Chiropractic Care: Your Path to Recovery After a Motor Vehicle Accident

Healing After a Car Crash: How Chiropractic and Integrative Medicine Can Restore Your Health
Motor vehicle accidents (MVAs) can leave you feeling shaken, sore, and uncertain about your health. Even minor collisions can cause injuries that linger, affecting your daily life. Musculoskeletal injuries, nerve damage, and back or neck pain are common after a motor vehicle accident (MVA). Still, the good news is that chiropractic care, when combined with integrative medicine, offers a powerful and non-invasive way to heal. This blog post explores how chiropractic treatments, led by experts like Dr. Alexander Jimenez in El Paso, Texas, can help you recover from MVA injuries. We’ll dive into the science behind these injuries, the role of advanced diagnostics, and how a holistic approach—including nutrition and health coaching—can restore your well-being.
Understanding Motor Vehicle Accident Injuries
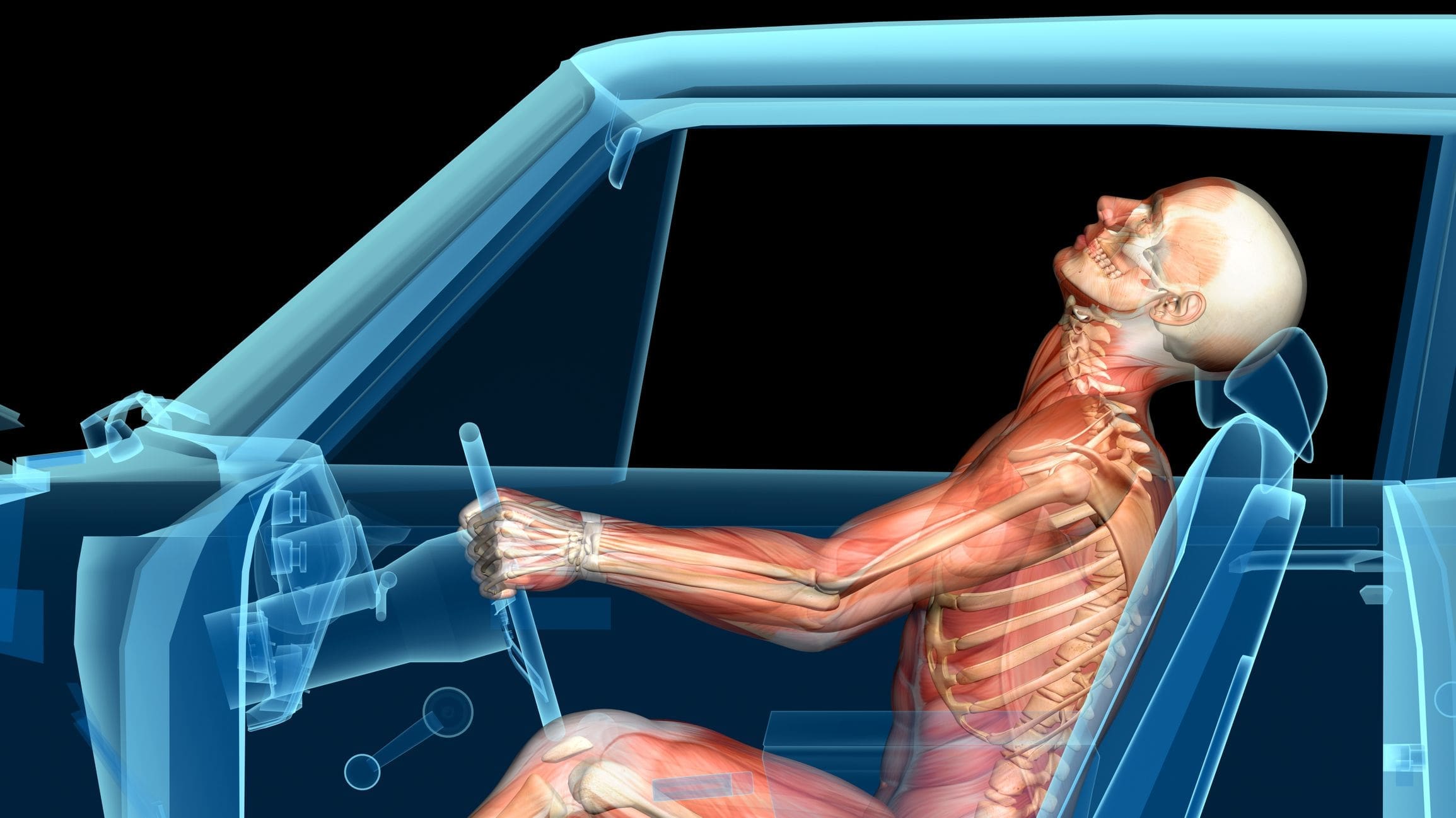
The Impact of MVAs on Your Body
When a car accident occurs, the sudden force can jolt your body in ways it’s not designed to handle. Whether it’s a rear-end collision, a side impact, or a rollover, the energy from the crash transfers to your muscles, joints, and nerves. Common injuries include:
- Whiplash: A rapid back-and-forth motion of the neck, often causing muscle strain, ligament sprains, and nerve irritation.
