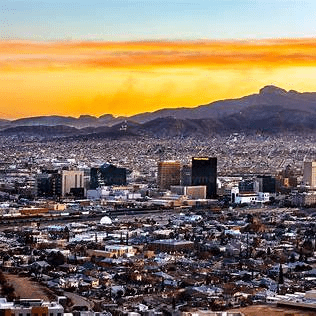
Neuropathy in El Paso, TX: Frequently Asked Questions
Diabetes Links and Local Care Options
Neuropathy is a common concern in El Paso, Texas, especially because diabetes is common in the region, and is one of the most common causes of peripheral neuropathy. Many people don’t just want another pill. They want to understand why the symptoms are occurring and what they can do (and what local treatment options are available) to protect function and quality of life.
This guide answers the most common neuropathy questions people ask in El Paso, with a clear focus on symptoms, causes (including diabetes), testing, and practical treatment options—including integrative chiropractic therapy and nurse practitioner (NP) care.
What is neuropathy?
Neuropathy refers to nerve damage or irritation. Most people are talking about peripheral neuropathy, which affects nerves outside the brain and spinal cord—often in the feet, legs, hands, or arms. Symptoms can range from mild tingling to burning pain, numbness, weakness, and balance problems. (Cleveland Clinic, n.d.; Mayo Clinic, 2023).
Neuropathy can also affect autonomic nerves, which help control body functions you don’t “think about,” like sweating, digestion, blood pressure, and sexual function. (Mayo Clinic, n.d.; Frontier Neurology, n.d.).
Why do neuropathy questions arise so often in El Paso?
People in El Paso commonly ask about neuropathy because:
- Diabetes is common, and long-term high blood sugar can injure nerves over time (Mayo Clinic, 2023).
- Neuropathy symptoms can feel scary (burning, numbness, weakness), and they can interfere with work, sleep, and walking.
- Many people want options beyond medication, like rehab, lifestyle support, and non-invasive care.
Local and regional sources also emphasize symptoms such as burning, throbbing, tingling, and numbness as common concerns that prompt people to seek evaluation. (El Paso Pain Center, n.d.).
FAQ 1: What symptoms should I watch for?
Neuropathy symptoms can vary, but common ones include:
- Tingling (“pins and needles”)
- Burning or sharp pain (often worse at night)
- Numbness or reduced ability to feel temperature or pain
- Sensitivity to touch
- Muscle cramping or weakness
- Balance trouble or feeling unsteady
Some people also notice autonomic symptoms, such as abnormal sweating, bowel changes, or sexual dysfunction. (Frontier Neurology, n.d.; Mayo Clinic, n.d.).
Why this matters: when you can’t feel pain normally, you may not notice injuries—especially on the feet. That can raise the risk of blisters, wounds, and infections. (ANESC, n.d.).
FAQ 2: Is neuropathy always caused by diabetes?
No. Diabetes is a leading cause, but it’s not the only cause.
Other common causes include:
- Vitamin deficiencies (especially B12)
- Alcohol-related nerve damage
- Certain medications (including some chemotherapy drugs)
- Infections, autoimmune conditions, or inflammation
- Injuries or nerve entrapment (compression)
- Metabolic or hormonal issues
- Vascular (circulation) issues
(Mayo Clinic, 2023; iVascular Center, n.d.).
Screening resources often highlight diabetes risk, but also mention nutrient deficiencies and other contributors that should be checked. (Medicos Family Clinic, 2025).
FAQ 3: How do I know if my symptoms are neuropathy or something else?
Neuropathy can overlap with other problems, such as:
- Radiculopathy (“pinched nerve”) from the neck or low back
- Carpal tunnel or tarsal tunnel syndrome
- Peripheral artery disease (PAD) or circulation issues
- Musculoskeletal problems that mimic nerve pain
- Medication side effects
That’s why a proper evaluation usually includes:
- A detailed symptom history (when it started, what makes it better/worse)
- A neuro exam (reflexes, sensation, strength)
- Gait and balance checks
- Foot/skin checks (especially if diabetes is present)
Many clinics also use targeted testing when needed (see below). (Cleveland Clinic, n.d.; Mayo Clinic, 2023).
FAQ 4: What tests diagnose neuropathy?
Diagnosis often starts with history + exam, and then testing is chosen based on your risk factors and symptoms.
Common tests include:
- Blood work (often to check diabetes control, B12, thyroid, inflammation, etc.)
- EMG/NCS (nerve conduction study + electromyography) to evaluate how nerves and muscles are functioning (useful in many neuropathy evaluations)
- Imaging (like MRI) if a spine or nerve-root problem is suspected
Electrodiagnostic testing (NCS/EMG) can support the diagnosis of peripheral neuropathy and help clarify patterns of nerve involvement. (Novello, 2023).
