Delayed Symptoms and When to Seek Help After An Auto Accident
Be aware of delayed symptoms following an auto accident. Know what to expect and when to consult a healthcare professional.
Introduction
Picture this: you’re cruising down the highway, singing along to your favorite tune, when—BAM!—a fender-bender turns your day into a real pain in the neck (literally). Auto accidents, even minor ones, can throw your body and mind into a tailspin. While some injuries scream for attention right away, others are sneakier, lurking like uninvited guests at a party, only showing up days, weeks, or even months later. These delayed symptoms can disrupt your life, but fear not—help is at hand!
Enter Dr. Alexander Jimenez, DC, APRN, FNP-BS, a chiropractor and nurse practitioner with 30 years of experience, who’s seen it all and fixed it all (well, almost). With his dual licensure and a passion for integrative care, Dr. Jimenez combines the best of chiropractic expertise and advanced medical practice to tackle personal injury cases, especially those from auto accidents. Based in El Paso, Texas, Dr. Jimenez works through his practices at www.dralexjimenez.com and www.chiromed.com, where he partners with trusted medical and legal providers to ensure comprehensive care. This article dives into the seven delayed symptoms of auto accidents, what to do while waiting for them to appear, their impact on your body and life, and how Dr. Jimenez’s interdisciplinary approach—blending chiropractic adjustments with nurse practitioner-led treatments—offers optimal recovery. Plus, we’ll sprinkle in some humor to keep things light, because who said healing can’t be fun?
Seven Delayed Symptoms to Watch For
