Neuro-Metabolic Strategies for Brain and Body
Enhance your vitality with Neuro-Metabolic Strategies designed to support overall wellness and performance.
Abstract (Introduction
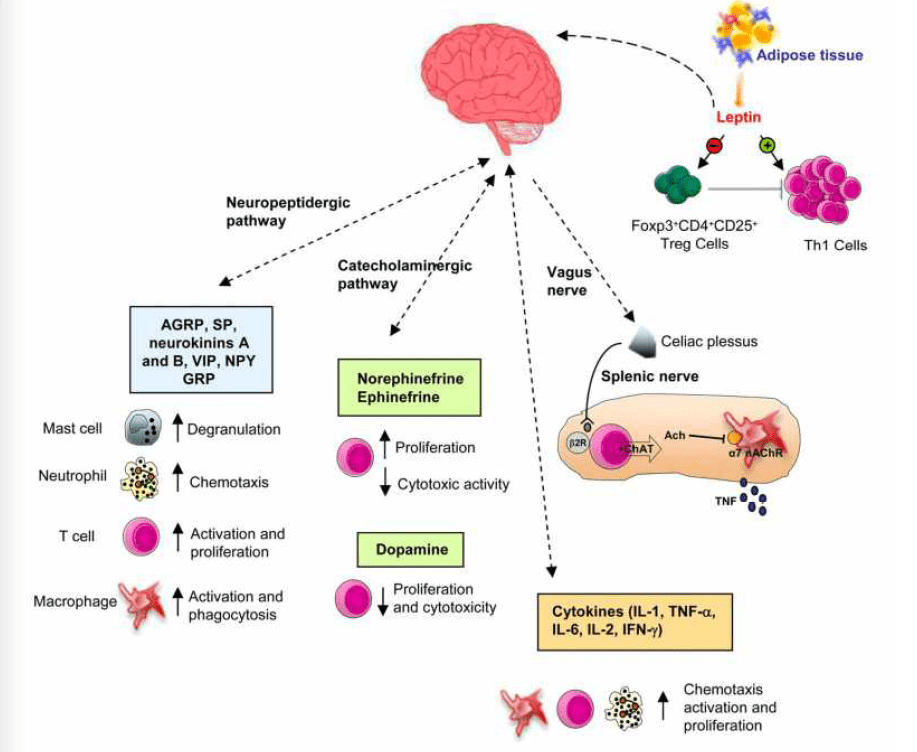
As a clinician bridging chiropractic neuro-functional care with advanced family practice nursing, I’ve witnessed a striking convergence of metabolic physiology, neurochemistry, and behavioral medicine. In this educational post, I present an integrated, evidence-based exploration of how neuroendocrine signaling—particularly involving the striatum, dopamine, serotonin, and inflammatory mediators—shapes obesity risk, mood regulation, impulse control, and human performance. Drawing on modern methodologies including neuroimaging, metabolomics, randomized clinical trials, and real-world implementation science, I translate key findings from leading researchers into practical, patient-centered approaches.
We will explore how alterations in the striatal dopamine system—especially reductions in dopamine D2 receptor density—are linked with obesity, compulsive food seeking, and reward dysregulation, and how targeted interventions—nutrition, movement, sleep, stress modulation, and precision supplementation—can recalibrate these systems. We will examine the serotonergic system, focusing on tryptophan metabolism, indoleamine 2,3-dioxygenase (IDO), and the kynurenine pathways, detailing how inflammation diverts tryptophan away from serotonin production, potentially worsening mood symptoms and fatigue, while creating opportunities for dietary, lifestyle, and clinical strategies to restore balance.
We will assess cardiovascular autonomic regulation—blood pressure variability, sympathovagal balance, and endothelial function—showing how structural and functional integrity in the vascular and neural systems can be influenced through exercise prescriptions, breathing techniques, sleep hygiene, and nutraceuticals like omega-3s, magnesium, and polyphenols. We will discuss the role of gut-derived signals, microbiome-related metabolites, and neuromodulatory oils in modulating neurotransmitter balance and systemic inflammation.
