An Overview of Somatovisceral Disorders & Head Injuries
Discover the connection between head injuries and somatovisceral disorders to enhance patient care and management.
Understanding Head Injuries and Their Impact on the Brain-Body Connection: A Comprehensive Guide to Somatovisceral Disorders and Non-Surgical Treatment Approaches
Millions of people worldwide are impacted by head injuries every year, making them a serious public health problem. The harm that results from head trauma, whether from a fall, auto accident, or sports collision, goes much beyond the location of the original hit. Researchers now identify somatovisceral illnesses as a result of these injuries, which cause a series of physiological alterations that interfere with the delicate brain-body communication system. Recovery outcomes and quality of life may be significantly improved by understanding how head trauma impacts this crucial brain-body link and by investigating effective non-surgical therapeutic options.
What Are Somatovisceral Disorders?
Complex connections between the body’s internal organs (visceral system) and physical structures (somatic system) are a feature of somatovisceral illnesses. Nerve impulses from body structures are transmitted to visceral organs through this complex process, resulting in specific physiological or pathological responses. In addition to involving two systems, the somatovisceral response is complicated because it may communicate in both directions, transferring information from somatic structures to visceral organs and vice versa. foundationhealth
Medical studies have focused more on the connection between somatovisceral diseases and brain trauma. According to a recent study, 15–27% of patients who had head trauma fulfilled the criteria for somatic symptom disorder six months after the injury, suggesting that mild traumatic brain injury (mTBI) may be a frequent precursor to this syndrome. This link demonstrates how brain damage may disrupt the normal communication pathways that control physiological processes, leading to chronic, often incapacitating symptoms throughout the body. neurologyopen.bmj
When people have upsetting physical symptoms together with excessive thoughts, emotions, or actions associated with those symptoms, it’s known as somatic symptom disorder. Many somatic problems, such as pain, weakness, difficulty moving, headaches, dizziness, excessive fatigue, changes in vision or hearing, itching, numbness, odd movements, stomach pain, and nausea, are often reported by patients after a brain injury. These symptoms illustrate how neurological impairment may materialize as pervasive physical dysfunction by reflecting the disturbed connection between the brain and many bodily systems. chop+1
The Brain-Body Connection and Head Injury
The human nervous system operates through an intricate network that connects the brain to every organ, muscle, and tissue in the body. This communication highway relies on precise signaling between the central nervous system (brain and spinal cord) and the peripheral nervous system (nerves throughout the body). When head trauma occurs, this delicate communication system can become disrupted at multiple levels, affecting both somatic (voluntary) and autonomic (involuntary) nervous system functions.
According to Dr. Alexander Jimenez, a board-certified Family Practice Nurse Practitioner and Doctor of Chiropractic in El Paso, Texas, the spine houses the spinal cord, which acts as the communication superhighway between the brain and body. Any misalignment in the spine can disrupt the nervous system’s signals, and for traumatic brain injury patients, this connection becomes crucial. Dr. Jimenez explains that misalignment caused by the injury itself or associated whiplash can worsen symptoms like headaches, brain fog, and balance issues, emphasizing the importance of addressing both cranial and spinal components in recovery. northwestfloridaphysiciansgroup
The brain-body disconnect following trauma manifests as disrupted somatic sensory processing, encompassing vestibular (balance) and somatosensory (touch, pressure, temperature) processing. These sensory systems are primarily concerned with survival and safety, given the potential consequences of impaired balance or diminished awareness of physical threats. Following a head injury, trauma-related symptoms are conceptualized to be grounded in brainstem-level somatic sensory processing dysfunction and its cascading influences on physiological arousal modulation, affect regulation, and higher-order capacities. pmc.ncbi.nlm.nih
Research has identified that traumatic conditions may manifest as disrupted vertical integration, in which the balance between lower brain regions and higher cortical areas becomes dysregulated, particularly within the midline neural circuitry responsible for generating a primordial sense of a bodily and affective self as a coherent and stable entity in relation to the environment. This alteration has a cascading impact on the horizontal integration of cortical brain structures, meaning that different regions of the brain may be structurally intact yet lack fluid communication. pmc.ncbi.nlm.nih
Autonomic Dysfunction After Head Injury
One of the most significant yet underappreciated consequences of head injury is autonomic nervous system dysfunction. The autonomic nervous system controls involuntary bodily functions, including heart rate, blood pressure, digestion, breathing, and temperature regulation. Following moderate-to-severe traumatic brain injury, patients often experience significant autonomic dysfunction affecting both sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) branches of this critical system. neurologyopen.bmj
Studies have demonstrated that patients with severe traumatic brain injury can experience sympathetic hyperactivity in the acute stages. More importantly, autonomic dysfunction persists in many patients for months or even years after their initial injury, affecting fully ambulant patients whom many might assume to be fully recovered. This persistent dysfunction occurs through various mechanisms, with the hallmark of moderate-to-severe traumatic brain injury being white matter injury caused by axonal shearing due to injury forces, continuing due to inflammation and delayed axonal degeneration in the chronic period, resulting in network disruption. neurologyopen.bmj
Autonomic dysfunction may occur due to injury to regions of the central autonomic network or their connecting white matter tracts. Brainstem nuclei and white matter connections to and from thalamic and basal ganglia regions may be particularly vulnerable to damage, underlying dysfunction that contributes to cognitive impairment post-traumatic brain injury. Given the importance of brainstem, thalamic, and basal ganglia circuits to autonomic function, injury to these white matter tracts may cause centrally mediated autonomic dysfunction. neurologyopen.bmj
The clinical manifestations of autonomic dysfunction after head injury are diverse and often debilitating. Many classic symptoms following concussion are, at least in part, likely a result of injury to the autonomic nervous system. Cognitive difficulties seen after mild traumatic brain injury may be related to autonomic dysregulation, specifically impaired cerebral blood flow. The presence of autonomic dysfunction has been shown to correlate with increased morbidity and mortality in moderate and severe traumatic brain injury, with perturbations of the autonomic nervous system consisting of either increased sympathetic or reduced vagal activity, potentially resulting in serious cardiac complications. health+1
Dr. Jimenez’s clinical practice emphasizes the importance of recognizing autonomic dysfunction in patients recovering from head injuries. His functional medicine approach includes detailed health assessments evaluating lifestyle, environmental exposures, and psychological factors to understand the root causes of chronic disorders and treat patients holistically. This comprehensive evaluation is particularly important for identifying autonomic dysfunction, which may manifest as dizziness, balance problems, temperature dysregulation, digestive issues, and cardiovascular irregularities.
Environmental Factors Affecting Brain Activity and the Body
Environmental factors play a critical role in shaping brain structure and function, as well as the development of mental and physical health conditions. The macroenvironment encompasses immediate factors such as air, noise, and light pollution; proximal factors, including regional socioeconomic characteristics; and distal factors, such as urbanization, natural spaces, and climate. These environmental exposures are mostly modifiable, presenting opportunities for interventions and strategies to promote the structural and functional integrity of the brain and mitigate the burden of illness following head injury. nature
- Air pollution has emerged as a significant concern for brain health, particularly following traumatic brain injury, when the brain is already vulnerable. Studies have demonstrated that air pollution may increase vulnerability to mood dysfunction and potentially inhibit an appropriate stress response. Prolonged exposure to fine particulate matter (PM2.5 and PM10) has been associated with negative stress-related brain activation in the prefrontal cortex, frontoinsular cortex, limbic system, inferior parietal cortex, and cingulate regions. Magnetic resonance imaging studies reveal that increased exposure to PM2.5 is associated with changes in brain structure in older adults, including brain atrophy, that occur before the onset of dementia. environmentalhealth.ucdavis+1
- Noise pollution, originating from urban traffic, airports, industries, and construction sites, can evoke negative emotions and disrupt recovery following head injury. Prolonged exposure to disruptive noise induces brain alterations through mechanisms such as sleep disturbances, which create a pro-oxidative environment that predisposes to neuroinflammation and heightened hypothalamic-pituitary-adrenal axis reactivity, contributing to mental and physical health problems. For individuals recovering from head trauma, protecting against excessive noise exposure becomes particularly important as the injured brain requires optimal conditions for healing. nature
- Light pollution and exposure to artificial light at night have become increasingly prevalent, especially in urban areas, disrupting natural darkness and circadian rhythms. Light is detected by the retina and transmitted through intrinsically photosensitive retinal ganglion cells to the suprachiasmatic nucleus in the hypothalamus and other brain regions involved in regulating circadian rhythms and sleep-wake cycles. Circadian rhythm disruptions have been linked to elevated risk of mood disorders, bipolar disorders, and heightened mood instability, potentially mediated by oscillations in clock gene expression responsive to light-dark transitions. nature
- Following traumatic brain injury, circadian rhythm disruptions become even more pronounced. Research has documented that traumatic brain injury can lead to decreased melatonin release, causing circadian rhythm delays. Studies using animal models have revealed that acute subdural hematoma resulted in dysregulation of circadian gene expression and rhythmic changes in body temperature during the first 48 hours post-injury. The regulation of biological rhythms through changes in core body temperature, pineal gland melatonin secretion, and blood cortisol levels becomes disrupted, affecting the body’s ability to anticipate and adapt to environmental changes. practicalneurology+1
Minor traumatic brain injury contributes to the emergence of circadian rhythm sleep disorders, with research identifying two distinct types: delayed sleep phase syndrome and irregular sleep-wake pattern. These disorders differ in subjective questionnaire scores and have distinct profiles of melatonin and temperature circadian rhythms. The alteration in the circadian timing system partially accounts for the presence of post-traumatic brain injury sleep-wake disturbances, which changes in sleep architecture alone cannot fully explain. pubmed.ncbi.nlm.nih+1
Understanding Long-Lasting Injuries- Video
How Head Injuries Affect Daily Tasks and Routines
The impact of head injuries extends far beyond the initial trauma, profoundly affecting an individual’s ability to perform everyday activities and maintain normal routines. The disruption to brain-body communication creates challenges across multiple domains of daily functioning, from basic self-care tasks to complex cognitive and social activities. Understanding these impacts helps patients, families, and healthcare providers develop realistic expectations and appropriate support strategies during recovery.
