Bio-Regulatory Medicine for Longevity & Cellular Health
Learn how bio-regulatory medicine for cellular health can enhance your health and support your body’s natural functions.
Abstract: An Introduction to Advanced Cellular Restoration and Regenerative Medicine
Hello, I’m Dr. Alexander Jimenez, and I am honored to share my clinical experience and insights with you today. As a practitioner holding dual qualifications as a Doctor of Chiropractic (DC) and a Family Nurse Practitioner (FNP-APRN), my approach is rooted in a comprehensive, systems-based understanding of human physiology. My practice is dedicated to integrating the latest findings from leading researchers in the field, employing modern, evidence-based research methods to navigate the complex landscape of chronic illness, aging, and performance optimization. This educational post is designed to move beyond surface-level discussions and delve into the intricate biochemical and physiological mechanisms that govern our health. My goal is to present this information not as a rigid lecture but as an educational dialogue, sharing insights from modern, evidence-based research in a narrative format that is both comprehensive and relatable.
In the sections that follow, we will examine several key conceptual areas in detail. We will begin by exploring the pleiotropic nature of natural molecules and therapies, likening them to “Swiss Army knives” for their multifaceted ability to modulate inflammation, reduce fibrosis, protect cells, and orchestrate healing. We’ll explore why a single approach is often insufficient and how combining therapies such as peptides, light therapy, and advanced oxygen therapies can create a powerful synergistic effect. Central to this is the extracellular matrix (ECM) and the role of myofibroblasts in healing versus fibrosis.
Next, we will navigate the practical yet challenging aspects of clinical practice. I’ll share my personal methodology for ensuring patients can access necessary and affordable lab testing without jeopardizing their future insurability, emphasizing patient education and advocacy in today’s medical economy. We will also address the operational hurdles of integrating advanced therapies, including the prohibitive cost of certain equipment and the critical importance of proper technique and patient safety. This includes a deep dive into Extracorporeal Shockwave Therapy (ESWT), differentiating it from ultrasound and explaining how its mechanotransduction properties reboot stalled healing processes.
A significant portion of our discussion will be dedicated to the cutting edge of regenerative medicine. We will explore novel treatments, such as Dezawa MUSE cells, and clarify what makes these stress-enduring stem cells unique. This leads to an exploration of cellular memory and energetic transfer, examining how information can be stored in tissues. We will then apply these principles to clinical scenarios, including a detailed case study on managing post-traumatic osteoarthritis using a hierarchical approach that prioritizes foundational support before escalating to agents such as Thymosin Beta-4 (TB-500) and Body Protection Compound 157 (BPC-157). This underscores the principle of treating the individual rather than the diagnosis.
Finally, we will synthesize these concepts in a comprehensive, interactive case study analysis of a 45-year-old woman with a complex constellation of symptoms. We will deconstruct her case, analyze her lab work, and construct a logical, evidence-based treatment plan from the ground up, demonstrating how to identify root causes and apply targeted interventions such as Selank, Tesamorelin, and GLP-1 agonists. We will conclude by reviewing the remarkable clinical outcomes achievable with an integrated, patient-centered approach, demonstrating the profound impact of moving beyond symptom management to restore foundational health. This post is a comprehensive resource that offers a deeper appreciation of the intricate, interconnected nature of the human body and the powerful tools we have to foster true healing and vitality.
The Critical Importance of Sourcing and Clinical Integrity in Regenerative Medicine
Before we delve into the core scientific concepts, I feel it’s imperative to address a fundamental aspect of my practice and a cornerstone of responsible medicine: the integrity of our tools and the nature of the practitioner-patient relationship. In the world of regenerative therapies, especially with substances like peptides, the source is everything. My journey into this field wasn’t just academic; it was a boots-on-the-ground investigation.
It began over a decade ago when a representative from an online peptide company unexpectedly appeared in my office. He was selling powders, and this was long before peptides were a common topic of discussion in clinical circles. My curiosity was piqued not only by the products but also by the person and his story. This encounter set me on a path. I felt a profound responsibility to understand exactly what I might one day offer my patients. This wasn’t a responsibility I could delegate. I couldn’t just trust a website or a salesperson’s word.
So, I traveled. I accompanied this individual to MIT, where I connected with distinguished scientists at the Broad Institute in Cambridge. They were deeply immersed in translational medicine, working on bringing laboratory discoveries to clinical practice. They recognized my potential as a collaborator, a clinician willing to bridge that gap. But I knew I had to proceed with the utmost caution. I couldn’t afford to put my patients or my license at risk. This led me down a literal and figurative path of exploration—visiting facilities, sometimes in back alleys, to see the steel tables and the synthesis processes firsthand. I needed to know the conditions under which these compounds were produced to assess the quality control, or lack thereof.
My search for knowledge and quality extended to Europe, where I began meeting peptide science founders and researchers in 2016 and 2017. These were the pioneers, the people who had been studying these molecules for decades. I wasn’t just an attendee at a conference; I immersed myself in their world, becoming a friend and a trusted clinical colleague. They were researchers, and I was often the only clinician in the room, bringing real-world patient challenges to the table. For instance, I was working with a small, desperate group of patients with massive brain injuries who had exhausted all other options. I began using peptides such as BPC-157, then attended meetings with leaders in the field and learned that they had been using Thymosin peptides in humans since the 1960s. They had governmental permission in other countries to use these to keep children with DiGeorge’s Syndrome, a severe immunodeficiency, alive.
This entire experience solidified a core principle: I must know my source. I need to work with pharmacists and manufacturers who can guarantee purity, explain peptide isomers, and don’t change their formulations arbitrarily. This is why I build personal relationships with my suppliers. I visit them. It’s the same level of personal commitment I bring to my patients. If I am going to offer a treatment, I must be confident that I am providing the highest-quality, safest option available—the same Tender Loving Care (TLC) I would want for myself or my family.
Empowering Patients Through Education and Shared Decision-Making
This brings me to the second cornerstone: the patient’s role. I do not make decisions for my patients. My role is to educate, lay out the options, risks, benefits, and the current state of scientific understanding. The final decision always rests with the patient. This is the essence of informed consent.
I work with the medical board and am consistently impressed by their diligence, but I’m also aware of the risks practitioners take, sometimes without a full appreciation of the dangers. I once had a conversation with a colleague, a clinician and co-owner of a practice, who casually mentioned taking a powerful medication without a second thought. To me, this demonstrated a lack of appreciation for the profound biological impact of these substances. It’s far more dangerous than a simple cortisol shot, a procedure that itself is fraught with peril.
I’ve witnessed the devastating consequences of seemingly routine procedures. I think of a patient, a vibrant man of Italian heritage, a passionate tennis player, who developed a knee problem. His doctors, intending to help, administered a steroid injection. And then another. Within two months, the tissue had degraded so severely that he required open-knee surgery. This surgery, performed on a body now in a state of malnourishment from the catabolic effects of the steroids, initiated a downward spiral. He developed a bleeding disorder, became emaciated, and ultimately, he passed away. This tragic story is a stark reminder that even well-intentioned interventions can have catastrophic, unforeseen consequences.
Therefore, my approach is one of partnership. I never convince anyone to do anything. When a patient is hesitant or upset, I don’t push. I calmly state, “I understand that there are things you don’t yet understand, and that is okay. You are on your own journey. We need to determine where you want to be on that path. Right now, it seems we are not aligned. And if we’re not aligned, it’s not the right time for me to treat you.” I would love to help, but the foundation must be a participatory dialogue. When the patient is ready to have that conversation and engage as an equal partner, we can move forward. In medicine, especially when exploring the frontiers of regenerative therapies, we are always managing risk. The best we can do is to ensure that every decision is fully informed, deeply considered, and truly shared.
Fascia: The Unsung Hero of Healing and Communication
For decades, medical textbooks depicted fascia as little more than biological shrink-wrap—a passive, inert barrier that held our muscles and organs in place. We now know this view is profoundly outdated. Modern research, through advanced imaging and biomechanical studies, has revealed fascia as a dynamic, intelligent, and communicative system. It is a tensegrity structure, a complex, body-wide web of connective tissue that is intricately involved in every aspect of our physiology.
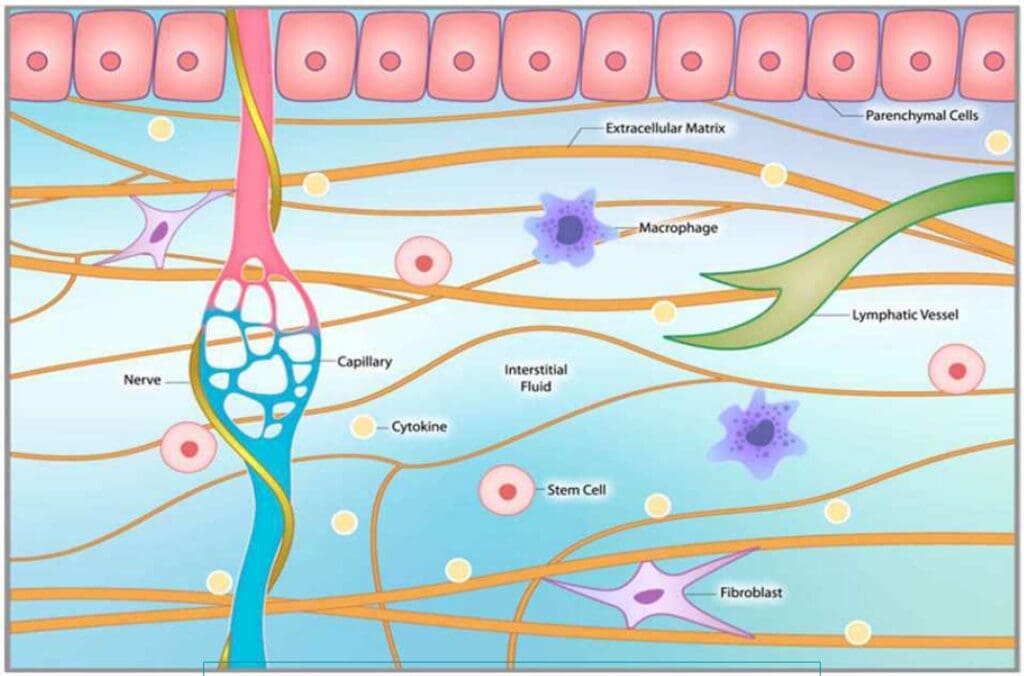
Fascia is not a passive barrier. It is the fundamental fabric of our extracellular matrix (ECM), the environment in which all of our cells live. This matrix is a bustling neighborhood composed of cells, signaling molecules, and structural proteins. The cells within the fascia, what they secrete, and the structural components they produce—such as collagen and elastin—collectively organize how our bodies heal. This process determines whether we successfully restore tissue integrity or are left with a dysfunctional scar. Understanding this is absolutely critical for any effective therapeutic intervention.
Myofibroblasts: The Architects and Potential Saboteurs of Healing
Within this fascial universe, a specific cell type plays the leading role in wound repair: the myofibroblast. When you sustain an injury—a cut, a tear, a strain—your body initiates a beautifully orchestrated inflammatory cascade. Local cells release signals that call fibroblasts to the site of injury. These fibroblasts are the workhorses of tissue repair. In response to specific mechanical and chemical cues, they differentiate into myofibroblasts.
These specialized cells are remarkable. They contain contractile filaments, much like those in smooth muscle cells, which allow them to physically pull the edges of a wound together. They are the architects of healing, diligently spinning a new scaffold of collagen to form a fibrin clot and bridge the damaged tissue. A little bit of this organized scarring is essential for survival. It provides a quick, strong patch to maintain structural integrity.