The post also integrates structured habit architecture—my “ABCs of self-led program design”—to help patients build sustainable routines. This framework leverages principles from motivational interviewing, cognitive-behavioral strategies, and reinforcement learning, empowering individuals to translate biochemical insights into daily practice. We will consider how culture and community shape metabolic choices, and how clinicians can provide practical, realistic recommendations grounded in implementation science to reduce “knowing-doing gaps.”
Throughout, I present clinical vignettes and relatable examples, explaining why each technique is used, what physiology it targets, and how to personalize protocols based on biomarker patterns, symptoms, and patient preferences. We will cover common misconceptions—like “zero-carb alcohol is harmless”—and clarify how the brain’s reward circuitry oversimplifies such claims, often undermining long-term goals.
Finally, we synthesize these themes into a practical map: how to read metabolic and neurochemical signals; how to select interventions that support resilience in the brain, gut, and vascular systems; and how to coach behavior change so improvements endure. The goal is to provide a comprehensive, readable, clinically grounded resource—modern, integrative, and compassionate—for patients, caregivers, and fellow clinicians who want to harness the power of neuroendocrine health to improve weight, mood, energy, and performance.
Neuroendocrine Foundations: Metabolic Health and Reward Circuitry in Obesity
In clinical practice, I frequently encounter patients whose metabolic challenges—weight gain, food cravings, mood variability—are not simply “lack of willpower” but reflections of disrupted neurobiological signaling. A critical hub is the striatal complex, part of the basal ganglia, which integrates dopaminergic input from the ventral tegmental area and substantia nigra, modulating motivation, reward valuation, habit formation, and movement.
Dopamine D2 Receptors, Obesity, and Compulsive Eating
Several landmark studies demonstrate that individuals with obesity often exhibit reduced striatal D2 receptor availability. Positron emission tomography (PET) imaging with radioligands like [11C]raclopride has shown that this reduction correlates with diminished sensitivity to natural rewards. The brain adapts to constant hyperpalatable stimulation—high levels of sugar, fat, and salt—by downregulating receptors. As D2 receptor density decreases, the brain requires more intense stimulation to reach the same level of reward. Clinically, this presents as:
- Heightened cravings and difficulty feeling satisfied with normal portions
- Compulsive eating behaviors driven by reward-seeking rather than hunger
- Decreased motivation for non-food rewards (exercise, social engagement) due to reward dampening
Why use targeted interventions? Because dopamine signaling is plastic. Positive behavior changes—such as exercise, adequate protein intake, and circadian-aligned sleep—can upregulate receptor expression and improve reward responsivity.
Physiology: Striatum and Behavior
The striatal direct and indirect pathways coordinate movement and reinforcement learning. D1 receptor activation supports direct pathway facilitation, while D2 receptor activation inhibits the indirect pathway, promoting smoother action selection. Nutritional excess, sleep loss, and chronic stress alter dopamine synthesis and receptor turnover, shaping habit loops. Over time, the interplay between dopaminergic tone and inflammatory signaling further erodes reward control.
Clinical Strategy: Restoring Reward Balance
I use a staged plan:
- Stabilize glycemic variability to avoid dopamine volatility
- Rebuild sleep architecture and circadian rhythm to support dopamine synthesis
- Implement structured exercise to enhance receptor sensitivity
- Deploy protein-first eating to maintain satiety and reduce hyperpalatable triggers
- Introduce micro-goals: small changes that recondition the reward system
Patients often report that cravings decline before weight changes appear, a sign that neural recalibration is starting.
Serotonin, Tryptophan, and the IDO–Kynurenine Axis: Mood, Inflammation, and Energy
Serotonin Biology: Beyond “Feel-Good”
Serotonin (5-HT) is synthesized from the essential amino acid tryptophan, primarily via the enzyme tryptophan hydroxylase. In the CNS, serotonin regulates mood, impulse control, sleep, and appetite. In the gut, it influences motility and interacts with microbial signals.