- Back Pain: The spine, particularly the lower back, can be affected by herniated discs, muscle strains, or misalignments.
- Neck Pain: Beyond Whiplash, Neck Pain Can Stem from Soft Tissue Damage or Joint Dysfunction.
- Nerve Injuries: Compressed or irritated nerves can cause tingling, numbness, or shooting pain.
- Soft Tissue Injuries: Muscles, tendons, and ligaments can tear or stretch, resulting in swelling and reduced mobility.
These injuries may not always be immediately apparent. Symptoms such as stiffness or mild discomfort can worsen over several days or weeks, making early treatment critical (The Winchester Institute, n.d.).
Why MVAs Cause Such Diverse Injuries
The human body is a complex system, and MVAs disrupt its balance. The spine, which houses the spinal cord and supports your posture, is particularly vulnerable to injury. When a collision forces your spine out of alignment, it can pinch nerves, strain muscles, and inflame joints. This cascade of effects often leads to chronic pain if left untreated (Miami Chiropractors, n.d.).
Dr. Alexander Jimenez, a chiropractor and nurse practitioner in El Paso, emphasizes that MVAs can cause “viscerosomatic disturbances,” where physical trauma affects both the body’s structure and its internal functions. His clinical observations highlight how misalignments (subluxations) in the spine can disrupt nerve communication, leading to pain and reduced mobility (Jimenez, 2025).
Citations
- The Winchester Institute. (n.d.). The role of chiropractic adjustments in treating car accident injuries. Retrieved from https://www.thewinchesterinstitute.com/chiropractor-dublin-ohio/wellness-blog/the-role-of-chiropractic-adjustments-in-treating-car-accident-injuries
- Miami Chiropractors. (n.d.). The role of chiropractic care in rehabilitation after a car accident. Retrieved from https://www.miami-chiropractors.com/the-role-of-chiropractic-care-in-rehabilitation-after-a-car-accident/
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
The Role of Chiropractic Care in MVA Recovery
What Is Chiropractic Care?
Chiropractic care focuses on restoring the body’s natural alignment, particularly in the spine, to promote healing and relieve pain. Chiropractors use hands-on techniques, such as spinal adjustments, to correct misalignments and improve joint function. Unlike surgery or medication, chiropractic care is a non-invasive option, making it a safe choice for many MVA victims (Apex Orthopedic Spine & Neurology, n.d.).
How Chiropractic Helps MVA Injuries
Chiropractic treatments target the root causes of MVA-related pain and dysfunction. Here’s how they work:
- Correcting Misalignments: Spinal adjustments realign vertebrae, reducing pressure on nerves and improving mobility. This is especially effective for whiplash and back pain (Quantum Chiropractic, n.d.).
- Reducing Inflammation: Techniques such as soft tissue therapy and electrical stimulation help decrease swelling in muscles and joints, thereby speeding up recovery (Pacific Coast Injury Group, 2025).
- Restoring Range of Motion: Rehabilitative exercises and stretches help rebuild strength and flexibility, preventing stiffness (DeBruin Chiropractic, n.d.).
- Relieving Nerve Pain: By addressing spinal misalignments, chiropractors can alleviate nerve compression, thereby reducing symptoms such as tingling or numbness (Brookdale Health, n.d.).
Dr. Jimenez’s approach integrates these techniques with his dual expertise as a chiropractor and nurse practitioner. His ability to combine biomechanical corrections with medical diagnostics ensures a comprehensive treatment plan tailored to each patient’s needs (Jimenez, 2025).
Benefits of Early Chiropractic Intervention
Seeking chiropractic care within 72 hours of a motor vehicle accident (MVA) can make a significant difference. Early treatment reduces inflammation, prevents scar tissue buildup, and lowers the risk of chronic pain. It also supports legal claims by documenting injuries promptly, which is crucial for personal injury cases (MVA MVP, n.d.).