The problem arises when this process doesn’t turn off. If the inflammatory signals persist—due to chronic injury, systemic inflammation, or metabolic dysfunction—the myofibroblasts remain activated. They continue to churn out collagen relentlessly. This is when healing goes awry. The organized, functional scaffold of a healthy scar devolves into a dense, disorganized, and restrictive mass of fibrotic tissue. This is the cytokine storm that creates a vicious cycle. The thick tissue restricts blood flow, trapping waste products and preventing nutrients from reaching the cells. This hypoxic and toxic environment triggers more inflammation, which in turn activates more myofibroblasts, leading to more fibrosis. The tissue loses its elasticity and glide, becoming stiff and painful.
This process isn’t limited to musculoskeletal injuries. It happens in our organs as well. Pulmonary fibrosis, liver cirrhosis, and the stiffening of cardiac tissue in heart failure are all manifestations of this same underlying pathology: chronic myofibroblast activation and runaway fibrosis.
A Clinical Case Study: The Systemic Impact of Localized Fibrosis
To illustrate how devastating this fibrotic state can be, let me share the story of a dear friend and patient. He is a brilliant man who, for various reasons, has been managing his health in a fragmented way. I had seen his labs years ago and noted some concerning markers—signs of anemia and kidney stress. But he didn’t follow up consistently.
He called me recently, five times in one week, his voice filled with despair. He had just seen his cardiologist, who informed him that his heart failure had significantly worsened. He was heartbroken and terrified. Listening to him, I immediately recognized the pattern. His body was in a state of hypercoagulation, a fibrogenic state strikingly similar to a systemic condition called Disseminated Intravascular Coagulation (DIC). In DIC, the body’s clotting mechanisms go into overdrive, creating micro-clots throughout the circulatory system, which can lead to organ failure.
In my friend’s case, the primary organ was the heart, but the underlying principle is the same. The fibrinogen levels in his blood were likely elevated—a marker I often see alongside high ferritin in inflammatory states. This sticky, clot-promoting environment is a direct consequence of the systemic inflammation that drives fibrosis. Our circulatory system is not separate from our tissues; it’s an information highway. Inflammatory cytokines and fibrotic signaling molecules produced in one area circulate throughout the body, triggering dysfunction elsewhere. His heart wasn’t failing in a vacuum; it was failing within a systemic environment that was primed for fibrosis and clotting.
I asked him a simple question: “What was your NT-proBNP level?” This is a crucial blood marker used to track the severity of heart failure. A healthy level is very low. In heart failure, it rises dramatically. With effective treatment, you can see this number drop from, say, 1,500 pg/mL down to 300 pg/mL, indicating that the strain on the heart is decreasing. He didn’t know his number. He hadn’t been tracking it, despite my recommendation a year prior.
He was looking for a cure, a magic bullet. But medicine rarely offers cures for chronic conditions like this. What we can do is manage the underlying physiology. We can work to turn off the inflammatory signals, break the fibrotic cycle, and support the body’s innate capacity for repair. His situation is a powerful, albeit tragic, example of how a localized problem—in this case, the heart—is deeply enmeshed in a systemic web of inflammation and fibrosis, demonstrating the critical need for a holistic, systems-based approach to healing.
Harnessing Sound for Healing: An In-Depth Look at Shockwave Therapy
Given this understanding of fascia, fibrosis, and the devastating cycle of chronic inflammation, the logical question is: how can we intervene? How can we communicate with the tissue to break this cycle and promote true regeneration? This is where modalities that act at the biophysical level become incredibly powerful. One of the most effective and well-researched of these is Extracorporeal Shockwave Therapy (ESWT).
My friend and colleague, Dr. P, does fantastic work with frequency-specific microcurrent and other vibrational therapies. Our conversations always circle back to the same conclusion: it’s not an “either/or” situation; it’s a “this and” approach. We are, at our core, electrical beings. Our tissues exhibit piezoelectricity, meaning they generate an electrical charge in response to mechanical stress. Our bodies are constantly interpreting and responding to physical forces. ESWT leverages this principle to restart a stalled healing process.
The Science of Shockwave: Beyond Ultrasound
First, let’s be clear about what a shockwave is and isn’t. People often confuse it with therapeutic ultrasound, but they are fundamentally different.
- Ultrasound waves are biphasic and continuous. As you can see in the upper diagram on the screen, they have a symmetrical sine-wave pattern with both positive (compressive) and negative (tensile) phases. These continuous oscillations primarily generate a thermal (heating) effect in the tissue.
- Shockwaves, in contrast, are monophasic. They are single-pulse acoustic waves characterized by a very rapid, high-pressure positive phase followed by a much smaller, longer negative phase. As the lower diagram illustrates, there is a dramatic, near-instantaneous rise to peak pressure. This is not a continuous oscillation. This unique physical property is what creates a strong mechanotransduction effect—the process by which cells convert a mechanical stimulus into a biochemical response.
ESWT is a non-invasive technology that uses a device to generate these high-intensity sound waves and deliver them to a specific area of the body. You might see it called Acoustic Wave Therapy or a similar name, but the principle is the same. It’s about delivering a precise mechanical force to stimulate a biological cascade. The technology has its roots in urology, where it has been used for decades as lithotripsy to break up kidney stones. It later found application in orthopedics for treating non-union fractures, in which bones have failed to heal on their own. Now, its application in musculoskeletal and regenerative medicine is exploding.
Radial vs. Focused Shockwave: Choosing the Right Tool for the Job
There are two main types of shockwave therapy, and they are not interchangeable. They have different methods of generation, physical characteristics, and clinical applications.
- Radial Shockwave Therapy (rESWT): This is the more common type you’ll see. The device has a handpiece that looks a bit like a pistol. Inside, a projectile is accelerated by compressed air and strikes a metal applicator. The energy created at the applicator head then radiates outwards into the tissue in a divergent, or radial, pattern.
- Characteristics: Energy is highest at the surface and dissipates as it moves deeper. It’s less precise and covers a broader area. The sensation is often described as a strong, percussive tapping.
- Best Use: Radial shockwave is excellent for treating larger, more superficial areas. I often use it as a preparatory treatment. It’s gentler and more diffuse, making it perfect for “loosening up” the surrounding fascial tissue before targeting a specific lesion. It helps improve circulation and downregulate hypersensitive nerve endings across a wide area.
- Focused Shockwave Therapy (fESWT): This technology is more advanced and was available in Europe long before it was widely adopted in the U.S. It uses an electrohydraulic, piezoelectric, or electromagnetic source to generate the wave, which is then focused by a lens or reflector to a specific point deep within the tissue, much like a magnifying glass focusing sunlight.
- Characteristics: The energy converges at a precisely adjustable focal point, enabling treatment of deep structures without significantly affecting the overlying tissue. It can penetrate much deeper than a radial shockwave.
- Best Use: Focused shockwave is the tool of choice for targeting specific deep pathologies, such as tendinopathies, non-union fractures, or trigger points within a muscle belly.
In my practice, I find the most effective approach is to use both together. I might start a treatment plan with radial shockwave to prepare the entire kinetic chain—calming the nervous system and improving tissue compliance. Then, in subsequent sessions, I can introduce focused shockwave therapy to target the primary lesion with greater precision and energy.
The Physiological Cascade: How Shockwave Reboots Healing
When a shockwave enters the tissue, it creates a cascade of biological effects that effectively reboot the healing process, shifting the tissue from a chronic, degenerative state to an acute, regenerative one.
- Releases Substance P and Induces Analgesia: Substance P is a neuropeptide that acts as a primary neurotransmitter for pain. Chronic pain conditions are often associated with high concentrations of Substance P. The intense pulses of shockwave therapy cause a depletion of Substance P in the local nerve endings and inhibit its resynthesis. This leads to a significant and often immediate reduction in pain—an analgesic effect.
- Enhances Circulation (Angiogenesis): Mechanical stress triggers the release of key angiogenic growth factors, such as Vascular Endothelial Growth Factor (VEGF). This stimulates angiogenesis and neovascularization—the formation of new blood vessels. You can see this in the diagrams showing tissue before and after treatment. The “before” tissue has sparse blood flow, while the “after” tissue shows a rich new capillary network. This is crucial. Improved blood flow brings oxygen and nutrients essential for healing and, just as importantly, flushes out metabolic waste products and inflammatory mediators that perpetuate the chronic state.
- Stimulates Collagen Production and Breaks Down Calcification: The therapy initiates a controlled, pro-healing inflammatory response. This functionally stimulates fibroblast proliferation. It encourages them to produce fresh, healthy Type I and Type III collagen, the building blocks of healthy tendons and ligaments. For conditions like “calcific tendinitis,” the mechanical force of shockwaves can physically break up calcium deposits, which the body can then clear through the lymphatic system and improved circulation. I’ve seen remarkable reductions in calcified scar tissue.
- Increases Cell Membrane Permeability and Restores Balance: At the cellular level, the shockwave’s shear force temporarily increases cell membrane permeability. This helps re-equilibrate the flow of ions such as sodium, potassium, and calcium, which is fundamental to restoring normal cell function, nerve signaling (action potentials), and mitochondrial energy production. You are essentially restoring the balance between tension and compression at the micro level, allowing the cells to breathe and function properly again.
- Mobilizes Stem Cells: Research has shown that shockwave therapy can stimulate the mobilization and migration of the body’s own mesenchymal stem cells to the site of injury. These are the master repair cells, capable of differentiating into various tissue types to facilitate regeneration. By using shockwave, we are essentially ringing the dinner bell and calling the body’s intrinsic repair crew to the job site.
The Principle of Hormesis: Therapeutic Stress for Adaptation
It’s vital to understand that the magic of shockwave—and many other regenerative therapies like Hyperbaric Oxygen Therapy (HBOT) or intermittent fasting—lies in the principle of hormesis. Hormesis is a biological phenomenon in which a beneficial effect results from exposure to a low dose of an agent that is otherwise toxic or lethal at higher doses.
When you apply shockwave to tissue, you create a controlled microtrauma. The therapy itself is the stressor. But the real healing happens after the treatment is over. The body perceives this controlled stress and mounts a powerful adaptive response. It up-regulates its own anti-inflammatory and regenerative systems. This response doesn’t just last an hour; it can last days or weeks.
It’s the same principle as HBOT. When you are in the chamber at high pressure (e.g., 2.0 ATA), your plasma becomes supersaturated with oxygen (hyperoxia). But when you come out, your body experiences a state of relative hypoxia. This swing is the hormetic trigger that stimulates the production of stem cells and other healing factors. Even low-pressure HBOT (e.g., 1.3 ATA) is now showing profound effects, especially in neurological healing, because it’s the change in oxygen tension that drives adaptation. The body loves adaptation. Shockwave therapy is a perfect example of using a targeted physical stressor to provoke a robust, positive biological adaptation.
Practical Application and Clinical Evidence: From Head to Toe
The applications for shockwave therapy are vast. Hundreds of peer-reviewed scientific studies have validated its efficacy for a wide range of musculoskeletal conditions, making it a highly cost-effective and evidence-based treatment.
- Plantar Fasciitis: This is one of the most well-studied indications, with success rates often exceeding 80-90%, even in chronic cases that have failed all other conservative treatments.
- Tendinopathies: Achilles tendinopathy, patellar tendinopathy (“jumper’s knee”), rotator cuff tendinopathy, and lateral epicondylitis (“tennis elbow”) all respond exceptionally well. ESWT is effective at breaking down the disorganized, degenerative tissue and stimulating the production of healthy new tendon fibers.
- Post-Stroke Spasticity: Shockwave therapy can be used to treat muscle spasticity and contractures after a stroke, improving range of motion and function.
- Bone Healing: As mentioned, it is highly effective for delayed union or nonunion fractures, stimulating bone-forming cells (osteoblasts) to resume activity. A case study on the screen shows the healing of a horse’s leg fracture, comparing a screw-only repair to a screw-plus-shockwave repair. The shockwave group shows significantly faster and more robust healing, getting the athlete back to play sooner.
- Myofascial Pain and Scar Tissue: It is excellent for breaking up dense scar tissue, whether from surgery or chronic injury, and for deactivating stubborn trigger points. I have even used it to break up cosmetic cellulite, which is fundamentally a problem of fibrotic bands pulling down on the skin.