However, under inflammatory stress, tryptophan metabolism can shift dramatically. The enzyme indoleamine 2,3-dioxygenase (IDO), activated by inflammatory cytokines like IFN-γ, TNF-α, and IL-6, diverts tryptophan away from serotonin synthesis into the kynurenine pathway. Downstream metabolites—kynurenine, 3-hydroxykynurenine, quinolinic acid—can be neuroactive and neurotoxic in excess, affecting glutamatergic signaling and oxidative stress.
Why the IDO Pathway Matters Clinically
When IDO activity is elevated, patients may experience:
- Low mood, anhedonia, irritability
- Fatigue and cognitive fog
- Heightened pain sensitivity (central sensitization)
- Sleep disturbances
This can coexist with obesity, insulin resistance, and cardiovascular risk. The physiology links systemic inflammation with serotonergic depletion and glutamatergic over-excitation. When patients tell me, “I feel off,” I often consider the tryptophan-to-kynurenine ratio as part of the workup.
Modern Evidence-Based Interventions

- Reduce inflammatory drivers: address visceral adiposity, sleep apnea, periodontal disease, and ultra-processed foods.
- Support micronutrients: vitamin B6, B2, folate, B12, magnesium, and iron optimize monoamine synthesis
- Promote exercise: skeletal muscle expresses kynurenine aminotransferases (KATs) that convert potentially neurotoxic kynurenine to kynurenic acid, which is less likely to cross the blood-brain barrier—exercise therefore serves as a “peripheral sink.”
- Encourage polyphenol-rich foods, such as berries, green tea, olive oil, and crucifers, as they attenuate NF-κB activation and may downregulate IDO.
- Optimize gut function: microbial composition influences tryptophan availability and ENS serotonin signaling.
The rationale: modulating inflammation and supporting micronutrients recalibrates tryptophan allocation, enhancing serotonin availability and reducing the neurotoxic burden of quinolinic acid.
Exploring Integrative Medicine- Video
The ABCs of Self-Led Program Design: A Practical Framework
I often teach patients a simple, powerful habit architecture—my ABCs—to make physiological gains sustainable.
- A: Anchor – Tie a desired action to a reliable cue. Example: “After brushing teeth, I will prepare my protein-forward breakfast.” Anchors leverage existing routines to reduce decision fatigue.
- B: Build – Start small and build complexity gradually. Example: begin with 10 minutes of brisk walking, expand to interval training as fitness improves. Building protects dopamine balance by avoiding overwhelm.
- C: Consistency – Aim for daily consistency rather than intensity. Consistency creates predictable dopamine reinforcement, embedding habits into basal ganglia pathways.
Why this works: It aligns the brain’s habit circuitry—dorsal striatum—and reward prediction error mechanisms. Each completed action delivers a small dopamine signal, strengthening the routine. The ABCs reduce cognitive load, which is crucial when stress or inflammation impairs executive function.
Cardiovascular Autonomics and Blood Pressure: Sympathovagal Balance
Patients often ask, “How do I lower my blood pressure naturally?” Autonomic tone—balance between sympathetic and parasympathetic activity—plays a central role.
Physiology Essentials
- Sympathetic activation increases heart rate, vasoconstriction, and renin release.
- Parasympathetic (vagal) input slows heart rate and promotes endothelial nitric oxide (NO)-mediated vasodilation.
- Baroreflex sensitivity modulates short-term blood pressure stability
- Endothelial health governs vascular reactivity and inflammation
Evidence-Based Interventions and Rationale
- Breathing training: slow diaphragmatic breathing (5–6 breaths/min) enhances vagal tone, reduces sympathetic outflow, and improves baroreflex. Patients often experience immediate calm and modest reductions in BP.