FAQ 5: What are “red flags” that mean I should seek urgent care?
Seek urgent medical evaluation if you have:
- Sudden, fast-worsening weakness
- New loss of bladder or bowel control
- Severe balance loss with repeated falls
- A rapidly spreading numb area
- A foot wound that looks infected (redness, swelling, warmth, drainage), especially with diabetes
- Chest pain, fainting, or severe dizziness (could be more than neuropathy)
Neuropathy can reduce sensation and raise injury risk, so foot wounds should be taken seriously. (ANESC, n.d.).
FAQ 6: If I have diabetes, what should I do first?
If diabetes is part of your story, first steps usually focus on nerve protection and risk reduction:
- Improve glucose management with your medical team
- Check feet daily (look for cuts, blisters, redness)
- Wear supportive footwear and avoid walking barefoot
- Address sleep, stress, and movement habits
- Treat pain, but also work on function (balance, strength, gait)
Diabetes is one of the most common causes of neuropathy, so controlling the underlying driver can help slow progression. (Mayo Clinic, 2023).
FAQ 7: What treatments exist beyond medications?
Many people in El Paso ask for options beyond “just meds.” A realistic plan often uses multiple layers, depending on the cause and severity.
Common non-medication options include:
- Physical therapy to improve strength, balance, gait, and safety with movement (P3 Physical Therapy, n.d.).
- Lifestyle trigger control (for example: reducing prolonged sitting/standing, improving footwear, and avoiding habits that worsen symptoms) (Modern Pain Management Clinic, n.d.).
- Foot care + specialized care (especially for diabetic foot risks) (ANESC, n.d.; El Paso Feet, n.d.).
- Laser therapy is discussed by local podiatry sources as an option used for diabetic foot-related pain conditions, including diabetic neuropathy (El Paso Feet, 2024).
- Interventional pain options, when appropriate (examples include nerve-focused procedures and other pain interventions discussed by local pain clinics) (El Paso Pain Center, n.d.).
- Neuromodulation options such as peripheral nerve stimulation (PNS), which uses mild electrical impulses to disrupt pain signaling in specific nerves (Donya Pain and Wellness Center, n.d.).
FAQ 8: Can chiropractic care help neuropathy?
Chiropractic care is not described as a “cure” for neuropathy in many clinical education resources, but it is often presented as a supportive, conservative approach that can help some people manage symptoms and improve movement, especially when nerve irritation is linked with mechanical stress, posture, or joint dysfunction. (Pain & Wellness Institute, n.d.).
Some chiropractic education pages describe goals like:
- Reducing mechanical pressure on sensitive areas
- Improving mobility and function
- Supporting circulation and movement quality
- Adding home exercises and soft-tissue work as part of a plan
(Leicester Spine & Wellness, 2025; Pain & Wellness Institute, n.d.).
Important note: neuropathy has many causes. Chiropractic care makes the most sense when it is part of a broader plan that also addresses medical causes (such as diabetes control, B12 deficiency, medication side effects, and circulation issues).
FAQ 9: What does “integrative chiropractic therapy + NP care” look like in real life?
This is where many El Paso patients feel they finally get clarity: a plan that addresses both the medical and functional sides.
A practical integrative model often includes:
- Nurse practitioner (NP) evaluation
- Reviews health history, medications, and risk factors
- Orders/coordinates labs and referrals when needed
- Screens for diabetes, vitamin deficiencies, thyroid issues, and other contributors
- Builds a step-by-step plan for lifestyle, nutrition, and symptom control
- Chiropractic and rehab-focused care
- Movement and posture assessment
- Gentle joint/spine techniques, when appropriate.
- Soft tissue work + mobility work
- Exercises for balance, gait, and functional strength
Dr. Alexander Jimenez, DC, APRN, FNP-BC describes a “dual-scope” approach—blending chiropractic assessment with medical-style evaluation—often including careful history, posture/mobility testing, and imaging when needed, and then combining conservative therapies (like rehab and other integrative strategies) based on the patient’s risks and goals. (Jimenez, n.d.-a).
He also discusses broader neuropathy management strategies, including lifestyle adjustments, injury prevention, and coordinated care with other providers when needed. (Jimenez, n.d.-b).
FAQ 10: What can I do at home to protect my nerves and function?
Here are practical steps many clinicians recommend (and that match what many neuropathy resources emphasize):
Daily safety and symptom control
- Check your feet daily (especially if you have numbness)
- Use supportive shoes; avoid tight footwear
- Keep skin moisturized and watch for cracks or wounds
- Avoid extreme heat on numb areas (heating pads can burn skin you can’t feel well)
Loss of sensation can raise injury risk, especially in the feet. (ANESC, n.d.).