I once treated my own hand after a particularly nasty injury. I made some Platelet-Rich Plasma (PRP), performed shockwave therapy on the area, and then injected the PRP. The initial response was intense—my hand was incredibly red and painful. I was worried I had overdone it. But I trusted the process and continued to work with it gently. The result was a complete recovery, with no residual scar tissue or dysfunction. I was shocked by how well it worked, especially in areas prone to adhesions, such as dentists’ hands or manual therapists’.
Important Contraindications and Precautions
While incredibly safe, shockwave therapy is not for everyone. There are some key contraindications:
- Active Malignancy: You never want to apply shockwave over a known tumor, as it could potentially encourage metastasis by increasing circulation.
- Pregnancy: It should not be used over the abdomen or the lower back of a pregnant woman.
- Coagulation Disorders or Anticoagulant Use: If a patient has a known clotting disorder or is taking blood thinners such as Warfarin, caution is essential. If my heart failure patient had a known clot in his heart (an atrial thrombus), I would absolutely not perform shockwave anywhere on his body.
- Over Open Growth Plates: It should not be used over the epiphyseal plates of growing children.
- Recent Corticosteroid Injection: Be cautious. Steroids weaken tissue. I recommend waiting at least six weeks after a steroid injection before applying shockwave to that area to avoid the risk of tissue rupture.
In conclusion, shockwave therapy represents a paradigm shift in how we treat chronic musculoskeletal and fibrotic conditions. By moving away from purely biochemical or suppressive interventions (like NSAIDs or steroids) and embracing a biophysical approach, we can communicate directly with the body’s tissues in a language they understand—the language of force and adaptation. We can break the cycle of chronic pain and degeneration and empower the body to do what it does best: heal itself.
A2M (Alpha-2-Macroglobulin): The Molecular “Mop” for Joint and Tissue Inflammation
In my practice, I am constantly seeking therapies that are not only effective but also work in harmony with the body’s natural physiology. One of the most remarkable tools in our regenerative arsenal is Alpha-2-Macroglobulin (A2M). This isn’t a synthetic drug or an external compound; it’s a large plasma glycoprotein that your own body produces, primarily in the liver. Think of it as the body’s innate cleanup crew, a molecular “mop” specifically designed to seek out and neutralize the agents of tissue destruction.
To truly appreciate the power of A2M, we must first understand the battlefield of a chronically inflamed joint, like an osteoarthritic knee. Within that joint space, a vicious cycle is at play. The initial injury or age-related wear and tear triggers an inflammatory response. This response, if not properly resolved, leads to the overproduction of a class of enzymes known as proteases. These include catabolic proteases like matrix metalloproteinases (MMPs) and ADAMTSs (A Disintegrin and Metalloproteinase with Thrombospondin Motifs).
In a healthy state, these enzymes are crucial for normal tissue remodeling—breaking down old, damaged cartilage so it can be replaced. However, in a state of chronic inflammation, they become hyperactive and unregulated. They begin to relentlessly chew away at the healthy cartilage, degrading the very collagen and proteoglycan structures that give the joint its cushion and smooth-gliding surface. This enzymatic destruction is a primary driver of pain, stiffness, and the progressive loss of function we see in osteoarthritis and other degenerative conditions.
This is where A2M makes its dramatic entrance. A2M is a massive protein with a unique structure, often described as a “venus flytrap.” Its primary function is to act as a pan-protease inhibitor, meaning it can trap and inactivate a broad spectrum of these destructive enzymes.
Here’s a step-by-step breakdown of its sophisticated mechanism:
- Detection and Baiting: The A2M molecule contains a “bait region.” When a destructive protease, such as an MMP, approaches, it is attracted to the bait region and cleaves it, thinking it’s just another protein to degrade.
- The “Trap” Mechanism: This cleavage triggers a massive conformational change in the A2M molecule. It essentially collapses around the protease, physically trapping it within a molecular cage. This is a covalent bond, meaning it’s incredibly strong and irreversible.
- Neutralization and Clearance: Once trapped, the protease is completely neutralized. It can no longer access and degrade cartilage or other tissue components. Scavenger receptors then recognize the entire A2M-protease complex on cells like macrophages, which engulf and clear it from the joint space, effectively removing the destructive agent from the environment.
By concentrating A2M directly in an inflamed joint or soft-tissue area, we are essentially giving the body a super-dose of its own natural defense mechanism. We are stopping the chemical source of the breakdown. This is why I find A2M so valuable, particularly as a preparatory step before other regenerative procedures. Imagine you are trying to plant a new garden. If the soil is full of weeds and toxins (the proteases), your new seeds (stem cells, for example) will struggle to grow. A2M therapy clears the soil. It creates a healthier, less inflammatory, and more pro-regenerative microenvironment.
If I am considering a stem cell or PRP procedure for a patient with significant joint degeneration, I will often recommend a preliminary A2M injection. By first reducing the levels of these hyperactive proteases, we ensure that the valuable growth factors and signaling molecules introduced by the subsequent procedure aren’t immediately degraded. It gives the regenerative cells a much better chance to survive, differentiate, and orchestrate the repair process.
The procedure itself involves a significant blood draw from the patient, as A2M needs to be concentrated from a large volume of plasma. My practice is equipped with the specialized centrifuge and filtration system required for this. While the kits and the process can be costly, the investment is often justified by the profound and long-lasting results. We are not just masking pain; we are intervening in the core biochemical pathway of tissue destruction. For patients suffering from neuropathic pain, joint degeneration, or chronic soft tissue inflammation, A2M offers a powerful, evidence-based strategy to halt damage and pave the way for true healing.
Photobiomodulation (PBM): Harnessing Light to Energize Cellular Healing
I firmly believe that we are, at our core, electrical and energetic beings. Our bodies are constantly humming with biochemical and bioelectrical activity. It stands to reason, then, that we can use external energy sources to influence and optimize these internal processes. This is the fundamental principle behind Photobiomodulation (PBM). This therapy uses non-ionizing light sources, including lasers, LEDs, and broadband light, in the visible and near-infrared spectrum to stimulate healing, relieve pain, and reduce inflammation.
For too long, medicine has been dominated by a purely chemical paradigm. PBM reintroduces the physics—specifically, the photoelectric effect—into our understanding of healing. This concept, for which Einstein won a Nobel Prize, describes how light, acting as a particle (a photon), can transfer its energy to an electron when it strikes a material. In the context of our bodies, this “material” is a specific molecule within our cells called a chromophore.
The primary chromophore targeted by PBM is Cytochrome C Oxidase, a crucial component of the mitochondrial electron transport chain. Think of the mitochondria as the power plants of our cells, responsible for producing Adenosine Triphosphate (ATP), the universal energy currency of the body.
Here’s how PBM sparks this cellular revitalization:
- Light Absorption: When photons of a specific wavelength (typically in the red and near-infrared range, roughly 600-1000nm) penetrate the tissue, they are absorbed by Cytochrome C Oxidase within the mitochondria.
- Nitric Oxide Dissociation: In stressed or inflamed cells, a molecule called Nitric Oxide (NO) can bind to Cytochrome C Oxidase, competitively inhibiting oxygen and effectively “clogging up” the ATP production line. The energy from the absorbed photon is just enough to break this bond, causing the NO to dissociate and release.
- Restoration of Oxygen Flow & ATP Production: With the NO “blockage” removed, oxygen can once again bind freely, restoring the electron transport chain to its full efficiency. This results in a significant increase in ATP production. More ATP means more energy for the cell to perform its essential functions, including repair and regeneration.
- Signaling Cascades: The release of NO isn’t just a side effect; it’s a therapeutic event in itself. The transient burst of NO acts as a powerful signaling molecule, leading to vasodilation (widening of blood vessels). This improves local circulation, bringing more oxygen and nutrients to the injured area and facilitating the removal of waste products. Furthermore, this process initiates downstream signaling cascades that activate transcription factors such as NF-κB (Nuclear Factor kappa B), leading to the production of a range of proteins involved in cell proliferation, migration, and tissue repair.
- Reduction of Oxidative Stress: PBM has also been shown to modulate Reactive Oxygen Species (ROS). While high levels of ROS cause oxidative stress and damage, the modest, transient increase induced by PBM appears to act as a beneficial signaling mechanism, upregulating the body’s own endogenous antioxidant defenses.
The clinical applications of these mechanisms are vast. In my practice, I utilize a variety of light therapy devices, from targeted wands to whole-body systems like a BioCharger, which combines multiple forms of energy. For a patient with peripheral neuropathy, for instance, applying PBM to the affected limbs can help reduce pain and inflammation by increasing circulation and providing the damaged nerves with the ATP they desperately need to repair their myelin sheaths. For a joint injury, it reduces swelling and pain. In the context of brain health, transcranial PBM is being explored to improve cognitive function by enhancing mitochondrial activity in neurons.
It’s crucial to understand that we are constantly bombarded by various energies in our modern environment, many of which are detrimental. Using targeted, therapeutic energies like PBM helps counteract this and actively support our body’s electrical nature. It is a modern, elegant, and deeply physiological approach that provides pain relief, reduces inflammation, improves circulation, and supports healing in a wide variety of neurological and musculoskeletal conditions. It’s a foundational therapy that helps power the very engine of cellular life.
The Foundational Trinity: Nourish, Measure, and Personalize
While advanced technologies like A2M and Photobiomodulation are powerful tools, they are most effective when applied to a body that has the fundamental building blocks it needs for repair. You cannot build a sturdy house with rotten wood and missing bricks. Similarly, you cannot expect the body to regenerate without the proper nutritional foundation. My approach to patient care is always anchored in this principle: nourish, nourish, nourish.
The ultimate goal is to nurture the extracellular matrix (ECM). The ECM is the intricate, non-cellular three-dimensional network that surrounds all our cells. I often describe it to patients as the “soil” in which our cellular “seeds” (including stem cells) are planted. This soil is composed of a complex mesh of proteins like collagen and elastin, as well as glycoproteins and proteoglycans. It provides structural support, but far more importantly, it’s the medium through which cells communicate, receive nutrients, and get signals to grow, migrate, or differentiate.
If this matrix is inflamed, dehydrated, or deficient in key nutrients, cellular function will be compromised. Stem cells will not receive the proper signals, waste products will accumulate, and the entire regenerative process will stall. Therefore, my priority is to ensure this “soil” is rich and fertile.
Measure, Don’t Guess: The Power of Advanced Diagnostics
This is where my philosophy diverges sharply from a one-size-fits-all approach. I never make things up. I need objective data to guide my clinical decisions because the risk of being wrong is too high when you are simply guessing. I rely on advanced functional testing to create a precise, personalized roadmap for each patient.
A cornerstone of this is the Organic Acid Test (OAT). This comprehensive urine test provides a snapshot of the body’s metabolic processes. It can reveal incredible detail about:
- Mitochondrial Function: Are you efficiently converting food into energy?
- Neurotransmitter Levels: Are there imbalances in dopamine or serotonin metabolites that could be contributing to mood or pain perception?
- Detoxification Pathways: Is your body effectively clearing toxins? The OAT measures markers for glutathione production, a master antioxidant crucial for detoxification.
- Nutrient Deficiencies: This is a critical one. The OAT can show functional deficiencies in key vitamins and minerals. It tells me whether the body has enough zinc, selenium, B vitamins, and amino acids, such as glycine, to perform its necessary enzymatic reactions.
When I see a low glutathione level, I know the body’s ability to handle oxidative stress is compromised. This isn’t just an abstract finding; it has direct clinical implications. It means the patient is more susceptible to inflammation and cellular damage. My intervention is then highly targeted: I will support glutathione production with its precursors, such as N-acetylcysteine (NAC), glycine, and selenium.
Personalized Supplementation: The Right Tools for the Right Job
Based on this detailed testing, I can recommend a highly specific nutrient protocol. This isn’t about throwing a generic multivitamin at the problem. It’s about surgical precision.