- Cognitive fatigue represents one of the most disabling consequences of traumatic brain injury, affecting 21-73% of patients regardless of injury severity or time since injury. Fatigue has been identified as the main cause of disability after traumatic brain injury, negatively affecting social, physical, and cognitive functions as well as participation in daily activities and social life. At the neural level, patients with fatigue following head injury exhibit significant disruption of global resting-state alpha-band functional connectivity between cortical midline structures and the rest of the brain. Furthermore, individuals with fatigue show reduced overall brain activation during cognitive tasks, without time-on-task effects. academic.oup
- Adults with a history of even mild traumatic brain injury report significantly greater fatigue and cognitive impairment than those with no history of head trauma, with symptoms becoming more profound with greater injury severity. This persistent fatigue affects the ability to maintain attention, concentrate on tasks, process information efficiently, and sustain mental effort throughout the day. Patients frequently report that activities requiring cognitive engagement become increasingly difficult as the day progresses, leading to a pattern of morning productivity followed by afternoon exhaustion. pubmed.ncbi.nlm.nih+1
- Memory difficulties present another significant challenge affecting daily functioning after a head injury. Patients may struggle with both short-term working memory (holding information in mind while using it) and long-term memory formation (creating new lasting memories). These memory challenges affect practical tasks such as remembering appointments, following multi-step instructions, recalling conversations, and learning new information or skills. The impact extends to occupational functioning, with studies finding a correlation between higher levels of mental fatigue and lower employment status following traumatic brain injury. headway+1
- Executive function impairments following head injury affect planning, organization, decision-making, problem-solving, and behavioral regulation. These higher-order cognitive processes are essential for managing daily responsibilities, from planning meals and organizing household tasks to managing finances and making important life decisions. Patients may find themselves struggling with tasks that previously seemed automatic, requiring conscious effort and external supports to maintain daily routines. headway
- Sensory processing alterations create additional challenges for daily functioning. The vestibular system, which contributes to balance, spatial processing, arousal modulation, first-person perspective, and social cognition, becomes particularly vulnerable following head trauma. Disturbed temporal binding of sensory information creates perceptual chaos and lack of coherence, which may lead to bodily disconnect and states of hypervigilance. Patients describe feeling disconnected from their bodies, experiencing the world as if through a fog, or feeling constantly on guard against potential threats. pmc.ncbi.nlm.nih
- Balance and coordination problems stemming from vestibular dysfunction affect mobility and safety in daily activities. Simple tasks like walking on uneven surfaces, turning the head while moving, or navigating busy environments become challenging and potentially dangerous. Many patients report increased anxiety about falling, leading to activity restriction and social withdrawal. Over one-third of adults over 40 will experience vestibular dysfunction at some point in their lives, and when it occurs, whether by injury, aging, or disease, individuals can experience vertigo, nauseating dizziness, vision and balance problems affecting every area of life. neuroinjurycare+1
Dr. Jimenez’s practice in El Paso focuses extensively on helping patients restore function and return to daily activities following head injuries. His integrated approach combines chiropractic care, functional medicine, and rehabilitation therapies to address the multiple systems affected by head trauma. By evaluating the connections between physical, nutritional, and emotional factors, Dr. Jimenez develops personalized care plans that recognize the complex ways head injuries disrupt daily functioning and quality of life.
Overlapping Risk Profiles and Symptoms Associated With Head Injuries
Head injuries create overlapping risk profiles affecting multiple body systems simultaneously, leading to complex symptom presentations that can challenge both patients and healthcare providers. Understanding these interconnected risk factors and symptoms is essential for comprehensive assessment and treatment planning. Individuals who sustain head injuries develop an increased risk for somatic symptom disorder, with early illness beliefs playing a significant predictive role. Specifically, believing that mild traumatic brain injury has serious life consequences and causes distress in the weeks following injury is associated with later development of somatic symptom disorder. Patients with somatic symptom disorder after head injury report more pain and post-concussion symptoms and are significantly more likely to have comorbid major depressive disorder and anxiety disorders compared to those without this condition. neurologyopen.bmj
- The systematic review examining the relationship between somatic symptoms and related disorders and mild traumatic brain injury found that the majority of acceptable evidence supported a relationship between these conditions. Nine studies reported associations between functional seizures and a history of mild traumatic brain injury, while 31 studies assessed relationships between questionnaires measuring somatic symptom disorder burden and mild traumatic brain injury. Three studies investigated healthcare practitioners’ diagnosis of somatic symptoms and related disorders and post-mild traumatic brain injury symptom burden, collectively demonstrating the strong connection between head trauma and subsequent development of somatic complaints. foundationhealth
- Cardiovascular complications represent another significant overlapping risk following head injury. Research demonstrates that individuals with moderate-to-severe traumatic brain injury have increased rates of self-reported hypertension and stroke but lower rates of myocardial infarction and congestive heart failure than uninjured adults. The findings highlight the importance of early screening for and management of cardiovascular risk factors in individuals with chronic traumatic brain injury, particularly those of younger age, not typically thought to be at risk for these conditions. ahajournals
- The relationship between blood pressure and traumatic brain injury follows a complex U-shaped pattern, with both hypotension and hypertension associated with worse outcomes. Early hypotension has been linked with poor outcomes following severe traumatic brain injury, but recent data suggest that arterial hypertension after injury is also associated with poor outcomes. The initial catecholamine response and resulting systemic hypertension may be protective to a point by maintaining cerebral perfusion pressure in the setting of impaired cerebral autoregulation after injury, yet catecholamine-induced hypertension may also cause secondary brain damage by aggravation of vasogenic edema and intracranial hypertension. pmc.ncbi.nlm.nih
- Post-traumatic headaches affect approximately 40% of individuals who experience concussions, representing one of the most common and persistent symptoms following head injury. Patients can experience tension headaches, migraine headaches, and cervicogenic headaches (radiating from the neck) all at once, making treatment particularly challenging. Ninety-five percent of people with a concussion experience headache associated with that injury, and among those with headache, about two-thirds have migraine features. Individuals with a family history of migraine or preexisting headache disorders face a higher risk of developing post-traumatic headache. wexnermedical.osu+1
- Sleep disturbances cluster with other post-traumatic brain injury symptoms, creating compounding difficulties for recovery. Changes in sleep architecture following injury cannot fully explain the extent and intensity of sleep-wake disturbances reported by patients. The current literature supports cognitive-behavioral therapy and sleep hygiene education, light therapy, and certain pharmacologic interventions for treating sleep disturbances in patients with brain injury, with early screening and individualized approaches prioritized to improve sleep and, consequently, speed recovery. pubmed.ncbi.nlm.nih
- Exercise intolerance commonly results from a concussion, often limiting return to activities and quality of life. The reviewed studies support clinical suspicion of autonomic dysfunction as an important component of exercise intolerance, though specific mechanisms of impairment and relationships to symptoms and recovery require additional investigation. Post-concussive exercise intolerance has been linked to a reduction in cerebral blood flow, theoretically prolonging the effects of the metabolic energy crisis associated with injury. pmc.ncbi.nlm.nih
- Mental health complications, including anxiety, depression, post-traumatic stress disorder, and behavioral changes, frequently develop following head injury. Brain injuries, no matter how severe, commonly cause emotional and behavioral changes, including emotional lability with extreme mood swings, anxiety disorders, depression, impulsive behaviors, flat affect causing a lack of emotional expression, and a lack of empathy and social skills. These psychological changes can cause unnecessary suffering and, in cases of severe depression and anxiety, can even halt physical recovery progress. flintrehab
Non-Surgical Treatments to Improve Somatovisceral Function
Fortunately, numerous non-surgical treatment approaches have demonstrated effectiveness in improving somatovisceral function and promoting recovery following head injuries. These interventions work through various mechanisms to restore proper communication between the brain and the body, balance the autonomic nervous system, and support the brain’s natural healing processes. Dr. Jimenez’s clinical practice emphasizes comprehensive non-invasive protocols, prioritizing natural recovery and avoiding unnecessary surgeries or medications.