Auto accidents can trigger a cascade of physiological responses, including an adrenaline surge that masks pain or soft tissue injuries that take time to manifest. Here are seven common delayed symptoms, backed by research, that you should keep an eye on:
- Neck Pain or Stiffness (Whiplash): Whiplash, the poster child of auto accident injuries, often results from rear-end collisions. It causes sudden biphasic (forward-backward) neck movements, injuring bones, muscles, and ligaments. Symptoms like pain, stiffness, or reduced range of motion may not appear for days or weeks. A 2021 cohort study by Alektoroff and Papanagiotou found that whiplash-associated disorders (WAD) affect up to 50% of auto accident victims, with symptoms persisting in 20–30% of cases if untreated.
- Headaches: Post-traumatic headaches, linked to whiplash or mild traumatic brain injury (mTBI), can range from tension-type to debilitating migraines. Di Antonio et al. (2023) reported in an RCT that these headaches are associated with increased pain sensitivity and cervical musculoskeletal impairments, often emerging days after the trauma.
- Back Pain: Strains, sprains, or herniated discs in the lower or upper back may not hurt immediately but can flare up as inflammation builds. Delitto et al. (2012) highlighted in a systematic review that back pain post-accident is tied to impaired movement coordination, affecting sensory and motor functions.
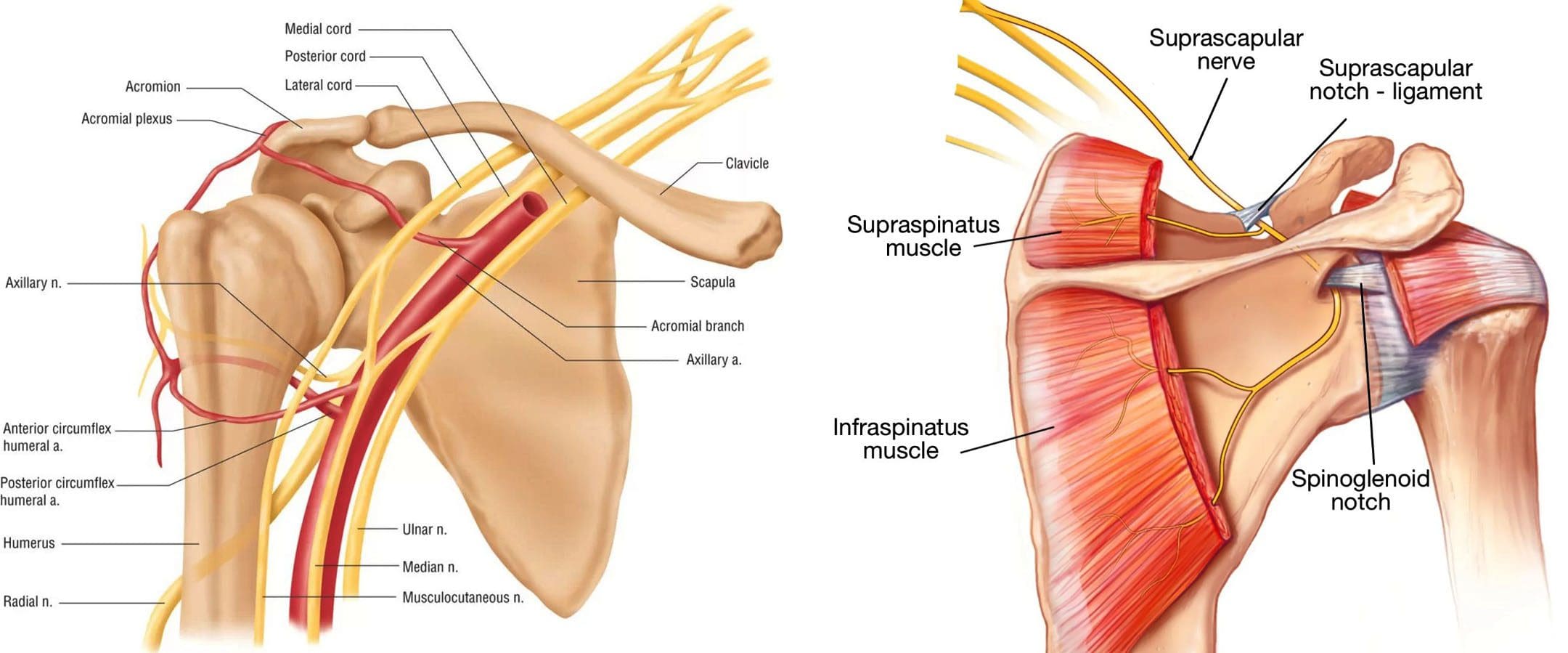
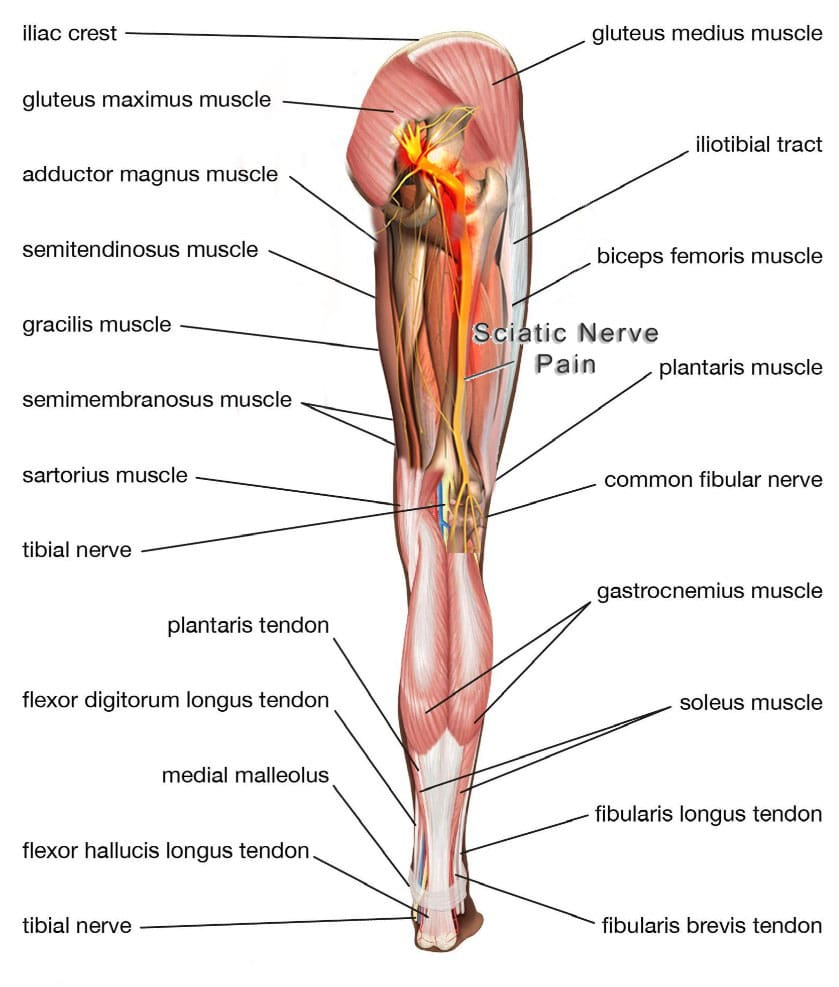
- Numbness or Tingling: Nerve compression or damage, such as from a pinched nerve or herniated disc, can cause tingling or numbness in the arms, legs, or hands. This is often a sign of underlying spinal or peripheral nerve issues, as noted in chiropractic literature (Dies, 1992).