- Essential Fatty Acids: Everybody needs some form of omega fatty acids, but the type and ratio matter immensely. Based on their lab work and clinical presentation, a patient might need more EPA/DHA from fish oil for its potent anti-inflammatory effects. Another patient, perhaps with skin issues or hormonal imbalances, might benefit more from GLA (Gamma-Linolenic Acid), an omega-6 fatty acid. I measure, so I know.
- Phospholipids: Phosphatidylcholine is a vital component of every cell membrane in your body. It ensures membrane fluidity, which is essential for proper cell signaling and nutrient transport. For patients with neurological issues or liver detoxification challenges, supporting cell membrane health with phosphatidylcholine can be a game-changer.
- Minerals: Zinc is a cofactor in over 300 enzymatic reactions in the body. As we will see in the case study, a deficiency can have widespread effects, from impaired immune function to hair loss. Selenium is a critical cofactor for the enzyme glutathione peroxidase. Without it, your primary antioxidant system cannot function properly.
My approach is flexible and patient-centered. If a patient is overwhelmed, we start with just one thing. Let’s fix the most critical deficiency first. My team and I provide extensive follow-up, acting as partners and guides. We check in, monitor progress, and once the first change has been integrated, introduce the next. It’s a step-by-step process of rebuilding the body from the ground up.
Sometimes, we start with hormones if that is the patient’s most pressing concern. Other times, we start with the gut. The entry point can be anywhere, just like reading a book—you don’t always have to start on page one. The key is to be confident in your understanding of the underlying physiology and to use objective data as your compass. The ultimate goal remains the same: to create a nutrient-rich, well-supported internal environment where the body’s own regenerative potential can be fully unleashed.
The Pleiotropic Power of Nature’s Molecules: The Swiss Army Knife Approach to Healing
In the world of functional and regenerative medicine, we often look to nature for inspiration. We find that the most effective molecules and therapeutic interventions rarely have just one job. Instead, they exhibit pleiotropic effects, meaning that a single agent can produce multiple, often seemingly unrelated, biological responses. Think of these compounds not as a simple key fitting a single lock, but as a sophisticated Swiss Army knife, equipped with a variety of tools to address a complex problem from multiple angles.
Let’s consider a common flavonoid found in many plants. This single small molecule might simultaneously act as a powerful antioxidant, neutralizing damaging free radicals. At the same time, it could modulate inflammatory pathways such as NF-κB, effectively turning down the “volume” of systemic inflammation. It might also inhibit enzymes that contribute to scar tissue formation (fibrosis), promote the detoxification of harmful compounds, and subtly influence neurotransmitter balance in the brain.
This multi-pronged action is not an accident; it’s a hallmark of biological efficiency. The body’s systems are deeply interconnected, and a problem in one area—say, chronic inflammation—inevitably spills over to affect others, like metabolic health, immune function, and neurological integrity. A therapy that only targets one specific point in this complex web is often fighting an uphill battle.
This is where the “Swiss Army knife” approach becomes so valuable. When a patient presents with a constellation of issues, I ask myself a series of questions:
- What is the primary driver of their dysfunction? Is it unchecked inflammation?
- Am I trying to modulate an overactive immune response or elevate a suppressed one?
- Is there a need to reduce fibrosis and break down restrictive scar tissue, perhaps in a joint or an organ?
- Do I need to protect the cells from ongoing oxidative stress, a process known as cytoprotection?
- Is the goal to modulate the intricate signaling of the gut-brain axis?
The beauty of pleiotropic therapies is that we can often address several of these needs simultaneously. This principle extends beyond plant molecules. Consider some of the advanced tools we use in our practice:
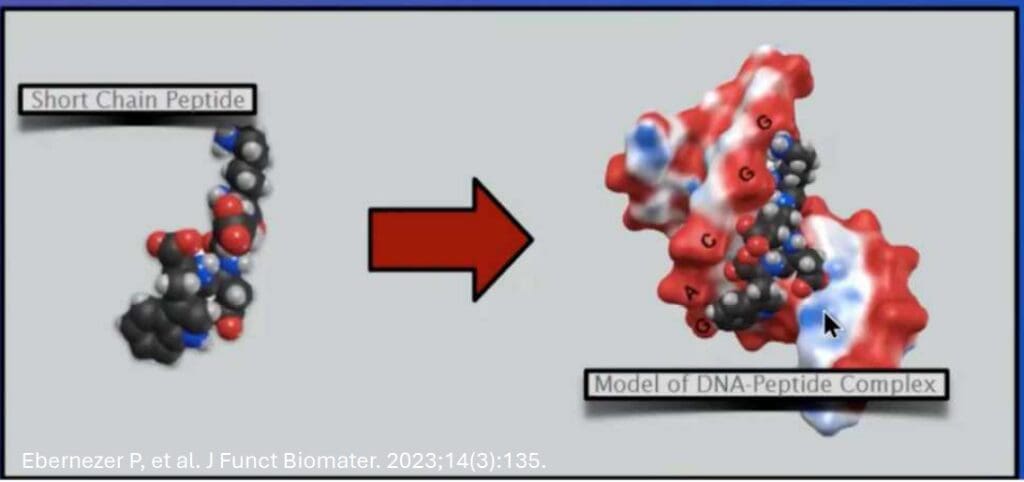
- Peptide Therapy: Peptides are short chains of amino acids that act as signaling molecules. A peptide like BPC-157 is a prime example of a pleiotropic agent. It is renowned for its ability to heal the gut lining. Still, it also promotes angiogenesis (the formation of new blood vessels), reduces inflammation, protects organs, and accelerates the healing of tendons and ligaments. It doesn’t just “fix” one thing; it orchestrates a broad, systemic healing response. It is the quintessential Swiss Army knife in our therapeutic toolkit.
- Light Therapy (Photobiomodulation): Exposing the body to specific wavelengths of red and near-infrared light can trigger a cascade of beneficial effects. It enhances mitochondrial function to produce more ATP (cellular energy), reduces inflammation, improves circulation, and stimulates collagen production. You might use it for skin rejuvenation, but it also helps reduce joint pain and improve muscle recovery.
- Hyperbaric and Intermittent Hypoxic-Hyperoxic Therapy (IHHT): The “hypoxic-hyperoxic paradox” involves strategically alternating between low-oxygen and high-oxygen environments. This process stimulates the production of Hypoxia-Inducible Factor 1-alpha (HIF-1α), a master regulator of cellular adaptation. The result? Growth of new blood vessels, mobilization of stem cells, enhanced mitochondrial efficiency, and a powerful anti-inflammatory effect. It’s a systemic “upgrade” driven by a simple, powerful stimulus.
The key takeaway is that these therapies are fundamentally modulatory. They don’t typically force a pathway into overdrive or shut it down completely, as many pharmaceuticals do. Instead, they work with the body’s innate intelligence to restore balance, or homeostasis. They provide the signals and resources the body needs to heal itself. This is why a peptide like BPC-157, or a therapy like IHHT, can be beneficial for such a wide range of conditions. They are not treating the disease; they are restoring the function of the underlying systems that have gone awry. By understanding and leveraging these pleiotropic, modulatory actions, we can create more elegant, effective, and holistic treatment plans that honor the complexity of the human body.
Navigating the System: Strategic Lab Testing and Patient Advocacy
One of the most significant challenges in modern medicine is not a lack of knowledge or technology, but the bureaucratic and economic maze of the healthcare system. As a clinician committed to evidence-based practice, I rely heavily on comprehensive laboratory testing to get an accurate picture of a patient’s physiology. However, obtaining these tests can be a minefield of insurance denials, exorbitant “patient responsibility” bills, and the looming threat of future insurance discrimination. A crucial part of my role has become that of a strategist and advocate, helping my patients navigate this system to get the care they need without facing financial ruin or future penalties.
The problem often begins with diagnostic codes. Every lab test ordered must be justified by an ICD-10 code, which represents a specific diagnosis or symptom. If an insurance company deems the test “not medically necessary” for the given code, they will deny the claim, leaving the patient with a potentially massive bill. Furthermore, certain diagnoses—even if used to justify a test—can be used by life or disability insurance companies to deny coverage or charge prohibitive premiums.
So, what is the solution? I’ve developed a meticulous strategy. When I determine a patient needs a panel of tests—perhaps to assess nutrient levels, hormonal balance, inflammation, and metabolic markers—I don’t use a single, highly specific (and potentially problematic) code. Instead, I carefully review the patient’s entire symptom profile and medical history to identify multiple, less alarming, and fully justifiable codes.
For example, I may use codes for:
- Myositis (muscle inflammation) to justify testing for inflammatory markers like C-Reactive Protein (CRP) or creatine kinase.
- Anemia (e.g., B12 deficiency anemia or iron-deficiency anemia) to justify tests for a complete blood count (CBC), ferritin, vitamin B12, and folate. This is a common, low-risk diagnosis.
- Vitamin D Deficiency is another common and non-threatening code.
- General symptoms like fatigue, malaise, or abnormal weight loss/gain.
I have compiled a master list of these “safe” and versatile codes, which my team uses to process lab requisitions. The goal is to find the most general yet accurate reason for the test that will not be held against the patient later. The primary reason I’m testing ferritin is that I suspect iron-deficiency anemia. Perhaps not. The primary reason might be to assess it as a critical inflammatory marker in the context of a complex chronic illness. But if the patient also has symptoms consistent with anemia, using that code is both ethically sound and strategically wise.
I also believe in radical transparency with my patients. I educate them about the “game” of health insurance. I explain that if we bill their insurance and the claim is denied, the lab will often charge them a retail price that is three or four times higher than the direct cash price. The lab cannot legally go back and offer the cash price after the insurance has been billed. Therefore, for some tests, it’s far cheaper to bypass insurance altogether. A Vitamin B12 test might cost $150 through insurance but only $12 if paid directly. Why a Vitamin D test can cost $50 is another mystery of healthcare pricing, but knowing the cost upfront empowers the patient.
I tell my patients, “I am going to recommend the tests I believe are clinically necessary for us to create an effective plan. I will also help you find the most affordable way to get them, whether it’s through a specific lab that offers better cash prices or by using your Health Savings Account (HSA). The choice is always yours. We can proceed with a plan based on your symptoms and clinical presentation—an educated guess—or we can test and know for sure. Here is the cost associated with each path.”
This approach was born from hard-learned lessons. Early in my practice, I worked with a lab company under the assumption that they would handle the billing responsibly. I sent the patient’s insurance information and the appropriate codes. Later, I received a massive bill for thousands of dollars in “outstanding” lab fees. The company claimed that because the patients did not respond to their calls or emails to settle the denied claims, I, as the ordering physician, was responsible. This experience solidified my resolve to protect both my patients and my practice from the predatory aspects of the medical-industrial complex.
My advice to patients today is often counterintuitive: consider getting a lower-premium insurance plan and saving the difference to pay for diagnostics and treatments directly. Use your HSA wisely. Be a savvy consumer of healthcare. My job is not just to diagnose and treat, but also to be your guide and advocate in this challenging environment, helping you make wise choices about your health and resources.
The Realities of Advanced Therapies: Cost, Safety, and Clinical Application
Integrating cutting-edge regenerative therapies into a clinical practice is an exciting prospect, but it comes with a host of practical challenges that are rarely discussed in academic papers. From the prohibitive cost of equipment to the steep learning curve and critical importance of patient safety, these are the on-the-ground realities that clinicians must master.
A perfect example is the financial barrier to entry for many advanced modalities. I’ve often looked at a new piece of equipment—say, a machine for a specific type of extracorporeal blood treatment—and been astounded by the price tag. The manufacturer wants me to buy their machine, but then they make the disposable, single-use kits required for each treatment absurdly expensive. I once had a machine that sat in my office for six years, a constant reminder of this frustrating dynamic. I even challenged my engineering student interns, “Go figure out how to make these disposables cheaper. It’s absurd that a single treatment kit costs $500. It’s simply not sustainable for the patient.” This financial burden creates a significant barrier to access, limiting these powerful therapies to only the very wealthy.