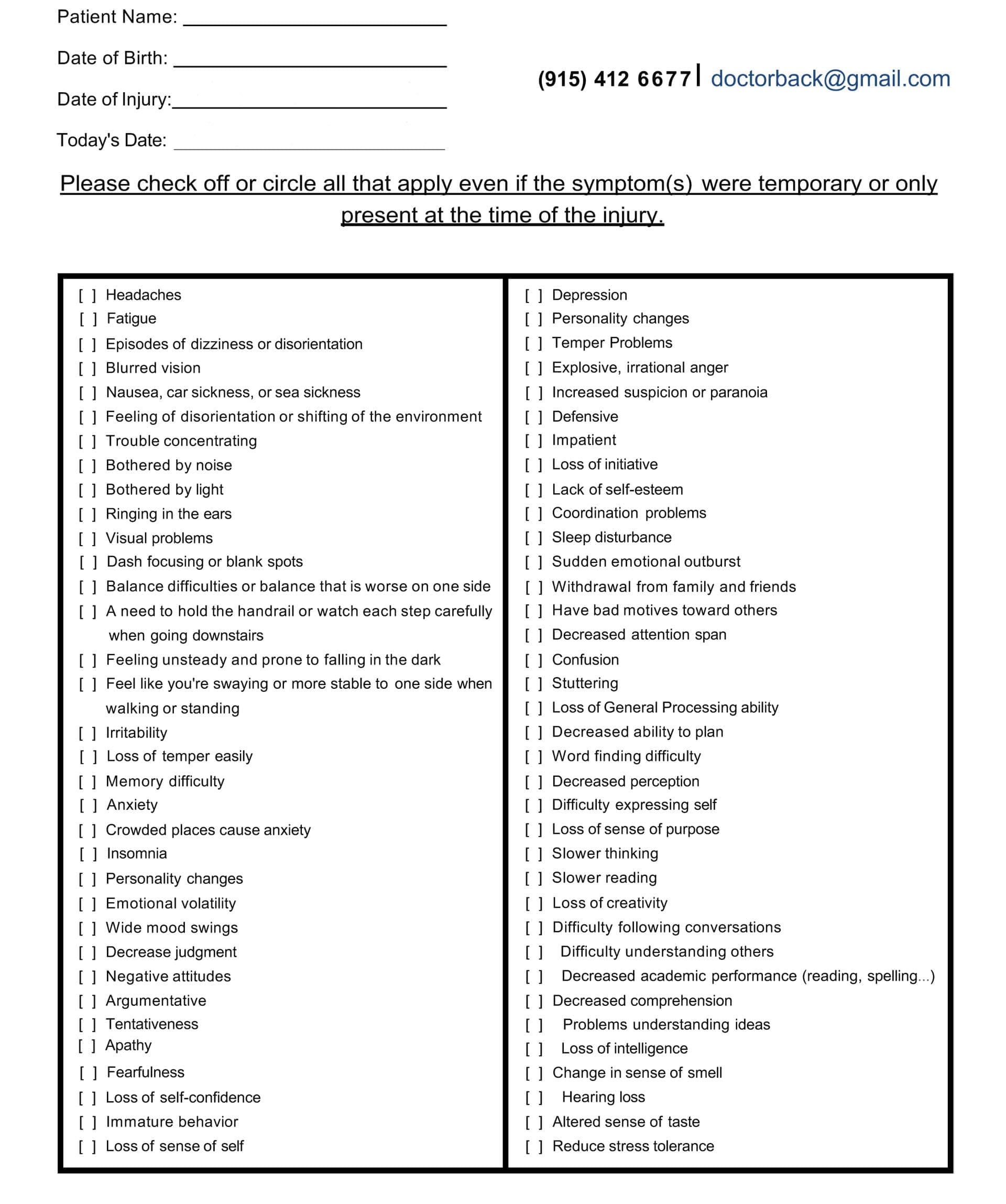
A Questionnaire Example of TBI Symptoms

Chiropractic Care and Spinal Adjustments
Chiropractic care focuses on the spine and nervous system, recognizing that the spine houses the spinal cord, which acts as the communication superhighway between the brain and body. For traumatic brain injury patients, proper spinal alignment becomes crucial because misalignment caused by the injury itself or associated whiplash can worsen symptoms like headaches, brain fog, and balance issues. Chiropractic care aims to restore proper alignment, thereby improving nervous system function and supporting the brain’s ability to heal. northwestfloridaphysiciansgroup Chiropractic adjustments help alleviate post-traumatic brain injury symptoms by releasing pressure on irritated nerves and improving joint function. For many patients, this results in improved comfort and reduced reliance on pain medication. Proper spinal alignment promotes better blood flow to the brain, and since the brain requires oxygen-rich blood to heal and function, improved circulation directly supports recovery from traumatic brain injury while reducing dizziness and fatigue. northwestfloridaphysiciansgroup
Research demonstrates that chiropractic intervention can modify proprioceptive input from more functional spinal joints, helping restore this input to the brain’s multisensory integration centers. Studies of patients receiving chiropractic care in neurorehabilitation hospitals have shown that spinal manipulation influences pain through complex mechanisms in the central nervous system. A case study documenting concussion treatment using massage and manipulation techniques showed diminished concussion symptoms and regained ease in cervical range of motion, highlighting the potential importance of manual therapy work to reduce headache, dizziness, and nausea in concussion recovery. pmc.ncbi.nlm.nih+2 Dr. Jimenez explains that by realigning the spine through chiropractic adjustments, treatment reduces nerve interference, optimizing mind-body communication, and enhancing overall function. The adjustments improve cerebral blood flow and reduce inflammation, thereby accelerating recovery from head injury. With enhanced nervous system function comes improved mental clarity, including reduced brain fog, sharper focus, and better memory, while also promoting stress relief and alleviating irritability and emotional strain often linked to head injuries. zakerchiropractic
Vestibular Rehabilitation
Vestibular rehabilitation is a specialized form of physical therapy that focuses on strengthening the connections between the brain, eyes, inner ear, muscles, and nerves. This treatment approach proves particularly valuable for post-concussion patients experiencing dizziness, vertigo, balance problems, and spatial impairment. According to a review in the British Journal of Medicine, vestibular therapy reduced symptoms in patients with sports-related concussions faster, with patients three times as likely to return to play within eight weeks of therapy compared to those who didn’t receive treatment. denverphysicalmedicine+1 Vestibular rehabilitation therapy involves exercises designed to improve the functioning between the inner ear, brain, eyes, muscles, and nerves. These exercises help minimize balance issues and treat dizziness, vertigo, and spatial orientation deficits caused by vestibular impairments that some individuals experience after brain injury. The therapy addresses issues in the inner ear through specific exercises designed to improve balance and coordination. biausa
The Epley Maneuver represents a simple yet effective exercise to treat benign paroxysmal positional vertigo, a very specific form of vertigo quite common after traumatic brain injury. During vestibular rehabilitation, benign paroxysmal positional vertigo generally responds well to the Epley Maneuver, and patients learn to perform the movement at home to alleviate symptoms as they arise. Studies have shown that vestibular rehabilitation is an effective modality for managing dizziness, vertigo, and imbalance following concussion, though careful consideration of the injury’s acuity and effective management of co-morbid conditions will optimize results. pubmed.ncbi.nlm.nih+1 Co-morbidities, including cognitive and behavioral issues, visual-perceptual dysfunction, metabolic dysfunction, and autonomic dysfunction, may hamper the effectiveness of traditional vestibular rehabilitation approaches. Working closely with other disciplines well-versed in treating these co-morbid issues helps individuals obtain optimal recovery. Dr. Jimenez’s integrated practice model exemplifies this multidisciplinary approach, bringing together chiropractic care, functional medicine, physical therapy, and other specialties to provide comprehensive treatment for patients with vestibular dysfunction following head injuries. pubmed.ncbi.nlm.nih
Physical Therapy and Exercise Rehabilitation
Physical therapy plays a pivotal role in optimizing recovery and enhancing functional independence after brain injury. Therapeutic approaches include gait training to improve walking patterns, balance activities to enhance stability and prevent falls, strength training to rebuild muscle mass and function, coordination exercises to improve fine and gross motor skills, and range-of-motion exercises to maintain flexibility. biausa In some cases, physical therapists recommend body-weight-supported treadmill training to help patients safely relearn walking patterns. Family and caregiver training proves extremely important and helpful, as loved ones can gain an understanding of how the brain works and the specific nature of the injury, supporting the rehabilitation process. biausa
Available evidence demonstrates the potential of exercise in improving cognitive impairment, mood disorders, and post-concussion syndrome following traumatic brain injury. Exercise rehabilitation has been shown to attenuate cognitive deficits in animal models by stimulating cerebral signaling pathways, with treadmill exercise improving memory by modulating neurotransmitter systems and neurotrophic factors. High-intensity interval training helps regulate the autonomic nervous system while boosting brain-derived neurotrophic factor, thereby promoting neuroplasticity, an essential factor for recovery. sciencedirect+1 However, exercise prescription following head injury requires careful consideration, as exercise intolerance commonly results from concussion and autonomic dysfunction. Graded exercise testing while monitoring symptoms and heart rate helps guide a safe return to physical activity. Current clinical practice involves careful assessment to determine appropriate exercise intensity and duration, gradually progressing as autonomic function improves. pmc.ncbi.nlm.nih
Acupuncture and Neuroplasticity Enhancement
Acupuncture has gained widespread recognition as an effective, low-cost treatment for neurological rehabilitation with minimal adverse effects. Clinical and experimental evidence documents the potential of acupuncture to ameliorate injury-induced neurological deficits, particularly sequelae such as dyskinesia, spasticity, cognitive impairment, and dysphagia. These effects relate to acupuncture’s ability to promote spontaneous neuroplasticity after injury. pmc.ncbi.nlm.nih+1 Specifically, acupuncture can stimulate neurogenesis, activate axonal regeneration and sprouting, and improve the structure and function of synapses. These processes modify the neural network and the function of the damaged brain area, leading to improvements in various skills and adaptability. Astrocytes and microglia may be involved in acupuncture-induced regulation of neuroplasticity, for example, by producing and releasing various neurotrophic factors, including brain-derived neurotrophic factor and nerve growth factor. pmc.ncbi.nlm.nih
Studies have shown that acupuncture reduces neuroinflammation after brain injury, with research published in The Journal of Neuroinflammation finding that acupuncture significantly reduced neuroinflammation and improved cognitive function in animal models of brain injury. By modulating inflammatory pathways, acupuncture helps reduce the production of pro-inflammatory cytokines, promoting brain healing and reducing symptoms such as headaches and dizziness. betsygordonacupuncture Acupuncture enhances neuroplasticity, which is crucial for recovery after brain injury, promoting improvements in memory, learning, and overall cognitive function. Research in Neural Regeneration highlighted that acupuncture promotes neuroplasticity, which is essential for rehabilitation. Studies demonstrate that acupuncture improves cognitive performance and reduces anxiety and depression in patients recovering from brain injuries. betsygordonacupuncture+1 Dr. Jimenez’s functional medicine practice incorporates acupuncture and electro-acupuncture as part of comprehensive care plans for patients recovering from head injuries. His team uses these modalities in combination with other therapies to create customized treatment approaches that promote natural healing, mobility, and long-term wellness.