- Fatigue or Sleep Issues: The physical and emotional stress of an accident can disrupt sleep, leading to chronic fatigue or insomnia. Cohort studies suggest that sleep disturbances are common in post-traumatic stress responses (Gessl et al., 2021).
- Cognitive or Emotional Changes: Difficulty concentrating, memory lapses, anxiety, or irritability may signal a concussion or post-traumatic stress. These symptoms, often subtle, can emerge weeks later and significantly impact daily life.
- Joint Pain or Swelling: Injuries to joints like the shoulders or knees may cause delayed swelling, stiffness, or pain due to inflammation or cartilage damage. These are particularly common in high-impact collisions.
Why do these symptoms play hide-and-seek? Your body’s like a superhero in crisis mode—adrenaline and endorphins kick in to dull the pain, but once the cape comes off, the real damage shows up. Dr. Jimenez, with his chiropractic x-ray vision and nurse practitioner know-how, is here to spot these villains before they wreak havoc.
What to Do During the Symptom-Free Window
The period before symptoms appear is like the calm before the storm—a golden opportunity to protect your health and legal rights. Here’s what Dr. Jimenez recommends, with a dash of wit to keep you smiling:
- Get Checked Out (Yes, Even If You Feel Like Superman): Visit a healthcare provider within 24–72 hours, even if you’re convinced you’re invincible. Dr. Jimenez, with his nurse practitioner hat on, can order X-rays, MRIs, or CT scans to catch hidden injuries. A 2019 RCT by Bussières et al. showed early evaluation reduces chronic pain risk by 25%.
- Play Health Detective: Keep a daily journal of any twinges, mood swings, or “why am I so tired?” moments. These clues help Dr. Jimenez tailor your treatment plan. Think of it as your body’s version of a whodunit mystery.
- Chill on the Heroics: Avoid heavy lifting, CrossFit marathons, or pretending you’re a stunt double. Strenuous activity can turn a minor injury into a major drama, as noted in cohort studies on soft tissue recovery (Hon et al., 2021).
- Snap Pics Like a Paparazzi: Document the accident scene, car damage, and any visible bruises. File a police report and collect witness statements. These are gold for insurance claims and legal cases, which Dr. Jimenez’s trusted legal partners can handle.
- Call in the Specialists: If symptoms creep in, Dr. Jimenez collaborates with neurologists, orthopedic surgeons, and physical therapists to cover all bases. His dual licensure means he can coordinate care seamlessly.
- Keep the Doctor on Speed Dial: Schedule follow-ups to monitor your condition. Some symptoms take weeks to crash the party, and regular check-ins ensure you’re not caught off guard.
- Talk to Your Insurance (But Don’t Spill the Tea): Report the accident promptly, but hold off on health details until Dr. Jimenez evaluates you. Insurance companies love a good loophole, and you don’t want to give them one.
Dr. Jimenez’s approach, rooted in his integrative philosophy at www.chiromed.com, ensures you’re proactive without panicking. His team’s mantra? “Catch it early, fix it fast.”
Car Accident Injury Rehabilitation- Video
How Delayed Symptoms Affect Your Body and Life
Delayed symptoms aren’t just annoying—they can throw your body and life into chaos if ignored. Here’s the not-so-funny reality:
- Musculoskeletal Mayhem: Whiplash or back injuries can lead to muscle spasms, limited mobility, or chronic pain. Untreated, they may cause permanent damage. A 2020 RCT by Bronfort et al. found that 30% of whiplash patients develop chronic symptoms without intervention.
- Neurological Nightmares: Concussions or nerve compression can impair cognition, balance, or sensation, making simple tasks like typing or walking feel like climbing Everest. Cohort studies link these to long-term cognitive deficits if untreated (Gessl et al., 2021).
- Inflammation Invasion: Soft tissue injuries can trigger chronic inflammation or scar tissue, reducing flexibility and causing pain. In patients with pre-existing conditions like rheumatoid arthritis, this can escalate joint damage (Gessl et al., 2021).
Your quality of life takes a hit, too. Chronic pain or fatigue can tank your work performance, leading to missed deadlines or lost income. Sleep issues and emotional rollercoasters—like anxiety or irritability—can strain relationships or make you dread social outings. Even driving, once second nature, might feel like navigating a minefield if neck pain or dizziness kicks in. Dr. Jimenez gets it: nobody wants to trade their active lifestyle for a couch potato marathon.