Beyond cost, there is the critical issue of technique and patient safety. A therapy is only as good as the person administering it. I’ve seen firsthand how a powerful treatment can go wrong in inexperienced hands. Let’s talk about Extracorporeal Blood Oxygenation and Ozonation (EBOO), a procedure where blood is drawn from one arm, passed through a dialysis filter where it is oxygenated and ozonated, and then returned to the other arm. It’s a powerful systemic detoxification and anti-inflammatory treatment. However, it requires significant skill to manage the patient, the equipment, and the IV access.
I’ve had patients tell me they would rather have a knee injection any day of the week than go through another EBOO treatment. Why? Because a poorly executed procedure is uncomfortable and stressful. You need to cannulate two veins, the patient is tethered to a machine, and the blood flow must be carefully managed. I even witnessed a cardiothoracic surgeon, a brilliant man in his own field, attempt to perform this procedure on a patient in my office. He hooked the patient up, and then we all left the room. A few moments later, I heard the patient coughing and gasping for air. I rushed in to find him in distress. The surgeon had inadvertently turned off the machine. I had to intervene immediately. It was a stark reminder that even the most accomplished medical professionals need specific training and hands-on experience for these specialized procedures. This is not a “set it and forget it” therapy.
This is why I am so meticulous about vetting both the technology and the practitioners I collaborate with. I have sought out and trained with clinicians who are true masters of their craft. For example, I spent days training with a remarkable physician who has developed his own refined techniques for blood filtration and has healed countless patients. I’ve had these procedures performed on myself. I’ve seen the difference that expertise makes.
The bottom line is this: there is no single silver bullet in medicine. If there were, none of us would need to be here, constantly learning and refining our approach. The effectiveness of any advanced therapy—whether it’s EBOO, MUSE cell administration, or peptide injections—depends on a combination of factors:
- The right patient: Is this therapy appropriate for this individual’s specific condition and physiology?
- The right protocol: What is the correct dosage, frequency, and duration of treatment?
- The right technique: Is the practitioner highly skilled and experienced in administering the therapy safely and effectively?
- The right combination: Is the therapy being used in synergy with other supportive treatments to address the root cause of the problem?
For example, some of the most advanced protocols I’ve seen involve a sequence of therapies. A clinician might perform an EBOO treatment to “clean the canvas”—to reduce the patient’s inflammatory load and improve the microcirculatory environment. Then, immediately afterward, they might administer a high dose of exosomes or Dezawa MUSE cells, knowing that these regenerative agents will now enter a much more receptive and less hostile biological environment. This thoughtful, synergistic sequencing is where the real art and science of regenerative medicine lie. It’s about more than just owning the latest machine; it’s about mastering the “how,” the “when,” and the “why” for each unique patient.
Body Signals Decoded- Video
The Vanguard of Regenerative Medicine: Understanding Dezawa MUSE Cells
In the rapidly evolving field of regenerative medicine, the term “stem cells” is often used as a broad, catch-all phrase. However, this oversimplification does a great disservice to the nuanced and highly specific science that underpins this discipline. Not all stem cells are created equal, and one of the most exciting and rigorously studied types is the MUSE cell, which stands for Multilineage-differentiating Stress Enduring cell. To truly appreciate their therapeutic potential, it’s essential to understand what they are and why the source and processing method are critically important.
MUSE cells were discovered and characterized by a team of researchers led by Dr. Mari Dezawa in Japan. Her extensive work, documented in over 200 published scientific papers, has established these cells as a unique and powerful tool for regeneration. What makes them so special?
- Stress Enduring: As their name implies, MUSE cells have a remarkable ability to survive severe cellular stress. When tissue is damaged—whether by trauma, lack of oxygen (ischemia), or inflammation—most cells die. MUSE cells, however, can endure this hostile environment. They are naturally present in our bodies in small numbers, acting as a “first responder” repair crew that activates in response to injury.
- Homing Capability: When administered intravenously, MUSE cells have an innate ability to “home” to sites of injury and inflammation. They are guided by the chemical distress signals (chemokines) released by damaged tissues. This means they travel through the bloodstream and accumulate precisely where they are needed most, rather than distributing randomly throughout the body.
- Multilineage Differentiation: Once they arrive at the site of damage, MUSE cells can differentiate into a wide variety of cell types to replace those lost. They are pluripotent, meaning they can become cells of all three primary germ layers: endoderm (e.g., liver, pancreas), mesoderm (e.g., bone, muscle, cartilage), and ectoderm (e.g., neurons, skin). This versatility makes them applicable to a vast range of degenerative conditions.
- Non-Tumorigenic: Unlike embryonic stem cells, MUSE cells are non-tumorigenic. They integrate into damaged tissue and stop dividing once the repair is complete, posing a very low risk of forming tumors.
- Immune-Privileged: MUSE cells have low immunogenicity, meaning they are less likely to be rejected by the recipient’s immune system. This makes allogeneic (donor-sourced) MUSE cell therapy a viable option without the need for harsh immunosuppressive drugs.
Given these remarkable properties, it’s clear why the name “Dezawa” is so important. When a clinician refers to “Dezawa MUSE cells,” they mean the cells have been isolated, cultured, and processed according to the specific, patented protocols developed by Dr. Dezawa and her team. This is a critical distinction in quality control. Many labs may claim to offer “stem cells.” Still, if they are not specifically Dezawa MUSE cells, they lack the same body of scientific evidence supporting their identity, safety, and efficacy. So, when I consider using a cellular therapy product, my first question is always: “Are these authentic Dezawa MUSE cells?”
The applications are profound. In my practice and in the broader research community, we’re seeing their use in complex cases ranging from neurodegenerative diseases to autoimmune conditions and post-COVID recovery. When you’re dealing with a patient who has a high inflammatory load and significant tissue damage, administering a high dose of these targeted, stress-enduring cells can provide the raw materials for a level of repair that the body can no longer achieve on its own.
Furthermore, we are seeing these cells being used in combination with other powerful therapies. As mentioned earlier, a protocol might first “clear the ground” with a treatment such as EBOO to reduce systemic inflammation, and then introduce the MUSE cells into a more favorable environment. Some protocols also incorporate other types of regenerative cells, such as trophoblastic stem cells, which are sourced from the placenta and are also known for their powerful regenerative and immunomodulatory properties.
The key is to understand that we are moving into an era of highly specific, targeted regenerative medicine. It’s not just about injecting “stem cells”; it’s about choosing the right type of cell, from the right source, processed in the right way, and administered in the right context to address the patient’s specific pathology. The work of pioneers like Dr. Dezawa has given us a powerful, evidence-based tool, and it is our responsibility as clinicians to use it with the precision and respect it deserves.
The Energetic Blueprint: Cellular Memory, Tissue Intelligence, and Intergenerational Transfer
One of the most profound and mind-bending concepts emerging from the frontiers of biology is the idea that our tissues possess a form of memory. This is not memory in the cognitive sense, such as recalling a childhood event, but a deeper, energetic, and informational imprint stored within the very fabric of our cells and the extracellular matrix. This concept challenges the purely mechanistic view of the body and opens the door to understanding how experiences, exposures, and even ancestral information can be physically encoded and transmitted.
We often talk about the body in electrical terms. Our nervous system runs on electrical impulses, our heart has an electrical conduction system, and every cell maintains an electrical potential across its membrane. But the concept of tissue memory suggests a more subtle form of energy and information storage. How else can we explain phenomena that defy simple biochemical explanations?
Consider the field of psychoneuroimmunology, which studies the interactions among our psychological processes, nervous system, and immune system. We know that chronic stress and trauma can lead to tangible, long-term changes in immune function and inflammation. The “memory” of that trauma isn’t just in the brain; it appears to be held in the body’s tissues, creating a state of chronic hypervigilance and inflammation. This is why body-based therapies like Somatic Experiencing or certain types of bodywork can be so effective in releasing trauma—they are working directly with the information stored in the tissues.
A more recent and controversial example comes from research surrounding the COVID-19 vaccines. Studies have emerged that found evidence of vaccine-induced spike protein in the sperm of vaccinated fathers. This information was then subsequently detected in their newborns. How is this possible? The conventional view struggles to explain how a protein fragment could be so durably stored and then transferred via germ cells.
However, if we adopt an energetic and informative framework, it makes more sense. The body is not just a collection of chemical reactions; it is a dynamic, resonant field of information. Tissues, and the water-rich extracellular matrix that surrounds them, may function like a liquid crystal, capable of storing and transmitting information via vibrational patterns and electromagnetic fields. The spike protein, or more accurately, the data of the spike protein, could be encoded into this biological matrix. This energetic signature, this “memory,” can then be passed on through the energetic continuum of the germ line.
This is a paradigm-shifting idea. It suggests that our cells and tissues are “listening” to our experiences and environment on a level we are only just beginning to comprehend. It gives a plausible mechanism for phenomena that have long been observed but dismissed as anecdotal, such as:
- The “memory” of an injury that aches when the weather changes.
- The transfer of tastes or preferences in organ transplant recipients.
- The persistence of “phantom limb” pain, where the energetic blueprint of the limb remains even after the physical structure is gone.
This concept has profound implications for how we approach healing. It means that true, deep healing may require more than just correcting biochemical imbalances. It may require us to address the informational and energetic imprints held within the body. Therapies that work on this level include:
- Peptide Therapy: Peptides are signaling molecules; they are pure information. They can introduce new, corrective messages into the system to override faulty or “stuck” informational loops.
- Frequency and Light Therapies: These modalities use specific frequencies of sound, light, or electromagnetic fields to interact with and restore coherence to the body’s own energetic field.
- Detoxification Protocols: By clearing heavy metals, toxins, and other disruptive elements from the extracellular matrix, we can improve the clarity and fidelity of the body’s internal communication system.
The idea that information and memory can be stored in our very tissues and passed down through generations is not science fiction. It is the leading edge of a new biology, one that recognizes the body as an intelligent, interconnected system of energy and information. As we continue to explore this “bio-energetic” framework, we will unlock even more powerful ways to understand and heal the human body, moving beyond the physical to address the energetic blueprint that underlies our health.
A Hierarchical Approach to Post-Traumatic Osteoarthritis in the Young
When a young person presents with osteoarthritis (OA) that is significantly advanced for their age, it’s almost always a case of post-traumatic OA. This can result from a single major injury, such as a ligament tear or fracture, or from the cumulative effects of repetitive microtrauma and surgeries. The conventional approach often jumps directly to managing symptoms with anti-inflammatory drugs and, eventually, joint replacement. My approach, however, is hierarchical and foundational. I believe we must first address the underlying systemic issues preventing the joint from healing before we bring in high-tech regenerative tools. There is a definite role for peptides like Thymosin Beta-4 (TB-500) and BPC-157, but they are not the first step.
Here is how I would structure the treatment plan for a young individual with post-traumatic OA, building from the ground up:
Step 1: Re-mineralize and Balance the Terrain
The first and most overlooked aspect of joint health is the body’s mineral composition. We are fundamentally mineral-based beings. The cartilage, bone, and synovial fluid that make up a joint require a rich and diverse array of minerals to maintain their structure and function. We have become hyper-focused on a few key players, like magnesium and calcium. Still, we often forget the vast spectrum of trace minerals that are essential for enzymatic processes, collagen synthesis, and the control of inflammation.
Our modern food supply is notoriously depleted of these vital minerals due to soil degradation. Therefore, my first intervention is to ensure the patient has an abundant supply of a full spectrum of minerals. This means looking beyond standard supplements. We must consider the periodic table of elements. Yes, some aspects of that table are toxic in large amounts, but many are required in minute, trace amounts for optimal physiological function. We often find that patients with degenerative conditions are deficient in elements such as silica, boron, manganese, copper, and many others that are no longer present in their diet.
