Chiropractic and Nurse Practitioner for Injury Recovery
What advantages does possessing dual licensure as a chiropractor and nurse practitioner confer in personal injury lawsuits and automobile accidents?

Chiropractic and Nurse Practitioner On Auto Accidents
Following a motor vehicle collision, chiropractors and nurse practitioners are essential in injury management and recovery facilitation. Chiropractors emphasize manual therapies, including adjustments and manipulations, to resolve musculoskeletal problems and enhance mobility, whereas nurse practitioners deliver comprehensive care encompassing assessments, diagnoses, treatment plans, and education, frequently collaborating with specialists to maximize patient outcomes. (Physicians Group, LLC. 2024)
Chiropractors
Chiropractors address musculoskeletal problems, including back and neck discomfort, frequently resulting from automobile accidents. They employ tactile methods to alleviate discomfort and enhance mobility, frequently without pharmaceuticals. Comprehensive data and expert testimony can substantiate personal injury claims, demonstrating the severity of injuries. (Dies, S., & Strapp, J. W., 1992)
Assessment and Management of Musculoskeletal Disorders
- Chiropractors can diagnose and treat spinal misalignments, muscle spasms, and soft tissue injuries that may occur following an accident.
Analgesic Relief
- Manual therapy, such as spine adjustments and soft tissue mobilization, can mitigate pain and diminish inflammation.
Enhanced Mobility
- Chiropractors can restore range of motion and enhance overall function by correcting joint and muscle limitations.
Comprehensive Care
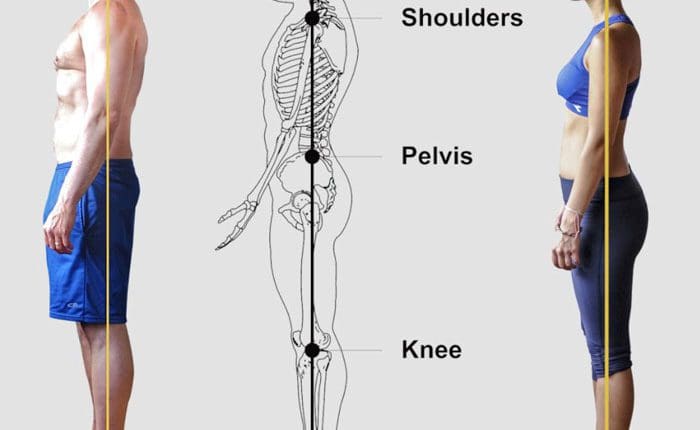
- Chiropractors typically emphasize holistic body care and guide sustaining proper posture, ergonomics, and general wellness to avert future injuries.
Cooperation with Additional Healthcare Practitioners
- Chiropractors can collaborate with physicians, physical therapists, and other professionals to develop a holistic treatment plan for the patient. (Physicians Group, LLC, 2024)
Nurse Practitioners
Nurse practitioners are capable of delivering comprehensive care for injuries resulting from motor vehicle accidents, encompassing (Integrity Spine & Orthopedics, 2024)
Evaluation and Identification
- Nurse practitioners are capable of performing physical examinations, interpreting diagnostic tests, and diagnosing conditions such as whiplash, soft tissue injuries, and concussions.
Therapeutic Protocols
- They can develop individualized treatment regimens, encompassing pharmacological therapies, physical rehabilitation, and additional interventions, to meet the patient’s distinct requirements.
Patient Instruction
- Nurse practitioners can instruct patients regarding their injuries, the recuperation process, and self-care techniques to facilitate healing and avert complications.
Care Coordination
- They can collaborate with other professionals, including surgeons, neurologists, and physical therapists, to guarantee a comprehensive approach to treatment.
Post-Treatment Care
- Nurse practitioners can assess the patient’s progress, modify treatment plans as necessary, and offer continuous care during the healing process.
Personal injury cases, especially those resulting from automobile collisions, frequently entail intricate medical and legal requirements. Chiropractors and nurse practitioners, each with unique scopes of practice, are essential in diagnosis, treatment, and documentation.
Chiropractors and nurse practitioners both contribute distinct advantages to personal injury cases. Chiropractors concentrate on musculoskeletal disorders, providing non-invasive therapies, whereas nurse practitioners address a wider range of medical requirements, including the prescription of drugs and the coordination of care. Their collaboration can improve patient results, as demonstrated in environments such as the Accident Treatment and Treatment Center, where nurse practitioners and physicians oversee treatment, augmenting chiropractic interventions. (Accident Care, 2025)
Legal resources indicate that the documentation of both professions is essential for insurance claims and settlements. Chiropractors’ meticulous reports on spinal injuries and nurse practitioners’ extensive medical records on overall health can collectively establish a compelling case for compensation. This synergy is especially apparent in automobile accident situations, where patients may necessitate both physical changes and medical supervision for complete recovery. (Chiropractic Economics, 2023)
Injury Medical Chiropractic and Functional Medicine Clinic
Dr. Jimenez, a family practice nurse practitioner, integrates advanced medical knowledge with chiropractic treatment to manage diverse illnesses. Our clinic amalgamates functional medicine, acupuncture, electro-acupuncture, and sports medicine to design tailored care regimens that foster natural healing, enhance mobility, and ensure long-term wellness. By emphasizing flexibility, agility, and strength, we enable patients to flourish, irrespective of age or health obstacles. At El Paso’s Chiropractic Rehabilitation Clinic & Integrated Medicine Center, we are dedicated to treating individuals following injuries and chronic pain disorders. We concentrate on enhancing your capabilities through customized flexibility, mobility, and agility training designed for various age demographics and disabilities. We employ both in-person and virtual health coaching, together with comprehensive care plans, to guarantee tailored care and wellness outcomes for each patient.
Don’t Ignore Your Post-Accident Pain
References
Physicians Group, LLC. (2024). The Role of Nurse Practitioners in Managing Auto Injuries. Physicians Group, LLC. https://physiciansgroupllc.com/the-role-of-nurse-practitioners-in-managing-auto-injuries/#:~:text=Nurse%20Practitioners%20are%20vital%20in,improved%20outcomes%20and%20patient%20satisfaction.
Dies, S., & Strapp, J. W. (1992). Chiropractic treatment of patients in motor vehicle accidents: a statistical analysis. The Journal of the Canadian Chiropractic Association, 36(3), 139–145.
The Neck and Back Clinics. (2025). Why Seeing a Chiropractor After a Car Accident Is Crucial for Long-Term Recovery. https://theneckandbackclinics.com/long-term-recovery/#:~:text=Reducing%20Inflammation%20and%20Pain,each%20patient%20for%20optimal%20recovery.
Integrity Spine & Orthopedics. (2024). The 9 Steps to Recovery After an Auto Accident. https://www.integrityspineortho.com/post/the-9-steps-to-recovery-after-an-auto-accident/#:~:text=CONTACT%20INTEGRITY%20SPINE%20AND%20ORTHOPEDICS%20AFTER%20A,concussions%2C%20soft%20tissue%20damage%20and%20spine%20damage.
Accident Care and Treatment Center, Inc. (2025). Comprehensive Therapies and Treatments in One Location. https://accidentcare.com/treatment/
Chiropractic Economics. (2023). Evidence-based chiropractic: the key to personal-injury cases. https://www.chiroeco.com/evidence-based-chiropractic-the-key-to-personal-injury-cases/