Citations
- Apex Orthopedic Spine & Neurology. (n.d.). Should I see a chiropractor after a car accident? Retrieved from https://www.apexosn.com/should-i-see-chiropractor-after-a-car-accident/
- Quantum Chiropractic. (n.d.). 6 reasons chiropractic care can help after a car accident. Retrieved from https://quantumchiropt.com/6-reasons-chiropractic-care-can-help-after-a-car-accident/
- Pacific Coast Injury Group. (2025). Chiropractic care for auto accident injuries. Retrieved from https://pacificcoastinjurygroup.com/2025/01/31/chiropractic-care-for-auto-accident-injuries/
- DeBruin Chiropractic. (n.d.). June newsletter: How chiropractic treatments can improve your range of motion. Retrieved from https://debruinchiropractic.com/articles/966741-june-newsletter-how-chiropractic-treatments-can-improve-your-range-of-motion
- Brookdale Health. (n.d.). Why chiropractic care is essential after a car accident. Retrieved from https://www.brookdalehealth.com/blog/why-chiropractic-care-is-essential-after-a-car-accident.html
- MVA MVP. (n.d.). Why chiropractic care is essential after a motor vehicle accident. Retrieved from https://mvamvp.com/why-chiropractic-care-is-essential-after-a-motor-vehicle-accident/
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
Dr. Alexander Jimenez: A Leader in MVA Recovery
Who Is Dr. Jimenez?
Dr. Alexander Jimenez, DC, APRN, FNP-BC, is a board-certified chiropractor and family nurse practitioner based in El Paso, Texas. With over 25 years of experience, he runs the Injury Medical & Chiropractic Clinic, specializing in injuries related to motor vehicle accidents (MVA). His dual licensure allows him to bridge chiropractic care with medical diagnostics, offering a unique, integrative approach to healing (Jimenez, 2025).
Dr. Jimenez’s Clinical Rationale
Dr. Jimenez’s treatment philosophy centers on addressing the root causes of injuries rather than masking symptoms. He utilizes advanced imaging techniques (such as X-rays and MRIs), dual-scope procedures (combining chiropractic and medical assessments), and diagnostic tools to create precise treatment plans. His approach is grounded in the following principles:
- Biomechanical Restoration: Correcting spinal misalignments to restore nerve function and reduce pain.
- Systemic Healing: Addressing metabolic and hormonal imbalances that can delay recovery.
- Legal Documentation: Providing detailed medical records to support personal injury claims, ensuring patients receive fair compensation.
His clinic’s multidisciplinary team, including nutritionists, physical therapists, and health coaches, works together to promote long-term wellness (Jimenez, 2025).
Success Stories from El Paso
Dr. Jimenez has treated thousands of MVA victims in El Paso, earning a reputation as a trusted provider. Patient testimonials highlight his compassionate, patient-centered care. For example, one patient described how Dr. Jimenez’s adjustments and nutritional guidance relieved chronic neck pain after a rear-end collision, allowing them to return to work pain-free (Jimenez, 2025).
Citations
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
Advanced Diagnostics in MVA Treatment
The Role of Imaging and Assessments
Accurate diagnosis is the foundation of effective MVA treatment. Dr. Jimenez utilizes advanced imaging techniques, including X-rays and MRIs, to detect hidden injuries such as disc herniations or fractures. These tools help pinpoint the exact location and severity of damage, guiding treatment decisions (Alexander Orthopaedics, n.d.).
Dual-scope procedures, which combine chiropractic and medical evaluations, offer a comprehensive view of a patient’s health. For instance, a patient with neck pain might undergo a chiropractic exam to assess spinal alignment and a medical assessment to check for nerve damage or inflammation. This holistic approach ensures no aspect of the injury is overlooked (Jimenez, 2025).
Why Diagnostics Matter for Legal Cases
In personal injury cases, detailed medical documentation is essential. Dr. Jimenez’s clinic provides thorough reports that link a patient’s injuries to the MVA, strengthening legal claims. These records include imaging results, clinical findings, and treatment progress, helping attorneys build a strong case for compensation (MVA MVP, n.d.).
Citations
- Alexander Orthopaedics. (n.d.). 5 car accident treatments. Retrieved from https://alexanderorthopaedics.com/blog/5-car-accident-treatments/
- MVA MVP. (n.d.). Why chiropractic care is essential after a motor vehicle accident. Retrieved from https://mvamvp.com/why-chiropractic-care-is-essential-after-a-motor-vehicle-accident/
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
Integrative Medicine: A Holistic Approach
Beyond Chiropractic: The Power of Integrative Care
While chiropractic care is highly effective, combining it with integrative medicine can further enhance recovery. Integrative medicine addresses the whole person—body, mind, and lifestyle. Dr. Jimenez’s clinic incorporates:
- Nutrition: Personalized diet plans reduce inflammation and support tissue repair. For example, foods rich in omega-3 fatty acids and antioxidants can accelerate healing (Square One Health, n.d.).