Nutritional Interventions and Functional Medicine
Nutrition plays a positive role during acute traumatic brain injury recovery, with patient needs being unique and requiring individualized approaches. Following mild traumatic brain injury, patients who consumed enough food to meet calorie and macronutrient (particularly protein) needs specific to their injury severity and sex within 96 hours post-injury had reduced length of hospital stay. Patients receiving nutrients and non-nutrient support within 24-96 hours post-injury had positive recovery outcomes, including omega-3 fatty acids, vitamin D, magnesium oxide, N-acetyl cysteine, and hyperosmolar sodium lactate. frontiersin Traumatic brain injury contributes to extensive dysbiosis of the gastrointestinal system, leading to worsened outcomes, making nutritional support essential. Early nutrition supports preservation of muscle mass, decreases infection complications, promotes cerebral homeostasis, and improves recovery outcomes. The human brain consumes 20% of total resting energy, despite accounting for only 2% of total body mass, underscoring the critical role of adequate nutrition for healing. xiahepublishing
A recent clinical trial demonstrated that dietary changes significantly reduce persistent post-traumatic headaches, a common and debilitating consequence of traumatic brain injury. Researchers found that increasing omega-3 fatty acids (commonly found in fatty fish) while reducing omega-6 fatty acids (abundant in seed oils) led to fewer and less severe headaches. Participants assigned to the intervention diet experienced approximately two fewer headache days per month and a 30% reduction in daily headache pain intensity compared to the control diet group. med.unc Supplementing with omega-3 fatty acids can reduce inflammation and oxidative stress, promote brain-cell survival, and help the brain recover from injury. Vitamins D and E, niacin, zinc, and magnesium have neuroprotective benefits, and supplementing with these vitamins and minerals has been shown to improve recovery, especially in patients who are deficient. An energy-balanced, anti-inflammatory diet with adequate sources of omega-3 fats and appropriate vitamin D supplementation proves especially important for patients with a history of traumatic brain injury. consultant360
Dr. Jimenez’s practice embraces Functional Integrative Medicine, a patient-focused approach that treats the whole person rather than just symptoms. His team offers detailed health assessments that evaluate genetics, lifestyle, environmental exposures, and psychological factors to create comprehensive health profiles. By combining Institute for Functional Medicine programs with personalized nutrition plans, Dr. Jimenez helps patients address chronic conditions and optimize brain health following head injuries.
Massage Therapy and Manual Techniques
Massage therapy provides valuable support in brain injury rehabilitation, offering benefits for physical, mental, and emotional well-being. Massage significantly improves blood circulation, ensuring that essential nutrients and oxygen are efficiently delivered to brain cells. By increasing circulation, the brain’s healing process is expedited, promoting cellular regeneration and reducing the risk of secondary complications. Improved blood flow also helps reduce swelling and inflammation, common challenges following brain injury. neuropraxisrehab Post-brain injury pain can be debilitating and hinder recovery, but massage therapy helps alleviate pain by targeting tense muscles and releasing built-up tension. Through gentle manipulation, massage therapists can improve muscle flexibility and joint mobility, relieving discomfort and enhancing overall physical comfort. Brain injuries often lead to muscle stiffness and reduced range of motion, but massage therapy techniques such as stretching and kneading help improve flexibility by breaking down scar tissue and adhesions. neuropraxisrehab
Specific massage modalities show promise for traumatic brain injury recovery. Manual Lymphatic Drainage uses light massage to stimulate the flow of lymphatic fluid, potentially increasing the lymphatic system’s ability to clear waste products from the brain. A case study combining Manual Lymphatic Drainage with craniosacral therapy and glymphatic system techniques resulted in an 87% reduction of concussion symptoms after three months of treatment. concussionalliance A case study documenting massage intervention for post-concussion treatment demonstrated complete return to pre-concussion activities and function with no continued symptoms following a short and specific massage series. The treatment focused on restoring ideal alignment of the atlanto-occipital joint, resulting in reduced pain, muscle hypertonicity, headaches, reduced medication use, and improved balance, posture, cervical range of motion, mental focus, and physical activity. pmc.ncbi.nlm.nih
Dr. Jimenez’s comprehensive approach includes specialized massage and manual therapy techniques, integrated with chiropractic care and other modalities. His team focuses particularly on neck and shoulder areas to reduce effects patients experience after traumatic brain injuries, with goals including improved neck mobility, reduction of headaches and nerve pain, and addressing balance, dizziness, and vertigo issues through specific therapeutic techniques. newapproachescenter
Cognitive Behavioral Therapy and Psychological Support
Cognitive Behavioral Therapy has been demonstrated to be effective by over 1,000 studies involving 10,000 patients, making it one of the most scientifically verified psychotherapy treatments available. CBT has been successfully used on a variety of disorders, including traumatic brain injury patients with post-concussional symptoms and secondary effects such as anxiety and fatigue. The therapy focuses on the relationship between thoughts, feelings, and behaviors, built around three core principles: beliefs create feelings, feelings dictate behavior, and behavior reinforces beliefs. flintrehab A new meta-analysis found substantial evidence for the use of cognitive behavioral therapy in managing anxiety and depression in patients with traumatic brain injury. Researchers identified that CBT interventions had immediate effects of reducing depression and anxiety, with effects sustained for depression at the three-month follow-up. Effects were greater in groups that received individualized CBT than in those that received group-based CBT. headway
CBT proves particularly valuable for addressing recovery expectations and perceived consequences of traumatic brain injury. Behavioral techniques such as relaxation, behavioral activation, and stress management help patients manage the anxiety, depressive symptoms, and insomnia that can be present following injury. In the acute phase of recovery, brief psychoeducational and cognitive behavioral interventions have consistently been shown to result in improvement in managing cognitive and psychological symptoms for brain injury survivors. abct For patients with cognitive impairment, CBT can be adapted with modifications including simplified concepts, concrete behavioral examples, pictorial handouts and cues, considerable repetition, and booster sessions. Studies found that adapted CBT was able to reduce anxiety and depression in patients who suffered moderate to severe traumatic brain injury. CBT helps patients identify and challenge unhelpful or inaccurate thoughts that can arise or intensify after injury, while focusing on behavioral activation and engaging in meaningful, important activities, which can boost mood and decrease isolation. cbtdenver+1
Mind-Body Therapies and Somatic Approaches
Mind-body therapies have gained recognition for their effectiveness in treating trauma-related symptoms and supporting nervous system regulation. More than 80% of specialized programs to treat post-traumatic stress disorder offer some form of mind-body therapy, including yoga, relaxation, tai chi, guided imagery, and mindfulness practices. These approaches prove particularly valuable for individuals experiencing somatic symptoms following head injuries. research.va Somatic therapy helps individuals reconnect with their bodies through awareness of physical sensations and their relationship to emotional experiences. For patients with head injuries who may feel disconnected from their bodies or experience persistent physical symptoms, somatic approaches provide pathways for healing by working through sensations in safe and supportive environments. Techniques such as grounding exercises, deep breathing, mindful observation of physical sensations, and guided movement empower individuals to explore how trauma manifests physically and provide avenues for release. pacmh
Yoga as a whole significantly reduced post-traumatic stress disorder symptoms in research studies, with a positive impact comparable to that of psychotherapeutic and psychopharmacologic approaches. Yoga may improve the functioning of traumatized people by helping them tolerate physical and sensory experiences associated with fear and helplessness, and increasing emotional awareness and affect tolerance. For individuals recovering from head injuries, gentle yoga practices adapted to their current functional abilities can support both physical and psychological healing. research.va Polyvagal theory provides a powerful framework for understanding how trauma affects the nervous system and pathways for healing. The theory centers on the autonomic nervous system as a key component in trauma recovery, emphasizing the role of the vagus nerve in regulating physiological and emotional states. Basic somatic exercises can bring the nervous system out of dysfunction, beginning to retrain safety and social cues. This proves particularly helpful for individuals with head injuries who experience autonomic dysregulation and hypervigilance. pyramid-healthcare
Breathing Practices and Vagal Tone Restoration
Voluntary regulated breathing practices offer accessible and effective means to support autonomic nervous system regulation and restore vagal tone. These practices draw on both modern scientific studies and ancient concepts, with applications ranging from clinical anxiety treatment to stress reactivity reduction. Effective breathing interventions support greater parasympathetic tone, which can counterbalance the high sympathetic activity intrinsic to stress and dysfunction following head injury. pmc.ncbi.nlm.nih The physiological sigh is a simple yet powerful breathing technique that involves two nose inhales, followed by a long exhale through the mouth. This technique rapidly reduces stress and calms the nervous system by leveraging the interaction between the sympathetic (arousing) and parasympathetic (calming) branches of the autonomic nervous system to control heart rate and promote calm. Studies have shown that this breathing pattern effectively reduces arousal and returns the body to baseline functioning. hubermanlab+1
Deep, slow breathing benefits vagal outflow, with evidence suggesting particular benefits for older adults in restoring vagal tone. One session of deep and slow breathing can produce measurable improvements in heart rate variability metrics associated with parasympathetic activity. Regular practice of paced breathing at approximately six cycles per minute, significantly lower than the standard respiratory rate of 12 to 20 breaths per minute, can enhance vagal tone and improve overall autonomic regulation. pmc.ncbi.nlm.nih+1 Heart rate variability biofeedback is an innovative, non-invasive, evidence-based technique that enhances vagal nerve activity by combining slow-paced breathing with real-time feedback. The practice proves simple to implement, cost-effective, and carries minimal risk, making it an accessible tool for various health interventions. HRV biofeedback likely modulates neuroplasticity in autonomic control centers, enhancing parasympathetic tone and improving cardiac efficiency, reducing sympathetic overactivation, and lowering systemic inflammation. pmc.ncbi.nlm.nih
Improving Central Nervous System Function and Communication
The comprehensive non-surgical treatments described work synergistically to improve central nervous system function and restore proper communication between the brain and body. These approaches target multiple aspects of neurological health, from cellular-level processes to whole-system integration, supporting the brain’s remarkable capacity for adaptation and healing known as neuroplasticity. Neuroplasticity represents the brain’s ability to reorganize and form new neural connections throughout life, enabling recovery from injury by creating alternative pathways when original circuits become damaged. Following a brain injury, neuroplasticity’s ability to adapt becomes crucial, as these injuries frequently result in severe impairments. Rehabilitation strategies exploit neuroplasticity, leveraging the brain’s plasticity to promote healing through approaches ranging from constraint-induced movement therapy to virtual reality and brain-computer interfaces. pmc.ncbi.nlm.nih
The integration of multiple treatment modalities enhances neuroplastic responses and accelerates recovery. Combining chiropractic care with vestibular rehabilitation, for example, addresses both spinal alignment and sensory integration, creating synergistic effects that amplify benefits beyond what either treatment could achieve alone. Similarly, pairing nutritional interventions with physical therapy provides both the structural building blocks and functional stimulation necessary for optimal neural repair and reorganization. frontiersin+4 Dr. Jimenez’s practice exemplifies this integrated approach, combining specialized chiropractic protocols with wellness programs, functional and integrative nutrition, agility and mobility fitness training, and rehabilitation systems for all ages. The team has taken great pride in providing patients with only clinically proven treatment protocols, using an integrated approach to create personalized care plans that often include functional medicine, acupuncture, electro-acupuncture, and sports medicine principles. The goal is to relieve pain naturally by restoring the body’s health and function through holistic wellness as a lifestyle.