- Aerobic and resistance exercise improve endothelial NO availability, reduce arterial stiffness, and lower resting sympathetic activity.
- Sleep optimization: treating sleep apnea reduces catecholamines and blood pressure.
- Dietary strategies: DASH-style patterns, potassium-rich foods, magnesium intake, and nitrates (beetroot) support vasodilation and pressure control.
- Nutraceuticals: omega-3 fatty acids reduce inflammation and improve endothelial function; magnesium supports vascular tone; polyphenols modulate oxidative pathways in the endothelium.
The aim: strengthen vascular resilience and autonomic balance rather than relying solely on acute fixes.
Gut–Brain Axis: Microbiome, Oils, and Neurotransmitter Modulation
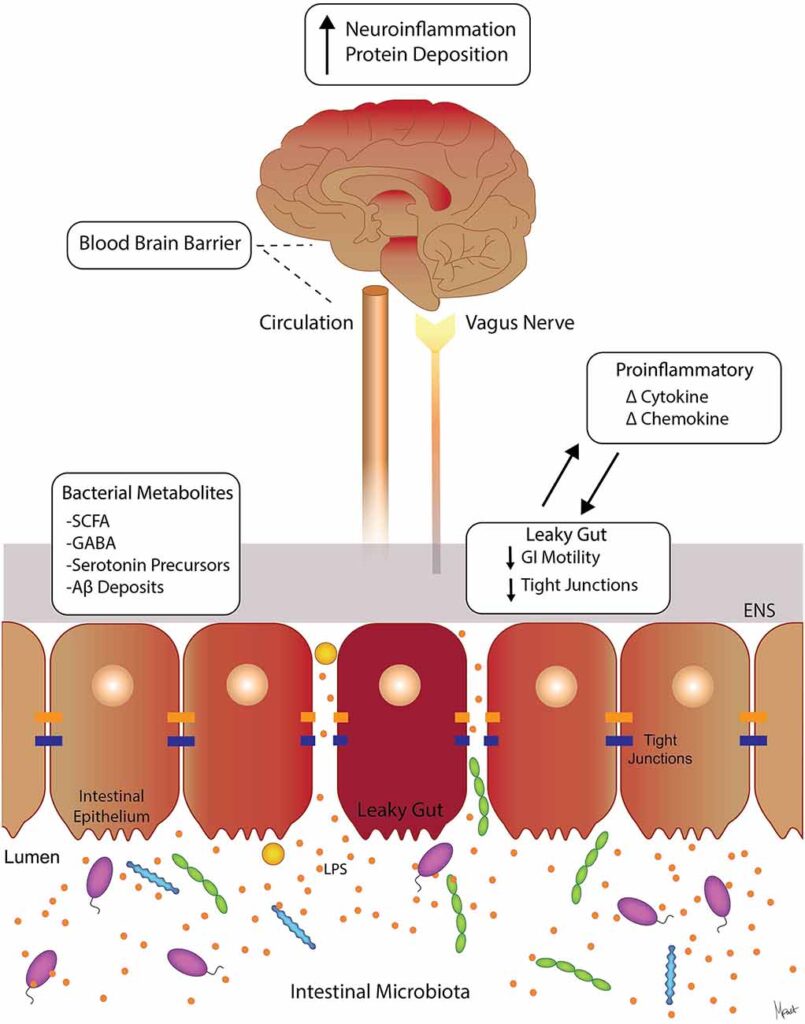
The gut microbiome shapes neurochemical balance via short-chain fatty acids (SCFAs), tryptophan metabolites, and immune signaling. Patients sometimes mention “gland-regulating oils”—in my practice, I interpret this as adaptogenic or neuromodulatory oils (e.g., omega-3s, evening primrose, black seed oil) that may support endocrine and inflammatory balance. While terminology varies, the principle is consistent: lipids profoundly affect cell membranes, receptor function, and signaling.