Alongside re-mineralization, I assess and address the body’s pH balance. A state of chronic, low-grade metabolic acidosis creates an internal environment that is hostile to healing. Acidic stress contributes to the breakdown of cartilage and bone, as the body leaches alkaline minerals from these tissues to buffer the acid load. Correcting this with dietary changes, proper hydration, and targeted alkaline-forming supplements is a non-negotiable first step.
Step 2: Protect the Core and Provide the Building Blocks
The next step is to protect the body’s primary regenerative engine: the bone marrow. The bone marrow is the source of our hematopoietic and mesenchymal stem cells, the very cells that are responsible for tissue repair. If the bone marrow is suppressed by chronic inflammation, toxicity, or nutrient deficiencies, the body’s ability to heal is profoundly compromised. Therapies that support bone marrow health, such as certain peptides and nutrient protocols, are crucial.
Simultaneously, we must provide the raw materials for repair. A joint is primarily made of collagen, which is made of protein. I will ensure the patient’s diet is rich in high-quality protein and supplemented with specific amino acids that are the precursors to collagen, such as glycine, proline, and lysine. Using a targeted secretagogue, which is a substance that stimulates the pituitary gland to release its own growth hormone, can also be beneficial here. A gentle, pulsatile release of endogenous growth hormone is a powerful signal for tissue repair without the risks of using exogenous hormones. A peptide like CJC-1295/Ipamorelin could be considered at this stage.
Step 3: Introduce Targeted Regenerative Peptides
Once the foundation is laid—the mineral stores are replenished, the pH is balanced, and the basic building blocks are available—we can introduce the more specialized tools. This is where peptides like BPC-157 and Thymosin Beta-4 (TB-500) shine.
- BPC-157: As our “Swiss Army knife,” BPC-157 will work systemically and locally to reduce inflammation in the joint, promote the formation of new blood vessels (angiogenesis) to bring nutrients to the damaged cartilage, and accelerate the healing of ligaments and tendons that provide stability to the joint. It is a master orchestrator of the healing cascade.
- Thymosin Beta-4 (TB-500): TB-500 primarily promotes cell migration, differentiation, and tissue regeneration. It is particularly effective at stimulating the progenitor cells that give rise to cartilage (chondrocytes) and at reducing inflammation within the joint capsule. It acts as the “foreman” on the construction site, directing the raw materials and cellular workers to the right place to rebuild the damaged structure.
In some cases, I might also consider a more advanced injectable therapy, such as Extracellular Matrix (ECM) products, which provide a biological scaffold for new tissue to grow on, or a bioregulatory peptide designed to support cartilage health.
The key to this hierarchical approach is patience and diligence. We are not looking for a quick fix. We are systematically rebuilding the body’s internal environment and its innate capacity for healing. By addressing foundational issues first, we ensure that when we introduce powerful regenerative agents like BPC-157 and TB-500, they can work their magic in a receptive, supportive biological environment, leading to more profound, lasting results. This is the essence of true regenerative medicine.
The Uniqueness of the Individual: A Tale of Two Twins
One of the most profound lessons in my clinical practice—and indeed, in my personal life—is the undeniable uniqueness of each individual. The principle of biochemical individuality is not just a theoretical concept; it is a fundamental truth that I see play out every single day. Even identical twins, who share 100% of their DNA, can have dramatically different health journeys and responses to life.
I have a unique perspective as the mother of identical twin daughters. For the first two decades of their lives, their synchronicity was astonishing. They looked the same, of course, but it went far deeper than that. They broke the same fingers on the same day. They lost their baby teeth within hours of each other. Their growth charts were so perfectly aligned that they would both grow half an inch in the same week. They slept in the same bed, shared everything, and even, as toddlers, would suck on each other’s thumbs. They were, for all intents and purposes, a single entity in two bodies.
All the “experts” who studied them were fascinated by their similarities. They had the same diet, the same environment, the same upbringing. And then, life happened.
They went off to college and, for the first time, had truly different experiences. One of my daughters entered into a situation that was incredibly damaging—emotionally, psychologically, and even physically. She experienced a level of trauma that her sister did not. And in their mid-20s, everything changed. The perfect synchronicity was shattered. The invisible trauma had imprinted itself on her biology. Their health trajectories, their emotional responses, and their physiological needs diverged completely. They were no longer the same.
This experience with my own daughters, who are now 28, informs my approach to every patient who walks into my office. If identical twins, with similar genes and nearly identical upbringings, can be so profoundly different due to their unique experiences, how can we possibly treat any two unrelated patients with the same protocol?
When a patient comes to me, I see more than a diagnosis. I see a unique biography written into their physiology. The fraternal twins I treat are unique individuals from birth. The siblings I treat require different approaches. My son, who is just 15 months older than my twins, has distinct needs.
This principle becomes particularly poignant when a family is in crisis. Recently, the daughter who endured the trauma required an intensive intervention. It was a serious event that demanded a massive mobilization of resources—emotional, financial, and temporal. I had to sit down with my other children and have a frank conversation. “Right now,” I told them, “all of my resources have to go to your sister. We are in survival mode. I am here for you, I love you, but there is only so much of me to go around. I need you to pull your own stuff together and let me know if you are in a true crisis. The squeaky wheel is getting the oil right now.” And I reminded them, “If it were you, and when it has been you in the past, you received the same focused attention.”
This is a microcosm of clinical practice. We must triage and prioritize. When a patient presents with a complex case, we must identify the “squeaky wheel”—the system in the most acute state of dysfunction—and direct our initial efforts there. Is it the gut? The adrenal glands? The immune system? We must address the most pressing fire first, all while keeping the whole person in view.
This is why I reject one-size-fits-all protocols. BPC-157 might be a go-to peptide for gut healing, but it’s not the right tool for everyone in every situation. A ketogenic diet might be miraculous for one person’s brain health and disastrous for another’s hormonal balance. The art of medicine lies in the ability to listen to the patient’s story, their symptoms, and the subtle signals of their body—and to tailor a truly individualized plan that honors their unique journey, biochemistry, and needs at that specific moment in time. My daughters taught me that in a way no textbook ever could.
Case Study Series: Applying Integrative Principles in Complex Conditions
To truly illustrate how these principles converge in a clinical setting, I want to share a series of cases that are powerful testaments to the body’s interconnectedness and its profound capacity for healing when the right underlying issues are addressed.
Case Study 1: Healing Alopecia, Inflammation, and Distress in a Young Boy
This case is one of my earliest and most memorable patients, and it solidifies my belief in an integrative, systems-based approach. The patient was an 11-year-old boy. His parents brought him to me in a state of deep distress. The presenting issues were alarming: alopecia areata (patchy, autoimmune hair loss) that was progressing rapidly, persistent nocturnal enuresis (bedwetting), and significant emotional upset. For a boy on the cusp of adolescence, losing his hair and wetting the bed was socially and emotionally devastating.

His parents explained that they had been on a frustrating journey, seeking answers from conventional medicine. They had been to a major children’s hospital where he was given a diagnosis of Lyme disease and treated with a course of minocycline. However, his condition did not improve; in fact, it worsened. The family came to me in January, feeling lost and desperate.
The Diagnostic Deep Dive: Uncovering the Roots
My first step, as always, was to look deeper. We ran a comprehensive panel of labs to investigate the underlying functional imbalances. The conventional tests for celiac disease, CRP (C-Reactive Protein, a general marker of inflammation), CBC (Complete Blood Count), and CMP (Comprehensive Metabolic Panel) were all largely unremarkable. This is a common scenario; standard labs often miss the functional disturbances that drive chronic illness.
However, two critical findings stood out from our more specialized testing:
- Low Zinc: His zinc level was significantly low. As I mentioned earlier, zinc is a vital mineral cofactor for hundreds of biological processes. It is essential for a healthy immune system, proper growth and development, and the integrity of skin and hair. A deficiency in a growing boy is a major red flag.
- Low BPC-157: We measured his low endogenous BPC-157 levels. BPC-157 (Body Protective Compound-157) is a peptide—a short chain of amino acids—naturally found in human gastric juice. It is a master repair signaling molecule, known for its potent systemic healing effects. It plays a crucial role in gut health, wound healing, angiogenesis (the formation of new blood vessels), and modulating inflammation. Knowing his genetic history and his parents’, I suspected a predisposition that might affect his ability to produce or utilize this critical peptide. Low levels would certainly contribute to systemic inflammation and poor tissue repair.
Here we had two concrete, actionable pieces of data. His body was lacking a fundamental building block (zinc) and a key repair signal (BPC-157). The alopecia and bedwetting were not two separate problems; they were likely downstream manifestations of a core systemic inflammatory process and a compromised ability to heal.
A Multi-Pronged Treatment Protocol
Armed with this information, we designed a multi-faceted treatment plan. This was not about treating the alopecia or the bedwetting in isolation; it was about treating the boy and restoring his body’s systemic balance.
- Nutritional Support: The first and simplest step was to correct the zinc deficiency. We significantly increased his zinc supplementation, from the low dose he was already taking to a more therapeutic level.
- Peptide Therapy – BPC-157: We began subcutaneous (subQ) injections of BPC-157. The goal was to replenish his low levels of this master repair peptide. By providing an external source, we aimed to quell the systemic inflammation, promote healing in his gut (which is often the epicenter of autoimmunity), and send a powerful “repair” signal throughout his entire system.
- Local Regenerative Therapy – PRP: To directly target the areas of hair loss, we performed Platelet-Rich Plasma (PRP) injections into the dermis of his scalp. This procedure involves drawing the patient’s own blood, concentrating the platelets, and injecting this platelet-rich solution into the target tissue. Platelets are a reservoir of powerful growth factors that stimulate tissue regeneration and activate local stem cells. In this case, the goal was to awaken the dormant hair follicles.
The results were astonishing. Five weeks after his first treatment, he returned to the office, and the change was dramatic. New hair was visibly starting to grow in the bald patches. His parents were overjoyed. More importantly, the bedwetting had stopped completely. This confirmed that we were on the right track—we were treating a systemic issue, and the improvements were body-wide.
Phase Two: Enhancing the Healing Cascade with TB4
While the initial progress was remarkable, there were still areas of alopecia. To build on our success, we initiated a second phase of treatment. We continued PRP on the scalp to further stimulate follicles and added methionine, an essential amino acid crucial for hair health. Crucially, we added another therapeutic peptide: Thymosin Beta-4 (TB4). TB4 is another systemically active repair peptide known for promoting cell migration, stimulating the formation of new blood vessels, and strongly downregulating inflammation. It works in beautiful synergy with BPC-157. While BPC-157 is a potent stabilizer and protector, TB4 is a primary promoter of actin mobilization—the very process by which cells move to sites of injury to begin repair. I often think of TB4 as a key signal for “recruiting the troops” to the battlefield. He started taking TB4 subcutaneously every day.
Over ten years ago, when I treated him, our understanding of peptide dosing was still evolving. But I knew the physiology. I knew that by providing both BPC-157 and TB4, we were giving his body an unparalleled combination of signals to protect, repair, and regenerate. The final results were a complete success. His mom sent me pictures showing a full, healthy head of hair. This case was a profound learning experience that solidified my belief in an integrative, systems-based approach.
Case Study 2: The Mouth-Body Connection and Oral Regeneration
The human body is not a collection of disconnected parts; it is a deeply integrated system. Nowhere is this more evident than in the relationship between oral health and systemic health.
One of the most critical and underappreciated issues in dentistry is the formation of cavitations. A cavitation is an area of dead or decaying bone, often occurring in the jaw at the site of a previous tooth extraction. These areas become chronic, low-grade septic pockets that continuously leak inflammatory cytokines and bacterial toxins into the bloodstream. I will state this unequivocally: if we could effectively identify and fix the cavitations in people’s mouths, we could heal a significant portion of heart disease. The mouth is a direct source of organisms and inflammation that seeds the rest of the body.