Restoring Vagal Tone and Autonomic Balance
The vagus nerve, as the main neural component of the parasympathetic nervous system, plays a crucial role in maintaining physiological homeostasis. The vagus nerve starts in the brain and ends in the abdomen, and it is responsible for the involuntary functions of the heart, lungs, digestive system, liver, and kidneys. Following a head injury, vagal tone frequently becomes diminished, contributing to autonomic dysfunction and associated symptoms. pmc.ncbi.nlm.nih+3 Heart rate variability serves as a non-invasive biomarker of vagal tone and autonomic flexibility, with reduced HRV associated with cardiovascular diseases, hypertension, inflammation, and mental health disorders. Non-invasive vagal neuromodulation through HRV biofeedback and similar interventions could potentially serve as rehabilitative strategies to restore autonomic balance, mitigate post-injury fatigue, and improve cardiovascular function. pmc.ncbi.nlm.nih
Practices such as breathwork, cold exposure, exercise, meditation, taking probiotics, laughter, singing, massages, and relaxation exercises help improve vagal tone. These accessible interventions provide multiple pathways for patients to actively participate in their recovery, building resilience and enhancing the body’s natural regulatory capacities. High vagal tone is associated with greater resilience to stress, promoting activation of the parasympathetic nervous system and reducing physiological symptoms of stress, such as increased heart rate and muscle tension. neurodivergentinsights+1 The Safe and Sound Protocol represents another non-invasive approach engaging the ventral vagal complex via auditory-motor pathways, facilitating neuroplasticity and enhancing emotional regulation. This protocol may function by modulating the prefrontal cortex’s influence on autonomic outflow, thereby promoting a shift toward parasympathetic dominance. Combined with heart rate variability biofeedback, these approaches offer promising avenues for restoring vagal tone and autonomic balance following head injury. pmc.ncbi.nlm.nih
Enhancing Communication Between Brain and Body
Effective treatment of head injuries requires addressing the fundamental disruption in communication between the brain and body that occurs following trauma. The somatovisceral response, characterized by intricate interactions between somatic (bodily) and visceral (organ) systems, depends on intact nerve signal transmission for proper function. When head injuries disrupt these communication pathways, comprehensive interventions targeting multiple levels of the nervous system become necessary. foundationhealth
- Chiropractic care directly addresses communication disruption by restoring proper spinal alignment, reducing nerve interference, and optimizing signal transmission between the brain and body. Research demonstrates that chiropractic adjustments can improve brain function by supporting proper cerebrospinal fluid flow and blood circulation, which are crucial for healing after traumatic brain injuries. By facilitating a return to the preferred anatomical form through therapy, function is restored, allowing a complete return to pre-injury activities. hmlfunctionalcare+2
- Vestibular rehabilitation specifically targets multisensory integration, recognizing that the vestibular system plays a role in multisensory binding, giving rise to a unified multisensory experience underlying self-representation and bodily self-awareness. By addressing vestibular dysfunction through targeted exercises, therapy helps restore temporal binding of sensory information, reducing perceptual chaos and improving coherence of bodily experience. pmc.ncbi.nlm.nih
- Acupuncture enhances brain-body communication through multiple mechanisms, including stimulation of neuroplasticity, modulation of neurotransmitter systems, and regulation of inflammatory processes. The effect of acupuncture begins with the stimulation of acupoints, which converts physical or chemical information into electrical activity that sends signals along afferent fibers to the spinal cord and brain. This modulation of neural structure and function supports restoration of proper communication throughout the nervous system. pmc.ncbi.nlm.nih
- Functional medicine approaches recognize that optimal brain-body communication requires addressing multiple factors, including nutrition, inflammation, gut health, hormone balance, and detoxification. Dr. Jimenez’s practice uses detailed Institute for Functional Medicine Collaborative Assessment Programs focused on Integrative Treatment Protocols, thoroughly evaluating personal history, current nutrition, activity behaviors, environmental exposures to toxic elements, and psychological and emotional factors. This comprehensive approach addresses the root causes of chronic disorders, treating the person holistically rather than just managing symptoms.
Improving Somatic and Autonomic Systems
The ultimate goal of comprehensive treatment for head injuries is to restore balance and proper function to both the somatic (voluntary) and the autonomic (involuntary) nervous systems. The somatic nervous system connects to most senses and helps control voluntary muscle movements, while the autonomic nervous system regulates involuntary bodily functions, including heart rate, blood pressure, digestion, and breathing. clevelandclinic Following a head injury, both systems frequently become dysregulated, leading to wide-ranging symptoms affecting physical function, cognitive abilities, and emotional well-being. Addressing this dysregulation requires integrated approaches that simultaneously target physical alignment, sensory processing, autonomic balance, and neuroplasticity. pmc.ncbi.nlm.nih+1
- Physical therapy, including vestibular rehabilitation and gait training, directly addresses somatic system function by retraining movement patterns, improving balance and coordination, and rebuilding strength and endurance. These interventions leverage neuroplasticity to establish new motor programs and compensatory strategies, supporting functional recovery even when some neural damage persists. pmc.ncbi.nlm.nih+1
- Autonomic system restoration requires approaches specifically targeting vagal tone and parasympathetic activation. Heart rate variability biofeedback, breathing practices, massage therapy, and acupuncture all support enhanced parasympathetic tone, helping shift the nervous system from states of hyperarousal toward balanced regulation. Dr. Jimenez emphasizes that, by focusing on flexibility, agility, and strength through tailored programs, his practice helps patients of all ages thrive despite health challenges. massgeneral+3
- Nutritional interventions support both somatic and autonomic function by providing essential building blocks for neural repair, reducing inflammation, supporting mitochondrial function, and optimizing neurotransmitter production. Omega-3 fatty acids, for example, reduce inflammation and oxidative stress while promoting brain cell survival, supporting both structural repair and functional optimization. xiahepublishing+2
- Cognitive-behavioral therapy and mind-body approaches address the psychological and emotional factors that influence both somatic and autonomic function. By helping patients reframe unhelpful thoughts, manage anxiety and depression, and develop healthy coping strategies, these interventions support overall nervous system regulation and functional recovery. pacmh+3
The Path Forward: Integrative Care for Head Injury Recovery
Recovery from head injuries represents a complex journey requiring patience, persistence, and comprehensive support. The disruption to brain-body communication and development of somatovisceral disorders following head trauma creates challenges that cannot be addressed through single-modality treatments. Instead, the most effective approach involves integrated care that simultaneously addresses physical alignment, sensory processing, autonomic regulation, nutrition, psychological well-being, and neuroplasticity enhancement. Dr. Jimenez’s practice in El Paso exemplifies this integrative model, bringing together chiropractic care, functional medicine, physical therapy, acupuncture, and other evidence-based approaches to provide comprehensive treatment tailored to each patient’s unique needs. His philosophy recognizes that the body has an innate healing capacity when provided with proper support, emphasizing natural recovery methods over invasive procedures or addictive medications. The evidence reviewed throughout this article demonstrates that non-surgical treatments can effectively improve somatovisceral function, restore vagal tone, enhance brain-body communication, and support recovery of both somatic and autonomic nervous systems. These approaches work synergistically, creating conditions that support the brain’s remarkable capacity for adaptation and healing through neuroplasticity. pubmed.ncbi.nlm.nih+6
For individuals recovering from head injuries, seeking comprehensive evaluation and integrated treatment early in the recovery process offers the best opportunity for optimal outcomes. Dr. Jimenez emphasizes that early identification of at-risk patients appears feasible, with somatic symptom disorder potentially serving as a useful framework for conceptualizing poor outcomes from mild traumatic brain injury in patients with prominent psychological distress and guiding rehabilitation. neurologyopen.bmj The future of head injury treatment lies in continued refinement of these integrated approaches, with ongoing research exploring optimal combinations of interventions, timing of treatment initiation, and personalization based on individual patient characteristics. As understanding of brain-body connections deepens and evidence for non-surgical treatments continues to accumulate, patients have increasing reason for hope that recovery is possible with the right comprehensive support. frontiersin
Conclusion
Head traumas cause serious problems with the complex communication systems that link the brain and body. This may lead to somatovisceral illnesses that affect multiple bodily systems simultaneously. To develop effective treatments, it’s important to understand how environmental influences affect brain activity, how symptoms overlap and cluster, and how everyday functioning might be affected. The extensive evidence examined indicates that non-surgical interventions, such as chiropractic care, vestibular rehabilitation, physical therapy, acupuncture, nutritional modifications, massage therapy, cognitive-behavioral therapy, and mind-body techniques, can successfully restore function after head injuries. These treatments increase the function of the central nervous system, restore vagal tone and autonomic balance, and improve communication between the brain and the body. In the end, they help both the somatic and autonomic systems heal.