Movement and function support
- Walk as tolerated (even short walks can help circulation and mobility)
- Do balance and strength work (a PT can tailor this)
- Build leg and core strength to reduce fall risk
Physical therapy clinics in El Paso commonly emphasize addressing nerve pain with movement-based strategies and individualized plans. (P3 Physical Therapy, n.d.).
Lifestyle triggers to reduce
- Limit prolonged standing or sitting if it flares symptoms
- Improve workstation ergonomics and posture
- Use footwear that doesn’t compress the toes and forefoot
(Modern Pain Management Clinic, n.d.).
FAQ 11: What local care options exist in El Paso?
People often want to know, “Who can help me here—without me bouncing around forever?”
Depending on your needs, El Paso-area resources commonly include:
- Neurology evaluation for complex neuropathy patterns or autonomic symptoms (Frontier Neurology, n.d.).
- Pain management clinics for neuropathic pain procedures and broader pain strategies (El Paso Pain Center, n.d.).
- Physical therapy for balance, gait, strength, and functional rehab (P3 Physical Therapy, n.d.).
- Podiatry/foot-focused care for diabetic foot protection, and options like laser therapy, which some clinics discuss for diabetic neuropathy support (El Paso Feet, 2024).
- Peripheral nerve stimulation (PNS) for selected chronic pain cases (Donya Pain and Wellness Center, n.d.).
A strong plan often uses the right mix of these services, based on your cause, your exam findings, and how the symptoms affect your life.
FAQ 12: Are support groups and community resources worth it?
Yes—especially for chronic symptoms. Support groups can reduce isolation, improve coping skills, and help people learn practical strategies from others living with neuropathy.
The Foundation for Peripheral Neuropathy lists virtual and in-person support group resources and guidance for people living with peripheral neuropathy. (Foundation for Peripheral Neuropathy, n.d.).
A simple “next-step” plan (what many clinicians would do first)
If you want a clear path forward, here’s a practical sequence:
- Step 1: Confirm the pattern
- Where is it? Feet only? Hands too? One side? Both?
- Numbness only, or burning pain + weakness?
- Step 2: Screen common drivers
- Diabetes and glucose control
- B12 and other nutrients
- Medication review
- Circulation and foot risk checks
(Mayo Clinic, 2023; Medicos Family Clinic, 2025).
- Step 3: Test when needed
- EMG/NCS for unclear cases or when weakness is present
(Novello, 2023).
- EMG/NCS for unclear cases or when weakness is present
- Step 4: Treat for function (not just pain)
- PT for balance/strength/gait
- Foot care protection
- Conservative integrative care (chiropractic + rehab + lifestyle coaching)
- Interventional options when appropriate
(P3 Physical Therapy, n.d.; Pain & Wellness Institute, n.d.).
Safety note and medical disclaimer
This article is for education only and is not personal medical advice. Neuropathy can have multiple causes, and some require urgent treatment. If you have rapidly worsening symptoms, major weakness, new bowel/bladder issues, or a serious foot wound—seek urgent medical care.
References
- ANESC. (n.d.). Neuropathy.
- Cleveland Clinic. (n.d.). Peripheral neuropathy.
- Donya Pain and Wellness Center. (n.d.). Peripheral nerve stimulator (PNS) in El Paso, TX.
- El Paso Pain Center. (n.d.). Sharp, throbbing, burning pain?.
- El Paso Feet. (2024). Laser therapy for diabetic neuropathy.
- Foundation for Peripheral Neuropathy. (n.d.). Support groups.
- Foundation for Peripheral Neuropathy. (n.d.). Help for the newly diagnosed.
- Frontier Neurology. (n.d.). Neuropathy.
- iVascular Center. (n.d.). Peripheral neuropathy.
- Jimenez, A. (n.d.-a). Safe chiropractic care in El Paso: What to expect.
- Jimenez, A. (n.d.-b). Managing peripheral neuropathy: Effective treatment strategies.
- Mayo Clinic. (2023). Peripheral neuropathy: Symptoms and causes.
- Mayo Clinic. (n.d.). Autonomic neuropathy: Symptoms and causes.
- Medicos Family Clinic. (2025). Understanding neuropathy screening.
- Modern Pain Management Clinic. (n.d.). 5 triggers of neuropathy and how to get relief.
- Novello, B. J. (2023). Electrodiagnostic evaluation of peripheral neuropathy.
- Pain & Wellness Institute. (n.d.). Can chiropractic care help my neuropathy?.
- P3 Physical Therapy. (n.d.). Nerve damage.
Post Disclaimer
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Neuropathy in El Paso, TX: Frequently Asked Questions" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and facilitate clinical collaboration with specialists across disciplines. Each specialist is governed by their professional scope of practice and licensure jurisdiction. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRN: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card