Let me share a case that highlights a regenerative approach to oral health. This patient first came to see me around 2019, dealing with a failing dental implant due to fragile bone. Her bone density was insufficient to support the implant. I advised her to consult her local oral surgeon, and in 2020, we began a collaborative effort. Her surgeon was Dr. Arun Garg, a talented practitioner I’ve had the pleasure of working with.
Our treatment plan was based on stimulating her body’s own healing processes within the jaw.
- Platelet-Rich Plasma (PRP): We used her own blood to prepare a platelet-rich plasma concentrate containing growth factors. Platelets release a host of growth factors that orchestrate the healing cascade: they attract stem cells, stimulate cell proliferation, and promote the formation of new blood vessels. We injected PRP throughout the soft tissue and into the bone surrounding the failing implant.
- Phosphatidylcholine (PPC): This is another key element of her protocol. PPC is a fundamental component of all our cell membranes. When administered, often intravenously, it helps to repair damaged cell membranes throughout the body, supporting cellular health and robust tissue regeneration. She takes it orally or via another route based on her preference and schedule.
This tailored treatment protocol empowers her to take control of her health. Today, her oral health is the best it has ever been. The bone has regenerated, the implant is stable, and she is thriving. This is a perfect example of what can be achieved when we combine skilled surgical intervention with biological therapies that support the body’s innate wisdom.
Case Study 3: Accelerating Musculoskeletal Recovery in Athletes
The principles of regenerative medicine have transformative applications in sports medicine. Let’s explore a few cases.
The Young Athlete with a Hamstring Tear: This case involves a 26-year-old male I’ll call George. He had just recovered from a significant health crisis when he sustained an acute hamstring tear while sprinting for a soccer ball. He came into the office right away. Our approach was twofold:
- Shockwave Therapy: We administered ESWT twice a week. The shockwaves create micro-trauma, jumpstarting the body’s healing response by increasing blood flow, stimulating growth factor release, and reducing pain.
- Peptide Therapy: To complement the physical modality, we used BPC-157 and TB4. BPC-157 is renowned for its healing effects on muscle and tendon, while TB4 is crucial for cell migration and stem cell activation. Together, they create a powerful synergistic effect.
The results were swift. He healed completely, getting back on his feet far quicker than with conventional rest and ice.
The Student with Chronic Joint Injuries: This 26-year-old student came to me in 2021 from California with chronic injuries in his left shoulder and right knee that had persisted for two years despite physical therapy. This is a classic picture of a chronic, non-healing state with fibrosis and low-grade inflammation. Our treatment plan included:
- Peptide Injections: We injected a combination of BPC-157 and TB4 directly into both the shoulder and knee joints to reduce inflammation, break down fibrosis, and stimulate regeneration.
- Shockwave Therapy: We used shockwave on both joints to stimulate blood flow and trigger the healing cascade.
- Altitude Therapy: Intermittent Hypoxic-Hyperoxic Training (IHHT), in which a patient breathes air with alternating low and high oxygen concentrations. This process creates a mild stress that forces mitochondria to become more efficient, enhancing systemic healing capacity.
The outcome was a complete success. He regained full strength and, since 2021, has been attending Harvard Business School, even running the Boston Marathon. These cases underscore a key principle: tissue wants to heal; you have to give it what it needs.
Decoding Long COVID: A Deep Dive into Systemic Inflammation and Autoimmunity
We now face a global health challenge of unprecedented scale: Post-Acute Sequelae of SARS-CoV-2 infection (PASC), more commonly known as Long COVID. This condition presents with a bewildering array of over 200 possible symptoms, affecting nearly every organ system. I want to walk you through a comprehensive case of a young woman with Long COVID to illustrate the profound systemic dysregulation that can occur and how we can begin to address it.
The Patient Presentation
This 22-year-old patient came to see me from Wisconsin. She is from a family of physicians; her mother is a pediatrician. For a year and a half, she had been incredibly sick. Her primary issue was profound exertional fatigue. This wasn’t just feeling tired; this was a complete crash after even minimal physical or mental effort, a hallmark symptom known as post-exertional malaise (PEM). Her case was a classic Long Hauler’s story.
Her medical history was complex:
- Initial Infection: March 2020, early in the pandemic.
- Reinfection: Two years later.
- Co-morbidities: A history of Irritable Bowel Syndrome (IBS), chronic elbow tendonitis, and recurrent skin issues.
- Systemic Symptoms: She was heavier than her normal weight, had developed disordered eating patterns, and was struggling with significant anxiety and depression.
My task was to get her out of the “tunnel” of chronic illness.
Lab Analysis: Uncovering the Roots of Dysfunction
To understand what we were dealing with, we needed a deep dive into her biochemistry. Her labs told a story of profound immune dysregulation and metabolic chaos.
Complete Blood Count (CBC): A Window into the Immune System
The first and most glaring finding was on her basic CBC with differential.
- White Blood Cell (WBC) Count: 1.7 K/uL (Normal range is typically 4.0-11.0). This is a state of severe leukopenia (low white blood cells).
- Neutrophils: Her neutrophil count was dangerously low (neutropenia). Neutrophils are our primary defense against bacterial infections.
- Platelets: Her platelet count was low at 175 K/uL (normal range is roughly 150-450). This is a concern in Long COVID and is often related to endothelial damage.
Clinical Insight: Forget the subtle details. The bottom line was leukopenia. Her immune system was suppressed and exhausted. This is the central problem that needs to be resolved.
Inflammatory and Metabolic Markers: The Fire Within
- C-Reactive Protein (CRP): 3.7 mg/L. Elevated, indicating a persistent inflammatory state.
- Fibrinogen: Slightly elevated. A sign of inflammation and potential micro-clotting.
- Interleukin-6 (IL-6): 3.0 pg/mL. Persistently elevated, driving a low-grade “cytokine storm.”
- Insulin and HOMA-IR: Elevated, indicating metabolic dysfunction and insulin resistance.
- Coenzyme Q10 (CoQ10): A significant deficiency. CoQ10 is critical to the electron transport chain in our mitochondria, which generates ATP. A deficiency means her cellular energy production was severely impaired—a direct biochemical explanation for her profound fatigue.
- Cortisol: Her morning cortisol level was 29 ug/dL. This is extremely high, reflecting severe, chronic stress.
Genetics and Immunology: The Attack on Self
- Genetics: She had genetic markers indicating a predisposition to high oxidative stress and issues with her glutathione pathway, the body’s master antioxidant.
- Cytomegalovirus (CMV): Her IgG was positive, indicating a past infection. Reactivation of latent viruses like CMV and Epstein-Barr Virus (EBV) is a common feature of Long COVID.
- Brain Autoimmunity: The most concerning finding was evidence of brain autoimmunity and brain inflammation. Her symptoms were not just “in her head”; they were the result of an inflammatory process affecting her central nervous system.
The Physiology of Long COVID: A Cascade of Dysfunction
Let’s synthesize this information. The SARS-CoV-2 spike protein binds to the ACE2 receptor, triggering a cascade of events:
- Endothelial Damage: The virus attacks the endothelium, the inner lining of blood vessels, leading to endotheliitis, inflammation, and a pro-clotting state.
- Mitochondrial Hijacking: The virus hijacks the mitochondria to replicate, draining the cell of energy and creating massive oxidative stress. This is the root of the profound fatigue.
- Immune Dysregulation: The immune response becomes chaotic, leading to exhaustion (leukopenia) and the production of autoantibodies that attack the body’s own tissues, including the brain.
- Neuroinflammation: The spike protein can cross the blood-brain barrier, triggering inflammation that injures regions such as the area postrema, a brainstem chemosensor. This leads to brain fog, headaches, dizziness, and dysautonomia.
This is a complex, vicious cycle. Inflammation drives mitochondrial dysfunction, which creates more inflammation.
A Phased Treatment Protocol: Rebuilding from the Ground Up
Given this complexity, the treatment must be comprehensive, personalized, and phased.
Phase 1: Foundational Support and Calming the System
- Oral Supplementation:
- Nutritional Support: A comprehensive medical food shake and a multivitamin.
- Mitochondrial Cocktail: High-dose CoQ10, L-carnitine, D-ribose, and magnesium.
- Adrenal Support: An adrenal adaptogen formula and potassium.
- Peptide Therapy: We started with gentle peptides.
- KPV: A small peptide fragment that is powerfully anti-inflammatory, especially in the gut.
- Thymosin Alpha-1 & Beta-4: To begin immune modulation and tissue repair.
- Photobiomodulation (Light Therapy): To support mitochondrial function systemically.
Phase 2: Deeper Healing and Cellular Regeneration
- Phosphatidylcholine (PPC) + Glutathione (GSH): A cornerstone IV therapy to repair damaged cell membranes and combat oxidative stress.
- Hyperbaric Oxygen Therapy (HBOT): She did 40 sessions. In an HBOT chamber, you breathe 100% oxygen under pressure. This floods tissues with oxygen, reducing inflammation, promoting new blood vessel growth (angiogenesis), mobilizing stem cells, and healing the brain.
- BioCharger: Before each HBOT session, she used the BioCharger, which uses light, frequencies, and PEMF to charge the body’s cells.
This multi-modal approach is not a quick fix. It is a systematic process of removing dysfunction while providing the raw materials and energetic support the body needs to heal itself, from the mitochondria up.
Case Study Workshop: Deconstructing Complexity
Now, let’s roll up our sleeves and apply these principles to a real-world scenario. This is the kind of complex case that walks into my office every day.
The Patient Profile
Our patient is a 45-year-old woman in a strained marriage, a significant source of chronic stress. She presents with a long list of symptoms and an even longer list of supplements.
Chief Complaints & History:
- Weight Gain: “Fluffy” weight gain around the middle.
- Stress & Eating Habits: She is a self-professed stress eater who craves bowls of cereal or nachos.
- Fatigue & Energy Dysregulation: Low energy in the middle of the day.
- Sleep Disruption: Wakes frequently at night.
- Gastrointestinal Issues: “Always” constipated, significant bloating, and floating stools.
- Sinus & Allergy Symptoms: Chronic sinus problems, itching, and watery eyes—a major red flag for gut issues.
- Cognitive & Mood Issues: Anxiety and “perseverates” on thoughts.
Current Regimen (The “Throw Everything at It” Approach):
- Phentermine: An amphetamine-like appetite suppressant.
- Caffeine: Consumed throughout the day.
- BPC-157, CJC-1295 / Ipamorelin, a “Vegan Cleanser,” Melatonin, and a laundry list of other supplements.
This is a classic case of a highly motivated patient who is completely lost. She is throwing dozens of interventions at the problem without a coherent strategy, and nothing is really working.
Initial Laboratory Findings & Analysis
We ran comprehensive labs, including a DUTCH test and a blood panel.
- DUTCH Test (Hormones): Her cortisol pattern is dysregulated—likely high at night (poor sleep) and blunted during the day (midday fatigue). She’s in a state of HPA axis dysfunction, or “adrenal fatigue.”
- Blood Panel:
- Thyroid Peroxidase (TPO) Antibodies: Elevated at 8.34 (top of range is 9.0), indicating she is on the cusp of Hashimoto’s thyroiditis.
- Analysis: She is stuck in a classic “wired and tired” cycle driven by chronic stress. She is using stimulants (Phentermine, caffeine) to function and a sedative (Melatonin) to sleep. Her gut is a mess, driving systemic inflammation that is now manifesting as autoimmunity against her thyroid.
Clinical Approach
Let me walk you through the protocol we actually implemented.
Phase 1: Stop the Noise and Calm the System
- Dampen the Stress Response: First, we got her off stimulants and managed her cortisol levels. We started her on Selank, a neuropeptide known for its potent anti-anxiety effects. Why Selank? Her stress eating is a classic cortisol-induced carbohydrate craving. By calming the stress response with Selank, we reduce cravings at their source.