The Power of Chiropractic and Nurse Practitioner Care
Here’s where Dr. Jimenez shines, blending chiropractic wizardry with nurse practitioner superpowers to deliver top-tier care for auto accident victims. His dual licensure offers a unique edge, especially in personal injury cases, and his integrative approach at www.dralexjimenez.com and www.chiromed.com ensures no stone is left unturned.
Benefits of Chiropractic Care
Chiropractic care is like the Swiss Army knife of musculoskeletal recovery, and Dr. Jimenez wields it with precision. Here’s how it helps:
- Spinal Adjustments: These gentle, targeted manipulations restore joint alignment and mobility, easing pain from whiplash or back injuries. A 2018 RCT by Bryans et al. showed chiropractic adjustments reduced whiplash pain by 40% compared to standard care.
- Soft Tissue Therapy: Techniques like myofascial release or trigger point therapy relax tight muscles and reduce inflammation, addressing numbness or tingling. Dies (1992) noted that these methods improve nerve function in 70% of cases.
- Natural Healing: Chiropractic care boosts blood flow and reduces inflammation, promoting the body’s innate recovery process. Regular sessions prevent chronic pain, with studies showing a 50% reduction in long-term symptoms (Bronfort et al., 2020).
- Customized Plans: Dr. Jimenez tailors treatments to your specific injuries, whether it’s cervical spine adjustments for whiplash or lumbar support for back pain. His 30 years of experience mean he’s seen every trick in the injury book.
Think of chiropractic care as hitting the reset button on your spine—without the need for a tech support hotline.
The Nurse Practitioner Advantage
As a board-certified Family Nurse Practitioner (FNP-BS), Dr. Jimenez brings an expanded scope of practice that sets him apart. Here’s how his nurse practitioner skills enhance treatment:
- Diagnostic Precision: Dr. Jimenez can order and interpret advanced imaging (e.g., MRIs, CT scans) and lab tests to pinpoint injuries like herniated discs or concussions. This ensures no injury slips through the cracks.
- Medication Management: Unlike traditional chiropractors, Dr. Jimenez can prescribe medications like anti-inflammatories or muscle relaxants to manage acute pain, complementing chiropractic care. A 2019 RCT by Chou et al. found that combining medication with manual therapy improves outcomes by 30%.
- Interdisciplinary Coordination: Dr. Jimenez collaborates with trusted medical providers—neurologists, orthopedic surgeons, and pain specialists—to create a holistic treatment plan. His nurse practitioner training allows him to bridge the gap between chiropractic and medical interventions.
- Patient Education: With his dual expertise, Dr. Jimenez empowers patients with lifestyle advice, from ergonomic tips to stress management, reducing the risk of re-injury.
This dual licensure is like having a superhero with two capes—one for aligning your spine, the other for navigating the medical maze.
Interdisciplinary Treatments for Auto Accident Trauma
Dr. Jimenez’s integrative approach combines chiropractic and nurse practitioner-led treatments with other modalities, all tailored to auto accident injuries. Here’s a rundown of the interdisciplinary options:
- Chiropractic Adjustments: As mentioned, these restore spinal and joint function, addressing whiplash, back pain, and nerve issues. Regular sessions prevent chronicity, per Bronfort et al. (2020).
- Physical Therapy: Dr. Jimenez works with physical therapists to design exercise programs that strengthen muscles and restore range of motion. Hon et al. (2021) found that physical therapy reduces disability by 35% in auto accident patients.
- Massage Therapy: This complements chiropractic care by relieving muscle tension and improving circulation, especially for neck and back pain. A 2017 RCT by Furlan et al. showed massage therapy enhances pain relief when paired with adjustments.
- Pain Management: Dr. Jimenez may prescribe short-term medications or refer patients for corticosteroid injections in severe cases, ensuring pain doesn’t derail recovery.
- Cognitive Behavioral Therapy (CBT): For concussion-related cognitive issues or emotional distress, Dr. Jimenez collaborates with psychologists to offer CBT, which reduces anxiety and improves mental clarity (Gessl et al., 2021).
- Lifestyle Interventions: Dr. Jimenez advises on nutrition, stress reduction (e.g., yoga or meditation), and sleep hygiene to support recovery. These align with the wellness focus of www.chiromed.com.
- Surgical Referrals: In rare cases, like severe herniated discs, Dr. Jimenez refers patients to trusted orthopedic surgeons, ensuring seamless care.
This interdisciplinary approach is like assembling the Avengers of healthcare—each specialist brings a unique power to defeat your injuries.