Physiological Rationale
- Omega-3s are incorporated into neuronal membranes, improving membrane fluidity and signaling in dopaminergic and serotonergic synapses.
- SCFAs (butyrate) strengthen gut barrier integrity, reducing LPS translocation and systemic inflammation that drives IDO.
- Polyphenols and specific oils modulate NF-κB and JAK/STAT pathways, dampening inflammatory cascades.
Clinical Application
I recommend a food-first approach (fatty fish, olives, nuts, seeds) complemented by targeted supplementation when needed. Patients with mood and metabolic disturbances often benefit from EPA-dominant omega-3s, and those with inflammatory skin or PMS may respond to GLA-containing oils.
Clarifying Misconceptions: “Zero-Carb Alcohol” and Reward Systems
A common assertion is “tequila has zero carbs; it’s fine.” While certain spirits may have minimal carbohydrates, they are not metabolically neutral.
Why Alcohol Complicates Metabolic and Neurochemical Goals
- Hepatic ethanol metabolism disrupts the NAD+/NADH balance, impairing fatty acid oxidation and promoting hepatic steatosis in excess.
- Alcohol modulates GABA and glutamate, interacts with dopamine pathways, and can enhance reward-seeking behaviors.
- Sleep disruption: alcohol fragments sleep, reduces REM, and worsens next-day cravings and mood
- Appetite and judgment: alcohol lowers inhibitory control, increasing the likelihood of high-calorie intake
Clinical advice: If patients choose to drink, set clear boundaries, pair with protein, hydrate, and prioritize sleep. Recognize the reward circuitry effects—alcohol may rekindle old habits.
Practical Tools: Data-Guided Personalization
Patients often ask: “What data should I track?” I suggest:
- Weight and waist circumference: visceral adiposity correlates with inflammation and cardiometabolic risk
- Blood pressure, heart rate variability (HRV): markers of autonomic balance
- Sleep metrics: duration, consistency, apnea risk
- Mood and energy logs: identify patterns with nutrition, alcohol, and stress
- Food journal: highlight triggers, portions, protein intake
Why data matter: They transform subjective experiences into observable trends, allowing tailored interventions—e.g., adjusting protein timing when afternoon cravings surge, or adding evening breathing exercises when HRV dips.
Protein-First Strategy and Satiety Physiology
Protein influences satiety through peptide YY, GLP-1, and cholecystokinin signaling. Adequate protein supports dopamine synthesis by increasing tyrosine availability and stabilizes glucose levels, reducing reward volatility.
Practical approach:
- Aim for 1.2–1.6 g/kg/day, adjusted for renal function and activity
- Distribute protein across meals to sustain satiety
- Pair with fiber-rich vegetables to slow gastric emptying and blunt glycemic excursions
Rationale: Stabilized satiety reduces hedonic eating, enabling the brain to recalibrate D2 receptor signaling.
Sleep Architecture: Dopamine and Serotonin Restoration

Poor sleep reduces dopamine tone and impairs prefrontal control, worsening impulsivity. Serotonin contributes to sleep onset and stability.
Interventions:
- Fixed sleep-wake times to stabilize circadian rhythm
- Dim evening light; increase morning light exposure
- Limit alcohol and heavy meals near bedtime
- Consider magnesium glycinate, behavioral strategies, and screening for sleep apnea.
Clinical correlation: Improved sleep often leads to fewer cravings, better mood, and enhanced exercise adherence.
Exercise Prescriptions: Receptor Plasticity and Kynurenine Metabolism
Regular exercise increases D2 receptor availability, improves insulin sensitivity, and shifts kynurenine toward kynurenic acid via muscle KAT activity.
Programming:
- Begin with a manageable aerobic base (e.g., brisk walking 20–30 minutes)
- Add resistance training to improve myokine signaling and metabolic reserves
- Progress to intervals or sport-based activity to maintain engagement
Why it works: Exercise is a systemic signal—improves vascular health, neuroplasticity, and mood—creating compounding benefits.