- Address the Gut Dysbiosis: Her gut is a disaster. We initiated a “kill” phase using antimicrobial agents like berberine and grapefruit seed extract. This was followed by a “repair” phase with L-glutamine, zinc carnosine, and BPC-157 (used at the right time!).
- Improve Insulin Sensitivity: Cortisol dysregulation has made her insulin-resistant. We used a combination of Alpha-Lipoic Acid (ALA), Chromium, and Berberine to help her body handle carbohydrates more effectively.
- Identify Food Triggers: Given her symptoms, food sensitivities are a certainty. We recommended a comprehensive food allergy/sensitivity test to identify and remove inflammatory triggers.
Phase 2: Rebuilding and Optimizing
Once the inflammation was down, we moved on to rebuilding, which included:
- Hormone Modulation: Carefully balancing her estrogen, progesterone, and testosterone.
- Thyroid Support: Providing nutrients like iodine and selenium.
- Targeted Peptide Therapy: Strategically using peptides like Tesamorelin, a GHRH analog that is particularly effective at reducing visceral adipose tissue—the dangerous fat around the organs driven by cortisol.
This systematic, hierarchical approach is key. We didn’t just add more supplements. We removed triggers, calmed the system, addressed root causes in order of priority (Stress/HPA Axis -> Gut -> Insulin Resistance), and rebuilt on a solid foundation.
The Power of GLP-1 Agonists: A Modern Tool for Metabolic Reset
In our discussion of metabolic health, it’s impossible to ignore one of the most significant breakthroughs in recent years: the class of medications known as GLP-1 (Glucagon-Like Peptide-1) receptor agonists. These include drugs like Semaglutide (Ozempic/Wegovy) and Tirzepatide (Mounjaro). While often sensationalized as simple “weight loss drugs,” their physiological effects are far more profound.
Let’s look at a case that illustrates their impact. This is a male patient with classic signs of metabolic syndrome.
Baseline Labs (Before GLP-1 Therapy):
- A1c: 6.1% (pre-diabetic)
- Fasting Glucose: 105 mg/dL (impaired)
- Triglycerides: 201 mg/dL (high)
- Total Testosterone: 296 ng/dL (low)
- SHBG (Sex Hormone-Binding Globulin): 38 nmol/L (high, binding up his testosterone)
This is a picture of severe insulin resistance. The high insulin is driving down his testosterone and driving up his SHBG, creating a vicious cycle: low testosterone leads to more fat and less muscle, which worsens insulin resistance, which further suppresses testosterone.
Now, let’s look at his labs after treatment with a GLP-1 agonist, combined with lifestyle changes.
Follow-Up Labs (After GLP-1 Therapy):
- A1c: 5.2% (optimal)
- Fasting Glucose: 85 mg/dL (optimal)
- Triglycerides: 75 mg/dL (excellent)
- Total Testosterone: 550 ng/dL (significant improvement)
- SHBG: 25 nmol/L (lowered, freeing up more testosterone)
The transformation is remarkable. GLP-1 agonists work through several key mechanisms:
- They Mimic a Natural Gut Hormone: GLP-1 signals the pancreas to release insulin, suppresses glucagon, and slows gastric emptying, making you feel full longer.
- They Work on the Brain: They activate receptors in the hypothalamus, the brain’s appetite-control center, thereby directly reducing hunger signals and cravings.
- They Improve Insulin Sensitivity: By reducing the glucose load and promoting weight loss, they dramatically increase the body’s sensitivity to insulin.
In this patient, breaking the cycle of insulin resistance restored his body’s natural hormonal cascade. As his insulin came down, his SHBG dropped, his pituitary sent a stronger signal to his testes, and his testosterone production came back online. The weight loss was a sign of a fundamental metabolic reset. It’s crucial to understand that these are powerful tools that must be used as part of a comprehensive program. But for the right patient, they can provide the leverage needed to break free and regain control of their health.
Summary, Conclusion, and Key Insights
Summary
This educational post has navigated a broad and complex landscape of modern regenerative and functional medicine from my perspective as Dr. Jimenez (DC, FNP-APRN). We began by establishing the foundational concept of pleiotropism, illustrating how natural molecules and advanced therapies act as “Swiss Army knives” to produce multifaceted healing responses. We transitioned to the pragmatic realities of clinical practice, detailing the strategic necessity of navigating diagnostic codes and the operational challenges of implementing advanced therapies like Extracorporeal Shockwave Therapy (ESWT) and A2M injections. The core of the post focused on applying these principles through a series of detailed case studies. We explored the successful treatment of alopecia areata with peptides such as Thymosin Beta-4 (TB4) and BPC-157, the regeneration of bone around a dental implant with PRP, and the rapid recovery of musculoskeletal injuries in athletes. We undertook an extensive analysis of a complex Long COVID case, uncovering severe leukopenia, mitochondrial dysfunction, and neuroinflammation, and outlined a multi-phased treatment protocol incorporating peptides, nutritional support, and Hyperbaric Oxygen Therapy (HBOT). Finally, we deconstructed a multi-symptom case in a 45-year-old woman, demonstrating a systematic approach to identify root causes such as HPA axis dysregulation and gut dysbiosis, and to build a logical treatment plan incorporating Selank and GLP-1 agonists.
Conclusion
The landscape of medicine is shifting from a model of disease suppression to one of physiological restoration. The future of medicine lies not in finding a single magic bullet, but in a deeper understanding of the body as an interconnected, intelligent system. True healing comes from a holistic and hierarchical approach that honors this complexity. It begins with re-establishing the foundations of health: providing essential nutritional building blocks, balancing the body’s internal terrain, and calming the chronic stress responses that drive modern disease. Only then can we effectively leverage the power of advanced regenerative tools—whether they are peptides, specialized stem cells, or novel metabolic drugs—to guide the body back to a state of balance and vitality. Pathological fibrosis and chronic inflammation are not irreversible endpoints but dynamic processes that can be influenced. The role of the clinician is evolving into that of a master integrator, a strategist, and a patient advocate, skillfully combining evidence-based science with the art of individualized care to unlock the profound healing potential that resides within each person.
Key Insights
- Fascia as a Communicative Organ: The most critical shift in understanding is to view fascia not as inert tissue, but as a body-wide sensory and communication system that actively directs healing and biomechanical function.
- Myofibroblasts are a Double-Edged Sword: While essential for acute healing, the chronic activation of myofibroblasts is the central villain in the story of fibrosis and many chronic pain syndromes. The primary therapeutic goal should be to turn off these “on” signals.
- Hormesis is the Master Principle of Healing: The body adapts and grows stronger in response to controlled stress. Regenerative therapies like ESWT and HBOT work by applying a targeted stressor that provokes a powerful, positive adaptive response. The healing is in the reaction, not the stimulus itself.
- Peptides as Master Regulators: Peptides like Thymosin Alpha-1, Thymosin Beta-4, and BPC-157 are sophisticated signaling molecules that can precisely modulate the immune system, orchestrate complex tissue repair, and reduce inflammation.
- Mitochondrial Health is Paramount: Profound fatigue and systemic dysfunction, especially in chronic conditions like Long COVID, are often rooted in mitochondrial damage. Therapies that support mitochondrial function are critical for restoring vitality.
- Long COVID is a Multi-System Disease: a complex syndrome driven by a vicious cycle of endothelial damage, mitochondrial dysfunction, immune dysregulation, and neuroinflammation that requires a comprehensive, multimodal approach.
- Biochemical Individuality is Paramount: Even genetically identical twins diverge based on life experiences, mandating that all treatment plans must be uniquely tailored to the individual’s biography and physiology.
- Systemic Problems Require Systemic Solutions: Seemingly unrelated symptoms often stem from a common root of systemic inflammation. Effective treatment requires looking beyond the site of pain to address the entire physiological environment.
References & Keywords
Keywords:
Peptide Therapy, BPC-157, Thymosin Beta-4, TB-500, Thymosin Alpha-1, GLP-1 Agonists, Regenerative Medicine, Functional Medicine, Fascia, Extracellular Matrix (ECM), Myofibroblast, Fibrosis, Extracorporeal Shockwave Therapy (ESWT), Mechanotransduction, Hormesis, Alpha-2-Macroglobulin (A2M), Photobiomodulation (PBM), Long COVID, PASC, Alopecia Areata, Autoimmunity, Oral Health, Dental Cavitations, Platelet-Rich Plasma (PRP), Musculoskeletal Injury, Mitochondrial Dysfunction, Neuroinflammation, Hyperbaric Oxygen Therapy (HBOT), HPA Axis Dysfunction, Insulin Resistance, Post-Traumatic Osteoarthritis, Cellular Memory, Dezawa MUSE Cells, Clinical Integrity, Informed Consent, Dr. Alexander Jimenez.
References (Illustrative Examples of Supporting Literature):
- d’Agostino, M. C., Craig, K., Tibalt, E., & Respizzi, S. (2015). Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. International Journal of Surgery, 24, 147-153.
- Gabbiani, G. (2003). The myofibroblast in wound healing and fibrocontractive diseases. Journal of Pathology, 200(4), 500-503.
- Goldstein, A. L., Hannappel, E., & Kleinman, H. K. (2007). Thymosin β4: a multi-functional regenerative peptide. Expert Opinion on Biological Therapy, 7(5), 671-678.
- Lechner, J., & von Baehr, V. (2014). RANTES and fibroblast growth factor 2 in jawbone cavitations: triggers for systemic disease? International Journal of General Medicine, 7, 277–290.
- Mattson, M. P. (2008). Hormesis defined. Ageing Research Reviews, 7(1), 1-7.
- Pretorius, E., Venter, C., & Laubscher, G. J. (2021). Prevalence of symptoms and comorbidities, and their association with T-cell activation and platelet-leukocyte aggregates, in a cohort of convalescent COVID-19 patients. Cardiovascular Diabetology, 20(1), 1-15.
- Robbins, T., Glyn, M., Bouteleux, C., & et al. (2022). Hyperbaric oxygen therapy for the treatment of long COVID: a randomised controlled trial. The Lancet Regional Health – Europe, 21, 100462.
- Schleip, R., Jäger, H., & Klingler, W. (2012). What is ‘fascia’? A review of different nomenclatures. Journal of Bodywork and Movement Therapies, 16(4), 496-502.
- Seiwerth, S., Birač, K., Vukojević, J., Kos, K., & Sikirić, P. (2021). Brain-gut axis and pentadecapeptide BPC 157: Theoretical and practical implications. CNS & Neurological Disorders-Drug Targets, 20(4), 304-314.
- Wang, S., Wei, X., Zhou, J., Zhang, J., Li, K., & He, C. (2014). Identification of α2-macroglobulin as a master inhibitor of cartilage-degrading enzymes in obscene, and its synergistic anti-inflammatory effects with platelet-rich plasma. Arthritis & Rheumatology, 66(7), 1843-1853.
- Wirth, K., & Scheibenbogen, C. (2021). A Unifying Hypothesis of the Pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Vicious Circle of Low-Grade Neuroinflammation and Dysfunctional Autoimmunity. Journal of Clinical Medicine, 10(15), 3418.
- Dezawa, M., et al. (2004). Specific Isolation of Multilineage-differentiating Stress Enduring (Muse) Cells from Human Bone Marrow. Journal of Stem Cells & Regenerative Medicine.
Disclaimer
The information provided in this post is for educational and informational purposes only and is not intended as medical advice. The content is not a substitute for professional medical advice, diagnosis, or treatment. The content reflects the clinical opinions and perspectives of Dr. Jimenez, based on her education, training, and experience. It should not be interpreted as a recommendation for a specific treatment plan, product, or course of action.
All individuals must obtain recommendations for their personal health situations from their own licensed medical providers. Do not disregard professional medical advice or delay in seeking it because of something you have read in this post. Reliance on any information provided here is solely at your own risk. The case studies presented are individual experiences and do not guarantee similar outcomes for others. Always consult your physician or another qualified health care provider with any questions you may have about a medical condition.