Dr. Alexander Jimenez’s clinical observations and integrative treatment strategy in El Paso, Texas, demonstrate how integrating evidence-based modalities into individualized care regimens can facilitate optimal patient recovery. This all-encompassing approach gives hope to those who are recovering from head traumas and have somatovisceral problems by concentrating on the body’s inherent ability to heal and treating the fundamental causes instead of merely the symptoms. To get well, you need to be patient, keep going, and get the right help. Integrated care, on the other hand, may help people regain function, lessen symptoms, and enhance their quality of life by treating all areas of health. As research continues to improve our knowledge of how the brain and body work together and how successful treatments are, the future looks bright for even better ways to help people recover from head injuries.
References
- Jobin, K., Wilson, A. J., King, R., Eliason, P. H., Galarneau, J., Gilmour, G. S., & Debert, C. T. (2025). Somatic symptom and related disorders and mild traumatic brain injury: A systematic review. Biopsychosocial Science and Medicine. https://doi.org/10.1097/PSY.0000000000001427
- Silverberg, N. D., Rioux, M., Mikolić, A., Perez, D. L., Burke, M. J., & Howard, A. (2025). Somatic symptom disorder after mild traumatic brain injury. Journal of Head Trauma Rehabilitation. https://doi.org/10.1097/HTR.0000000000001068
- Braun, T., & The ENIGMA Consortium. (2024). How does the macroenvironment influence brain and behaviour—a review. Molecular Psychiatry, 29, 3268–3286. https://doi.org/10.1038/s41380-024-02557-x
- Harricharan, S., Nicholson, A. A., Densmore, M., Théberge, J., McKinnon, M. C., Neufeld, R. W., & Lanius, R. A. (2022). The brain-body disconnect: A somatic sensory basis for trauma-related disorders. Frontiers in Neuroscience, 16, Article 1015749. https://doi.org/10.3389/fnins.2022.1015749
- Defense and Veterans Brain Injury Center. (2023). Information paper: The impact of mild traumatic brain injury on the autonomic nervous system. https://health.mil/Reference-Center/Publications/2023/03/15/TBICoE-Information-Paper
- Engel, G. L., Winters, M., Giannoulakis, C., Gong, W., Kalns, J. E., Bingaman, S., & Williamson, J. B. (2022). Autonomic dysfunction after moderate-to-severe traumatic brain injury. BMJ Neurology Open, 4(1), Article e000308. https://doi.org/10.1136/bmjno-2022-000308https://doi.org/10.1136/bmjno-2022-000308
- Katz, D. I., Cohen, S. I., & Alexander, M. P. (2015). Mild traumatic brain injury. Handbook of Clinical Neurology, 127, 131-156.
- Hilz, M. J., Wang, R., Xu, X., & Reichmann, H. (2017). Autonomic dysfunction after mild traumatic brain injury. Frontiers in Neurology, 8, Article 511. https://doi.org/10.3389/fneur.2017.00511
- Yuan, J., Liu, W., Liang, Q., Wang, Y., Liu, M., & Zhang, J. (2023). Negative environmental influences on the developing brain. Exploration of Medicine, 4(5), 804-820. https://doi.org/10.37349/emed.2023.00169
- Cleveland Clinic. (2025). Somatic nervous system: What it is & function. https://my.clevelandclinic.org/health/body/23291-somatic-nervous-system
- Baguley, I. J., Heriseanu, R. E., Cameron, I. D., Nott, M. T., & Slewa-Younan, S. (2008). A critical review of the pathophysiology of dysautonomia following traumatic brain injury. Neurocritical Care, 8(2), 293-300.
- Calderón-Garcidueñas, L., Hernández-Luna, J., Mukherjee, P. S., Styner, M., Chávez-Franco, D. A., Luévano-Castro, S. C., … & González-Maciel, A. (2024). Air pollution and brain health. Environmental Health Sciences Center. https://environmentalhealth.ucdavis.edu/air-pollution/brain-health
- Boston Children’s Hospital. (2025). Somatic symptom and related disorders. https://www.childrenshospital.org/conditions/somatic-symptom-and-related-disorders
- Cognitive FX. (2024). Post-concussion autonomic dysfunction. https://www.cognitivefxusa.com/blog/post-concussion-autonomic-dysfunction-dysautonomia
- Anatolia, M. S., & Kızıl, Y. (2023). Environmental influences on brain aging. Mechanisms of Ageing and Development, 215, Article 111850.
- Psychology Today. (2025). The brain-body disconnect: A key to trauma recovery. https://www.psychologytoday.com/us/blog/healing-from-trauma/202507/the-brain-body-disconnect-a-key-to-trauma-recovery
- Concussion Alliance. (2024). Autonomic nervous system dysfunction. https://www.concussionalliance.org/autonomic-nervous-system-dysfunction
- Poldrack, R. A., Shine, J. M., Shine, R., Ferguson, M. A., Pessoa, L., Lindquist, M. A., & Uddin, L. Q. (2024). A longitudinal single-subject neuroimaging study reveals the effects of daily environmental, physiological, and lifestyle factors on functional brain connectivity. PLOS Biology, 22(10), Article e3002797.
- Gianaros, P. J., & Jennings, J. R. (2025). Brain–body states as a link between cardiovascular and mental health. Trends in Neurosciences. https://doi.org/10.1016/j.tins.2025.01.017
- Medscape. (2023). Post head injury autonomic complications. https://emedicine.medscape.com/article/325994-overview
- Allegheny Health Network. (2025). Healing the brain and body: Traumatic brain injury rehab. https://www.ahn.org/health/articles/healing-the-brain-and-body-traumatic-brain-injury-rehab
- Yadav, N., & Morris, R. (2025). Harnessing non-invasive vagal neuromodulation: HRV biofeedback and the safe and sound protocol. Journal of Integrative Neuroscience, 24(3), Article 101. https://doi.org/10.31083/j.jin2403101
- Northwest Florida Physicians Group. (2025). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries
- Memorial Hermann. (2025). Brain injury rehabilitation. https://memorialhermann.org/services/treatments/brain-injury-rehabilitation
- Neurodivergent Insights. (2022). How to improve vagal tone for mental and emotional well-being. https://neurodivergentinsights.com/how-to-improve-vagal-tone
- Neuro Trauma Centers. (2025). Chiropractic care for traumatic brain injury. https://neurotraumacenters.com/2025/02/19/chiropractic-care-for-traumatic-brain-injury
- Brooke Army Medical Center. (n.d.). Brain injury rehabilitation. https://bamc.tricare.mil/Health-Services/Specialty-Care/Rehabilitation-Medicine/Brain-Injury-Rehabilitation
- Massachusetts General Hospital. (2024). The vagus nerve: A key player in your health and well-being. https://www.massgeneral.org/news/article/vagus-nerve
- HML Functional Care. (2025). How chiropractic neurology supports brain healing. https://hmlfunctionalcare.com/how-chiropractic-neurology-supports-brain-healing
- Mayo Clinic. (2021). Traumatic brain injury – Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561
- Russo, M. A., Santarelli, D. M., & O’Rourke, D. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11, Article 19267. https://doi.org/10.1038/s41598-021-98736-9
- Zaker Chiropractic. (2024). Chiropractic care for head injury rehabilitation. https://zakerchiropractic.com/chiropractic-care-head-injury-rehabilitation
- Shen, Y., Jiang, L., Lai, J., Hu, J., Liang, F., Zhang, X., & Ma, F. (2025). A comprehensive review of rehabilitation approaches for traumatic brain injury: Efficacy and outcomes. Frontiers in Neurology, 16, Article 1608645. https://doi.org/10.3389/fneur.2025.1608645
- Mayo Clinic. (2024). Vagus nerve stimulation. https://www.mayoclinic.org/tests-procedures/vagus-nerve-stimulation/about/pac-20384565
- Northwestern Health Sciences University. (2025). Chiropractic Economics: Chiropractic and traumatic brain injuries. https://www.nwhealth.edu/news/reis-writes-for-chiropractic-economics-chiropractic-and-traumatic-brain-injuries
- Sun, J. H., Tan, L., & Yu, J. T. (2025). Advances in clinical neurorestorative treatments in brain trauma. Journal of Neurorestoratology. https://doi.org/10.1016/j.jnrt.2025.100130https://doi.org/10.1016/j.jnrt.2025.100130
- Association of American Medical Colleges. (2025). Enlisting the vagus nerve to help the body heal itself. https://www.aamc.org/news/enlisting-vagus-nerve-help-body-heal-itself
- Stude, D., & Mick, G. (2018). Patients receiving chiropractic care in a neurorehabilitation hospital: A retrospective case series. Journal of Chiropractic Medicine, 17(2), 127-136. https://doi.org/10.1016/j.jcm.2017.11.008
- Caring Medical. (2024). How can you repair your vagus nerves? https://caringmedical.com/can-repair-vagus-nerves
- Haavik, H., Kumari, N., Holt, K., Niazi, I. K., Amjad, I., Pujari, A. N., … & Murphy, B. (2024). Effect of chiropractic intervention on oculomotor and attentional performance. Brain Sciences, 14(5), Article 423.