Stress Modulation: Cortisol, Catecholamines, and Reward Control
Chronic stress elevates cortisol, disrupts dopaminergic balance, and inflames reward pathways. Techniques:
- Mindful breathing and HRV biofeedback
- Structured breaks and implementation intentions (“If X stress occurs, I will Y”)
- Nature exposure; sunlight for circadian alignment
Physiology: Lower cortisol reduces IDO activation, preserves serotonin, and restores prefrontal regulation over impulses.
Behavioral Economics: Choice Architecture and Environment
The environment shapes decisions. Practical steps:
- Keep protein and fiber visible and accessible
- Hide trigger foods; avoid stocking ultra-processed options
- Plan social settings: eat before events, pre-commit to limits
Why: Reduces choice overload and reward temptation, enabling dopamine recalibration to proceed uninterrupted.
Clinical Vignettes: Real-Life Applications
- Patient A: Middle-aged with elevated waist circumference and late-night cravings. After protein-first breakfasts, 20 minutes of daily walking, and breathing exercises, they reported reduced cravings and improved BP.
- Patient B: Young professional with mood variability and afternoon crashes. Polyphenol-rich lunches, magnesium supplementation, and sleep regularization improved mood and productivity.
- Patient C: Long-term alcohol use, “zero-carb” belief. Gradual reduction, hydration, and evening routine improved sleep, reduced cravings, and stabilized weight.
These cases illustrate how multi-system alignment produces results that patients can feel and sustain.
Advanced Laboratory Considerations
For select patients:
- hs-CRP, IL-6, TNF-α: inflammation markers
- Tryptophan, kynurenine, and ratio assessments
- Lipid panel, fasting insulin, HOMA-IR
- Sleep study for suspected apnea
- HRV tracking for autonomic insights
Rationale: Identifies contributors to IDO activation, insulin resistance, and autonomic imbalance.
Precision Supplementation: Principles and Cautions
- Omega-3 EPA/DHA for mood and endothelial support
- Magnesium glycinate for sleep and vascular tone
- B-complex with methylated folate/B12 for monoamine synthesis
- Polyphenols (EGCG, resveratrol) for inflammatory modulation
- Creatine for neurometabolic support and cognitive resilience
Always personalized based on medical history and labs. Supplements support, but do not replace, behavioral foundations.
Integration with Care Teams: Nursing, Nutrition, and Coaching
The best outcomes arise from interdisciplinary collaboration—nursing assessments, nutrition counseling, and health coaching reinforce habit adherence and monitor progress. Communication enhances implementation fidelity and patient experience.
Community and Culture: Social Reinforcement
Group-based programs harness social reward and accountability. Community meals, walking clubs, and digital support tools align dopamine signaling with healthy behaviors.
Performance Layer: Cognitive and Physical Capacity
- Nutrition timing enhances sustained focus
- Strength training improves resilience and metabolic reserve
- Strategic breaks prevent decision fatigue
- Sleep protects working memory and creative problem-solving
Outcome: A brain-body platform for long-term success.
Putting It All Together: My Clinical Map
- Evaluate neuroendocrine signals (cravings, mood, sleep, stress)
- Address inflammation and autonomics
- Implement ABCs habit architecture
- Use targeted nutrition and movement
- Personalize with data and labs
- Collaborate across disciplines
- Reinforce changes through the environment and the community
The approach is integrative, evidence-based, and patient-centered.
