 2020). American Massage Therapy Association
Rehabilitation exercises.
- Early: short, frequent walks and positional relief to keep blood moving without provoking pain.
- Progression: core and hip endurance, hip-hinge training, and gentle nerve-mobility drills (sliders) as tolerated.
- Lifestyle coaching: sitting breaks, sleep positioning, and lift mechanics to prevent re-compression.
Conservative care is first-line for most cases; procedures or surgery are considered if red flags appear or conservative care fails (Penn Medicine, n.d.; Mayo Clinic, 2023). Penn Medicine+1
Practical home strategies (that don’t backfire)
- Move in “snacks.” Several 3–8-minute walks daily beat one long session during a flare.
- Change positions often. Alternate sitting, standing, and lying every 30–45 minutes.
- Spine-smart bending. Hinge from the hips; keep loads close to the body.
- Sleep set-ups. Side-lying with a pillow between the knees, or back-lying with knees slightly elevated.
- Watch the response. Mild, short-lived symptoms after activity can be normal; sharp spreading pain or new weakness means scale back and message your provider.
These habits lower mechanical stress while the clinic plan restores capacity (AdvancedOSM, n.d.). advancedosm.com
Special scenarios to know
Crush injuries & compartment-type pressure.
Direct limb compression can injure the sciatic nerve or raise tissue pressure enough to cut blood flow—an emergency requiring urgent evaluation (Horton & Mendez, 2024; PhysioWorks, n.d.). Horton Mendez+1
Is it nerve compression—or something else?
Other conditions can mimic sciatica (e.g., hip disorders, systemic neuropathies). If symptoms don’t match a single level or linger despite care, expect your team to re-check the diagnosis and, if needed, expand testing (OSMC, 2025; MedStar Health, n.d.). OSMC+1
Bottom line for ChiroMed readers
A “pinched nerve” is not just irritation—it’s a physical change inside a living cable. The sooner we de-compress the nerve, restore circulation, and retrain movement, the better the chances for a strong recovery. Chiropractic-led, integrative care unites precise manual therapy, soft-tissue work, and progressive rehab—plus timely imaging and referrals when needed—to help you get back to work, sport, and life with confidence (Penn Medicine, n.d.; Mayo Clinic, 2023). Penn Medicine+1
References
Advanced Orthopaedics & Sports Medicine. (n.d.). Peripheral nerve compression. advancedosm.com
ADR Spine. (2025, March 3). Last stages of sciatica: Causes, symptoms, & treatment. adrspine.com
American Massage Therapy Association. (2020, February 13). Massage therapy for nerve compression injuries. American Massage Therapy Association
Horton & Mendez Injury Attorneys. (2024). Do crush injuries cause nerve damage?. Horton Mendez
MedStar Health. (n.d.). Lesion of the sciatic nerve. MedStar Health
Menorca, R. M. G., Fussell, T. S., & Elfar, J. C. (2013). Peripheral nerve trauma: Mechanisms of injury and recovery. Hand, 8(1), 31–37. PMC
Mayo Clinic Staff. (2023, March 16). Pinched nerve: Symptoms & causes. Mayo Clinic
NCBI Bookshelf. (n.d.). Biological response of peripheral nerves to loading: Pathophysiology of nerve compression syndromes. NCBI
OSMC. (2025, October 1). Is it nerve compression or something else? Common signs. OSMC
Penn Medicine. (n.d.). Sciatica. Penn Medicine
PhysioWorks. (n.d.). Compartment syndrome. PhysioWorks!
Verywell Health. (2023, June 21). How ischemia affects different parts of the body. Verywell Health
iCliniq. (n.d.). What is a sciatic nerve injury?. iCliniq
Align Wellness Center. (2025, March 18). Sciatica nerve pain mystery: Possible suspects for your sciatica woes. Align Wellness Center
Post Disclaimer
Professional Scope of Practice *
The information on this blog site is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to Chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somatovisceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and/or functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-C, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-C*, CCST, IFMCP*, CIFM*, ATN*
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Masters in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez DC, APRN, FNP-C, CIFM*, IFMCP*, ATN*, CCST
My Digital Business Card