- Neuro Injury Care. (2024). Vestibular rehabilitation – Guide to Epley Maneuver for TBI. https://neuroinjurycare.com/vestibular-rehab-epley-maneuver-for-tbi
- Wang, Q., Chen, C., Cai, J., Wang, T., Zhou, X., Wang, X., … & Zhang, H. (2022). The impact of acupuncture on neuroplasticity after ischemic stroke: A literature review and perspectives. Frontiers in Cellular Neuroscience, 16, Article 817732. https://doi.org/10.3389/fncel.2022.817732https://doi.org/10.3389/fncel.2022.817732
- Choi, W. J., & Kim, M. J. (2023). Nutritional support following traumatic brain injury. Exploratory Research and Hypothesis in Medicine, 8(4), 389-403. https://doi.org/10.14218/ERHM.2022.00086
- Schneider, A. L. C., Lakshminarayan, K., Peterlin, B. L., & Gottesman, R. F. (2013). Vestibular rehabilitation following mild traumatic brain injury. NeuroRehabilitation, 32(3), 519-528.
- Betsy Gordon Acupuncture. (2024). Acupuncture reduces neuroinflammation after brain injury. https://betsygordonacupuncture.com/acupuncture-reduces-neuroinflammation-after-brain-injury
- Finnegan, E., Daly, E., Pearce, A. J., & Ryan, L. (2022). Nutritional interventions to support acute mTBI recovery. Frontiers in Nutrition, 9, Article 977728. https://doi.org/10.3389/fnut.2022.977728https://doi.org/10.3389/fnut.2022.977728
- Brain Injury Association of America. (2025). Physical therapy and brain injury recovery. https://biausa.org/public-affairs/media/physical-therapy-and-brain-injury
- Chavez, L. M., Huang, S. S., MacDonald, I., Lin, J. G., Lee, Y. C., & Chen, Y. H. (2021). Effect of acupuncture on neuroplasticity of stroke patients with motor dysfunction: A meta-analysis of fMRI studies. Evidence-Based Complementary and Alternative Medicine, 2021, Article 8841720.
- Consultant360. (2021). Feeding the brain: Nutrition for patients with traumatic brain injury. https://www.consultant360.com/article/nutrition411/emergency-medicine/feeding-brain-nutrition-patients-traumatic-brain-injury
- Washington University in St. Louis. (2025). Vestibular and concussion rehabilitation. https://pt.wustl.edu/patient-care/service-lines/vestibular-and-concussion-rehabilitation
- Sun, X., Zhang, Y., Zhang, N., Fang, S., Meng, X., Zhang, X., … & Wang, J. (2024). Acupuncture, an effective treatment for post-stroke neurologic rehabilitation. Complementary Therapies in Medicine, 87, Article 103168.
- University of North Carolina School of Medicine. (2025). New research finds that changing your diet could ease persistent headaches after a brain injury. https://www.med.unc.edu/phyrehab/uncategorized/new-research-finds-changing-your-diet-could-ease-persistent-headaches
- Denver Physical Medicine. (2024). Vestibular rehabilitation. https://denverphysicalmedicine.com/services/vestibular-rehabilitation
- Flint Rehab. (2025). Acupuncture for brain injury: Is it an effective treatment? https://www.flintrehab.com/acupuncture-for-brain-injury
- Flint Rehab. (2025). Nutrition therapy for traumatic brain injury: How it works. https://www.flintrehab.com/nutrition-therapy-for-traumatic-brain-injury
- Cleveland Clinic. (2025). Vestibular rehabilitation therapy: What it is & exercises. https://my.clevelandclinic.org/health/treatments/15298-vestibular-rehabilitation
- Modern Oriental Medicine. (2025). Acupuncture and neuroplasticity: Rewiring the brain for healing. https://modernorientalmedicine.com/blog/f/acupuncture-and-neuroplasticity-rewiring-the-brain-for-healing
- UCLA Health. (2022). Nutrition may play a key role in supporting brain health for people recovering from a TBI. https://www.uclahealth.org/news/article/nutrition-may-play-a-key-role-in-supporting-brain-health-for-people-recovering-from-a-tbi
- Cognitive FX. (2023). How to get the best vestibular therapy for concussion symptoms. https://www.cognitivefxusa.com/blog/vestibular-therapy-for-concussion-symptoms
- Liu, X., Wang, Y., Yang, Z., Zhang, Y., Chen, Y., Wang, J., … & Tao, J. (2025). The effect of acupuncture combined with hyperbaric oxygenation therapy on patients with traumatic brain injury. Frontiers in Neurology, 16, Article 1538740.
- Neuropraxis Rehab. (2023). The healing touch: Benefits of massage after brain injury. https://neuropraxisrehab.com/the-healing-touch-benefits-of-massage-after-brain-injury
- Wright, A. D., Smirl, J. D., Bryk, K., & van Donkelaar, P. (2023). Autonomic dysfunction and exercise intolerance in concussion: A narrative review. Journal of Athletic Training, 58(7-8), 539-550. https://doi.org/10.4085/1062-6050-0103.22
- Pacific Mental Health. (2025). The mind-body connection: Understanding somatic therapies. https://pacmh.org/the-mind-body-connection-understanding-somatic-therapies
- New Approaches Center. (2025). Massage therapy after a traumatic brain injury. https://newapproachescenter.com/physical-therapy-after-a-traumatic-brain-injury
- Mission Connection Healthcare. (2025). Somatic therapy for PTSD & anxiety. https://missionconnectionhealthcare.com/our-approach/somatic-therapy
- Morin, M., & Dumoulin, S. O. (2015). Concussion treatment using massage techniques: A case study. Journal of Bodywork and Movement Therapies, 19(2), 252-258. https://doi.org/10.1016/j.jbmt.2014.04.012
- Aspire Psychology Portland. (2025). Healing trauma & anxiety with mind-body therapy: A holistic approach. https://www.aspirepsychologyportland.com/our-blog/somatic-therapy-explained-mind-body-healing-for-trauma-anxiety-amp-stress
- Concussion Alliance. (2016). Massage therapy. https://www.concussionalliance.org/massage-therapy
- Hassett, L. M., Moseley, A. M., Harmer, A. R., & Mackey, M. G. (2021). The benefits of exercise for outcome improvement following traumatic brain injury: A systematic review. Experimental Neurology, 350, Article 113960.
- US Department of Veterans Affairs. (2019). Review study points to the most effective mind-body therapies for PTSD. https://www.research.va.gov/currents/0119-Mind-body-therapies-for-PTSD.cfm
- Brain Injury Association of Michigan. (2018). Addressing the symptoms of brain injury using massage therapy. https://www.biami.org/wp-content/uploads/2018/01/FR12-Jenks.pdf
- Cognitive FX. (2024). Brain injury and exercise: How cardio intervals help patients recover. https://www.cognitivefxusa.com/blog/brain-injury-exercise
- Gisolfi, A., Wagner, A. K., Rasmussen, S., & Borrasso, A. J. (2025). The acceptability of somatic therapy for PTSD among patients in primary care. Families, Systems, & Health. https://doi.org/10.1037/fsh0001007
- AutoAccident.com. (2024). Massage for brain-injured patients. https://autoaccident.com/massage
- Kulkarni, M., Brown, R., Stuart, R., Tahir, H., & Granner, M. A. (2025). Altered autonomic cardiovascular function in adults with persisting post-concussion symptoms and exercise intolerance. Physiological Reports, 13(11), Article e70378.
- Davis, D. W., Harris, O. A., & Frim, D. M. (2023). Massage therapy may be safe and reduce pain in critically ill patients with acute neurological injury. Brain Injury, 37(10), 998-1005. https://doi.org/10.1080/02699052.2023.2247990
- Lim, J. A., Salles, A., & You, J. S. (2025). Exercise effects on cardiovascular, autonomic, cerebrovascular, and cognitive functions in spinal cord injury. Journal of Neurotrauma. https://doi.org/10.1089/neu.2024.0523
- Ćwirlej-Sozańska, A., Sozański, B., Wiśniowska-Szurlej, A., & Wilmowska-Pietruszyńska, A. (2023). Adaptive neuroplasticity in brain injury recovery: Mechanisms, challenges and therapeutic implications. International Journal of Molecular Sciences, 24(18), Article 14210. https://doi.org/10.3390/ijms241814210
- Clauw, D. J., & Chrousos, G. P. (2015). Chronic pain: Where the body meets the brain. Transactions of the American Clinical and Climatological Association, 126, 167-183.
- Pyramid Healthcare. (2023). Treating trauma with polyvagal theory. https://www.pyramid-healthcare.com/blog/2023/06/09/treating-trauma-with-polyvagal-theory
- Psychiatric Times. (2025). The healing code: Harnessing neuroplasticity for brain injury recovery. https://www.psychiatrictimes.com/view/the-healing-code-harnessing-neuroplasticity-for-brain-injury-recovery
- Wikipedia. (2025). Somatic symptom disorder. https://en.wikipedia.org/wiki/Somatic_symptom_disorder
- Counseling Today. (2025). Trauma stabilization through polyvagal theory and DBT. https://www.counseling.org/publications/counseling-today-magazine/article-archive/article/legacy/trauma-stabilization-through-polyvagal-theory-and-dbt
- Neuropsychology Dorset. (2025). Neuroplasticity: How the brain adapts and recovers from injury. https://www.neuropsychologydorset.co.uk/post/neuroplasticity-brain-adaptation-recovery
- Chopra, A., Diwan, A. D., & Cooney, M. (2025). Differentiating complex regional pain syndrome from somatic symptom disorder. PLOS Mental Health, 2(1), Article e0000214.