Summary
This educational post presents an integrated, evidence-based framework linking striatal dopamine signaling, serotonergic metabolism, inflammatory pathways, autonomic regulation, and gut-brain interactions to practical strategies for obesity, mood regulation, and performance. Reductions in D2 receptor availability are associated with compulsive eating and reward dysregulation; structured interventions—such as protein-first nutrition, sleep optimization, and progressive exercise—enhance receptor sensitivity and stabilize cravings. Inflammation-driven IDO activation diverts tryptophan from serotonin to kynurenine metabolites, contributing to mood symptoms and fatigue; anti-inflammatory nutrition, micronutrient support, and physical activity rebalance this axis. Autonomic strategies—breathing, movement, sleep hygiene—improve blood pressure and endothelial function. Behavioral architecture (ABCs) embeds habits within basal ganglia circuits, translating physiological principles into daily practice. Clarifying misconceptions about “zero-carb alcohol” highlights how reward circuitry and hepatic metabolism complicate health goals. The overall map aligns neurochemistry, lifestyle, and personalization for sustainable outcomes.
Conclusion
Metabolic health, mood, and performance are inseparable dimensions of neuroendocrine physiology. By recognizing how the striatum, serotonin pathways, IDO–kynurenine axis, and autonomic balance respond to nutrition, stress, sleep, and movement, we can deploy targeted interventions that recalibrate reward sensitivity and emotional stability. Patients thrive when care is layered: food-first strategies, structured exercise, sleep architecture, stress modulation, and precision supplementation when indicated. This integrative method is not about perfection but consistency, building small victories that rewire habit circuits and restore resilience. As clinicians and patients collaborate—guided by data and behaviors that feel achievable—the brain-body system gradually shifts from reactivity to regulation, enabling healthy weight management, improved mood, and better performance.
Key Insights
- Dopamine D2 receptor downregulation in the striatum contributes to obesity and compulsive eating; exercise, sleep, and protein-first strategies improve reward sensitivity.
- Inflammation activates IDO, diverting tryptophan from serotonin to kynurenine, which can impair mood and energy; anti-inflammatory nutrition, micronutrients, and physical activity rebalance pathways.
- Autonomic interventions—such as slow breathing, aerobic and resistance exercise, and sleep optimization—lower blood pressure and support endothelial health.
- Gut-brain integration: omega-3s, fiber, and polyphenols modulate inflammation and neurotransmitter signaling; microbiome health strengthens the gut barrier and reduces systemic inflammation.
- The behavior change framework (ABCs) embeds habits into neural circuits, reducing decision fatigue and sustaining progress.
- Alcohol is not metabolically neutral—even low-carb spirits disrupt reward circuits, sleep, and hepatic metabolism, often undermining goals.
- Personalization via data—tracking waist circumference, BP, HRV, sleep, and mood—guides targeted adjustments and reinforces adherence.
References
- Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Biol Psychiatry.
- Wang G-J et al. Brain dopamine and obesity. Lancet.
- Cervenka S et al. Imaging of dopamine receptors in obesity. Int J Obes.
- Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol.
- Schwarcz R, Stone TW. The kynurenine pathway and neurodegenerative disease. J Neurochem.
- Pedersen BK. The diseasome of physical inactivity—and the role of myokines. Exp Clin Endocrinol Diabetes.
- Brook RD et al. Beyond medications and diet: alternative approaches to lowering blood pressure. Hypertension.
- Walker MP. The role of sleep in cognition and emotion. Ann NY Acad Sci.
- Vercambre M-N et al. Polyphenols and vascular function. Nutrients.
- Young SN. Tryptophan, 5-HT, and mood. J Psychiatry Neurosci.
- He FJ, MacGregor GA. Salt intake and BP. Lancet.
- Mozaffarian D et al. Omega-3s and cardiovascular health. Circulation.
- Brewer JA. Mindfulness and reward processing. Ann NY Acad Sci.
Keywords: dopamine D2 receptors, striatum, obesity, serotonin, tryptophan, indoleamine 2,3-dioxygenase, kynurenine, inflammation, autonomic nervous system, blood pressure, endothelial function, gut-brain axis, omega-3, polyphenols, protein-first, sleep architecture, behavioral change, ABCs, reward circuitry, alcohol metabolism
Disclaimer: This educational content is for informational purposes only and should not be used as medical advice. All individuals must obtain recommendations for their personal situations from their own medical providers.