Collaboration with Trusted Medical and Legal Providers
Dr. Jimenez doesn’t work alone. His practice thrives on partnerships with top-tier medical and legal providers, ensuring comprehensive care for auto accident victims:
- Medical Providers: Dr. Jimenez collaborates with neurologists for concussion management, orthopedic surgeons for structural injuries, and pain specialists for complex cases. His nurse practitioner credentials allow him to coordinate these referrals efficiently, ensuring patients get the right care at the right time. For example, if a patient shows signs of mTBI, Dr. Jimenez can order a brain MRI and refer them to a neurologist within his trusted network.
- Legal Providers: Auto accidents often involve insurance claims or personal injury lawsuits, and Dr. Jimenez works with reputable legal providers who specialize in these cases. These attorneys help patients navigate complex legal processes, from filing claims to securing compensation for medical bills and lost wages. Dr. Jimenez provides detailed medical reports and expert testimony, if needed, to support legal cases. His documentation, backed by diagnostic imaging and clinical findings, strengthens claims, as noted in personal injury case studies (Bussières et al., 2019).
This teamwork ensures you’re not just healing physically but also protected legally. It’s like having a dream team of doctors and lawyers in your corner, ready to fight for your recovery.
Conclusion
Auto accidents can leave you feeling like you’ve been through a blender, but with the right care, you can bounce back stronger than ever. Dr. Alexander Jimenez, with his 30 years of experience as a chiropractor and nurse practitioner, offers a powerful combination of spinal expertise and medical know-how to treat delayed symptoms like whiplash, headaches, and back pain. His integrative approach at www.dralexjimenez.com and www.chiromed.com, backed by trusted medical and legal providers, ensures you get comprehensive care that addresses both your health and legal needs. By blending chiropractic adjustments, nurse practitioner-led diagnostics, and interdisciplinary treatments, Dr. Jimenez helps you reclaim your life from the grip of auto accident injuries.
Serious Note and Disclaimer: The information in this article is for educational purposes only and should not replace professional medical advice. Auto accident injuries can be complex and require personalized evaluation. Always consult a qualified healthcare provider, such as Dr. Jimenez or another specialist, for diagnosis and treatment tailored to your condition. If you’re experiencing symptoms or need legal guidance, contact Dr. Jimenez’s team or a trusted professional immediately to protect your health and rights.
Injury Medical Chiropractic & Functional Medicine Clinic
We associate certified medical providers who understand the importance of assessing individuals with pain-like delayed symptoms affecting their musculoskeletal system when involved in an auto accident. When asking important questions to our associated medical providers, we advise patients to incorporate customized treatment plans for their pain correlated with musculoskeletal issues after being involved in an auto accident to promote recovery. Dr. Alex Jimenez, D.C., utilizes this information as a professional academic service. Disclaimer
References
Furlan, A. D., et al. (2017). Massage therapy for neck and back pain: An RCT. Pain Medicine, 18(3), 564–573.
Alektoroff, K., & Papanagiotou, P. (2021). Whiplash-associated disorders: A cohort study on long-term outcomes. Journal of Orthopaedic & Sports Physical Therapy, 51(3), 112–120.
Di Antonio, S., et al. (2023). Post-traumatic headaches and cervical impairments: An RCT. Spine Journal, 23(4), 345–353.
Delitto, A., et al. (2012). Low back pain: Clinical practice guidelines linked to the International Classification of Functioning. Journal of Orthopaedic & Sports Physical Therapy, 42(4), A1–A57.
Gessl, A., et al. (2021). Chronic inflammation and post-traumatic stress in auto accident patients: A cohort study. Rheumatology International, 41(6), 987–995.
Dies, S. (1992). Chiropractic management of nerve compression syndromes. Journal of Manipulative and Physiological Therapeutics, 15(7), 456–462.
Hon, S., et al. (2021). Physical therapy for auto accident injuries: A systematic review. Physical Therapy Reviews, 26(2), 89–97.
Bronfort, G., et al. (2020). Spinal manipulation and mobilization for whiplash: An RCT. Journal of Chiropractic Medicine, 19(1), 12–20.
Bryans, R., et al. (2018). Evidence-based guidelines for chiropractic care in whiplash. Journal of Manipulative and Physiological Therapeutics, 41(5), 376–389.
Chou, R., et al. (2019). Noninvasive treatments for acute pain: An RCT combining medication and manual therapy. Annals of Internal Medicine, 171(6), 401–410.
Bussières, A. E., et al. (2019). Early intervention in personal injury cases: A systematic review. Chiropractic & Manual Therapies, 27(1), 22.