- Dr. Arielle Schwartz. (2024). The polyvagal theory and healing complex PTSD. https://drarielleschwartz.com/the-polyvagal-theory-and-healing-complex-ptsd-dr-arielle-schwartz
- Morrison, S., & Sudmeier, L. (2025). The neuroplastic brain: Current breakthroughs and emerging frontiers. Brain Research, 1850, Article 149212.
- Children’s Hospital of Philadelphia. (2024). Somatic symptom and related disorders. https://www.chop.edu/conditions-diseases/somatic-symptom-and-related-disorders-ssrds
- The MH Collective. (2023). Trauma + the polyvagal theory. https://themhcollective.com/trauma-and-the-polyvagal-theory-dr-nazneen-nizami
- Centre for Neuro Skills. (2025). Neuroplasticity. https://www.neuroskills.com/neuroplasticity
- PM&R KnowledgeNow. (2024). Somatic symptom disorder. https://now.aapmr.org/somatic-symptom-disorder
- Nicabm. (2022). Polyvagal theory and trauma. https://www.nicabm.com/topic/polyvagal-theory-explained
- Khadka, S., Zhou, X., Dhiman, S., Hu, M., & Jiang, H. (2025). A comprehensive review of adaptive plasticity and recovery mechanisms following traumatic brain injury. Neurological Practice and Epidemiology, 7(1), Article 70006.
- American Psychiatric Association. (n.d.). What is somatic symptom disorder? https://www.psychiatry.org/patients-families/somatic-symptom-disorder/what-is-somatic-symptom-disorder
- Porges, S. W. (2021). Trauma and the nervous system: A polyvagal perspective [Video]. YouTube. https://www.youtube.com/watch?v=ZdIQRxwT1I0
- Physiopedia. (2023). Role of neuroplasticity in neuro-rehabilitation. https://www.physio-pedia.com/Role_of_Neuroplasticity_in_Neuro-rehabilitation
- Ohio State University Wexner Medical Center. (n.d.). An innovative treatment for chronic post-traumatic headaches. https://wexnermedical.osu.edu/departments/innovations/pmrnews/chronic-post-traumatic-headaches
- Headway. (2024). CBT for anxiety and depression after TBI. https://www.headway.org.uk/about-brain-injury/further-information/research/psychological-effects-of-brain-injury-research/cbt-for-anxiety-and-depression-after-tbi
- Practical Neurology. (2025). Sleep & traumatic brain injury. https://practicalneurology.com/diseases-diagnoses/sleep/sleep–traumatic-brain-injury/30113
- Practical Neurology. (2025). Post-traumatic headache treatment guide. https://practicalneurology.com/diseases-diagnoses/tbi/aches-and-trauma-understanding-post-traumatic-headache-part-2-management-and-treatment/30119
- Flint Rehab. (2021). Cognitive behavioral therapy after traumatic brain injury. https://www.flintrehab.com/cognitive-behavioral-therapy-after-traumatic-brain-injury
- Modarres, M., Kuzma, N. N., Kretzmer, T., Pack, A. I., & Lim, M. M. (2024). Traumatic brain injury-induced disruption of the circadian clock. Brain, Behavior, & Immunity – Health, 36, Article 100724.
- American Migraine Foundation. (2025). Concussion, migraine & post-traumatic headache. https://americanmigrainefoundation.org/resource-library/concussion-and-post-traumatic-headache
- CBT Denver. (2025). CBT for brain injury: Improve mood, coping & functioning. https://www.cbtdenver.com/blog/cbt-for-brain-injury
- Cantor, J. B., Ashman, T., Gordon, W., Ginsberg, A., Engmann, C., Egan, M., … & Dijkers, M. (2024). Sleep and circadian rhythms after traumatic brain injury: A narrative review. Sleep Medicine Reviews, 81, Article 102065.
- Willer, B., & Leddy, J. J. (2012). Medical therapies for concussion. Physical Medicine and Rehabilitation Clinics of North America, 23(2), 467-479.
- Association for Behavioral and Cognitive Therapies. (2024). Adult traumatic brain injury for mental health professionals. https://www.abct.org/fact-sheets/adult-traumatic-brain-injury-for-mental-health-professionals
- Ayalon, L., Borodkin, K., Dishon, L., Kanety, H., & Dagan, Y. (2007). Circadian rhythm sleep disorders following mild traumatic brain injury. Neurology, 68(14), 1136-1140.
- Cognitive FX. (2025). Post-concussion headaches: Causes & treatment options. https://www.cognitivefxusa.com/blog/concussion-headaches-and-post-concussion-headaches
- Brainline.org. (2022). Cognitive behavioral therapy. https://www.brainline.org/treatment-hub/cognitive-behavioral-therapy-cbt
- Morrison, E. H., Cooper, D. B., Kennedy, J. E., Peskind, E. R., Cherman, T. S., & Yurgil, K. A. (2012). Desynchrony as a pathological outcome to traumatic brain injury. Translational Research in TBI, 2, Article 100109.
- StatPearls. (2023). Posttraumatic headache. https://www.ncbi.nlm.nih.gov/books/NBK556134
- Concussion Alliance. (2019). Cognitive behavioral therapy. https://www.concussionalliance.org/cognitive-behavioral-therapy
- Cognitive FX. (2025). TBI sleep problems: Causes and treatment. https://www.cognitivefxusa.com/blog/tbi-sleep-problems-causes-and-treatment
- Defense Health Agency. (2024). Managing headaches following a concussion: fact sheet. https://health.mil/Reference-Center/Fact-Sheets/2024/03/06/Managing-Headaches-Following-Concussion-Fact-Sheet
- Cattelani, R., Zettin, M., & Zoccolotti, P. (2019). Psychological intervention in traumatic brain injury patients: An overview. Behavioural Neurology, 2019, Article 4182958. https://doi.org/10.1155/2019/4182958
- Rasmussen, L. J. H., Caspi, A., Ambler, A., Broadbent, J. M., Cohen, H. J., d’Arbeloff, T., … & Moffitt, T. E. (2025). Neural correlates of fatigue after traumatic brain injury: Resting state and cognitive task performance. Brain Communications, 7(2), Article fcaf082.
- Bose, B., Katznelson, L., & Bose, S. (2013). Hypertension after severe traumatic brain injury: Friend or foe? Journal of Neurosurgical Anesthesiology, 25(4), 455-462.
- Huberman Lab. (2025). How to regulate your nervous system. https://www.hubermanlab.com/topics/regulate-your-nervous-system
- Mollayeva, T., D’Souza, A., Mollayeva, S., & Colantonio, A. (2024). Prevalence of fatigue and cognitive impairment after traumatic brain injury: An online population study. Archives of Physical Medicine and Rehabilitation, 105(6), 1145-1152.
- Faden, A. I., Chan, P. H., & Longar, S. (1987). Treatment of hypertension associated with head injury. Annals of Emergency Medicine, 16(5), 545-549.
- Jerath, R., Beveridge, C., & Barnes, V. A. (2023). Breathing practices for stress and anxiety reduction: Conceptual framework of implementation based on a systematic review of the published literature. Brain Sciences, 13(12), Article 1612.
- National Institute of Neurological Disorders and Stroke. (2023). Traumatic brain injury. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi
- Haarbauer-Krupa, J., Pugh, M. J., Prager, E. M., Harmon, N., Wolfe, J., & Yaffe, K. (2024). Prevalence of cardiovascular conditions after traumatic brain injury: A self-report study. Journal of the American Heart Association, 13(9), Article e033673.
- Hackensack Meridian Health. (2024). Reclaim your calm with nervous system regulation exercises. https://www.hackensackmeridianhealth.org/en/healthu/2024/08/06/how-to-use-nervous-system-regulation-exercises-to-reclaim-your-calm
- Headway. (2024). Cognitive effects of brain injury. https://www.headway.org.uk/about-brain-injury/individuals/effects-of-brain-injury/cognitive-effects-of-brain-injury
- Badjatia, N., Carney, N., Crocco, T. J., Fallat, M. E., Hennes, H. M., Jagoda, A. S., … & Vashi, N. (2024). Hypotension and adverse outcomes in moderate to severe traumatic brain injury: A TRACK-TBI study. JAMA Network Open, 7(11), Article e2447751.
- Brentwood Therapy Collective. (2025). How to regulate your nervous system: 7 science-backed tools. https://www.brentwoodtherapycollective.com/blog/how-to-regulate-your-nervous-system-science-backed-techniques-for-anxiety-and-stress
- Andelic, N., Hammergren, N., Bautz-Holter, E., Sveen, U., Brunborg, C., & Røe, C. (2022). Long-lasting pathological mental fatigue after brain injury—A complex symptom with individual features. Frontiers in Behavioral Neuroscience, 15, Article 791984.
- Cognitive FX. (2024). Why a concussion can lead to blood pressure change & POTS. https://www.cognitivefxusa.com/blog/pots-and-concussion-blood-pressure-changes
- Neurodivergent Insights. (2022). Nervous system reset: 13 effective ways to regulate and reground. https://neurodivergentinsights.com/13-ways-to-reset-your-nervous-system
- Mayo Clinic. (2021). Traumatic brain injury – Symptoms & causes. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- Harvard Medical School. (2024). Brain injury increases the risk of cardiovascular disease. https://hms.harvard.edu/news/brain-injury-increases-risk-cardiovascular-disease
- Cheng, K. (2024). The essential skill to regulate your nervous system [Video]. YouTube. https://www.youtube.com/watch?v=YcoIE3Yiaw0
- Royal Children’s Hospital Melbourne. (2024). Brain injury – Cognitive fatigue. https://www.rch.org.au/kidsinfo/fact_sheets/Brain_injury_Cognitive_fatigue
- US Department of Veterans Affairs. (2023). Traumatic brain injury carries risk for cardiovascular disease in post-9/11 veterans. https://www.research.va.gov/currents/0123-Traumatic-brain-injury-carries-risk-for-cardiovascular-disease-in-post-911-Veterans.cfm