- Health Coaching: Virtual or in-person coaching helps patients adopt healthy habits, manage stress, and stay motivated.
- Physical Rehabilitation: Targeted exercises rebuild strength and prevent re-injury.
- Acupuncture and Electro-Acupuncture: These techniques relieve pain and stimulate healing in soft tissues (Total Vitality Medical, n.d.).
Nutrition’s Role in Recovery
After an MVA, inflammation can slow healing and worsen pain. Dr. Jimenez’s nutritional counseling emphasizes the consumption of anti-inflammatory foods, including leafy greens, fatty fish, and berries. He also recommends supplements like turmeric or vitamin D to support recovery. By addressing nutritional deficiencies, patients can heal more quickly and experience improved overall well-being (Jimenez, 2025).
Health Coaching for Long-Term Wellness
Health coaching empowers patients to take control of their recovery. Coaches work with patients to set goals, such as improving mobility or reducing stress, and provide practical strategies to help them achieve these objectives. This personalized support is especially valuable for MVA victims dealing with emotional trauma or chronic pain (Jackson Healing Arts, n.d.).
Citations
- Square One Health. (n.d.). Chiropractic care for back pain relief: How chiropractors can help. Retrieved from https://squareonehealth.com/chiropractic-care-for-back-pain-relief-how-chiropractors-can-help/
- Total Vitality Medical. (n.d.). Car accident injuries treated by chiropractors. Retrieved from https://totalvitalitymedical.com/news/car-accident-injuries-treated-by-chiropractors/
- Jackson Healing Arts. (n.d.). Why chiropractic care should be part of your post-car accident treatment plan. Retrieved from https://www.jacksonhealingarts.com/why-chiropractic-care-should-be-part-of-your-post-car-accident-treatment-plan/
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
The Science Behind Chiropractic and Integrative Medicine
Evidence Supporting Chiropractic Care
Research supports the effectiveness of chiropractic care for motor vehicle accident (MVA) injuries. A 2020 study in the Spine Journal found that spinal manipulative therapy significantly reduces pain and disability in patients with chronic low back pain (Rubinstein et al., 2020). Another study in the Journal of Clinical Endocrinology & Metabolism linked cortisol imbalances to chronic pain, suggesting that patients require holistic treatments that address stress and inflammation (Hannibal et al., 2019).
Integrative Medicine and Long-Term Health
Functional medicine, a key component of Dr. Jimenez’s practice, focuses on root-cause analysis. By assessing factors such as nutrition, stress, and hormonal balance, functional medicine helps prevent chronic conditions like fibromyalgia or arthritis from developing after a motor vehicle accident (MVA). This approach aligns with the Institute for Functional Medicine’s protocols, which emphasize personalized care (Jimenez, 2025).
Citations
- Rubinstein, S. M., de Zoete, A., van Middelkoop, M., Assendelft, W. J. J., de Boer, M. R., & van Tulder, M. W. (2020). Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: Systematic review and meta-analysis of randomised controlled trials. Spine Journal, 20(4), 602-614. https://doi.org/10.1016/j.spinee.2019.10.014
- Hannibal, K. E., & Bishop, M. D. (2019). Chronic stress, cortisol dysfunction, and pain: A psychoneuroendocrine rationale for stress management in pain rehabilitation. Journal of Clinical Endocrinology & Metabolism, 104(12), 5627-5636. https://doi.org/10.1210/jc.2019-00889
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
Practical Tips for MVA Recovery
What to Do After an Accident
- Seek Medical Attention: Visit a chiropractor or doctor within 72 hours, even if you feel fine. Early assessment catches hidden injuries.
- Document Everything: Keep records of medical visits, symptoms, and treatments for legal and insurance purposes.
- Follow Your Treatment Plan: Attend all scheduled chiropractic sessions and adhere to the provided nutrition and exercise recommendations.
- Manage Stress: Practice relaxation techniques, such as deep breathing, to support emotional and physical well-being.
Choosing the Right Chiropractor
Look for a provider with experience in managing MVA injuries, such as Dr. Jimenez. Verify credentials, read patient reviews, and confirm that they offer integrative services such as nutrition counseling or rehabilitation. A chiropractor who collaborates with other specialists, such as physical therapists or attorneys, can provide comprehensive care (Cesak Chiropractic, n.d.).
Citations
- Cesak Chiropractic. (n.d.). How chiropractic care can help after an auto accident injury. Retrieved from https://www.cesakchiropractic.com/blog/1276560-how-chiropractic-care-can-help-after-an-auto-accident-injury
Conclusion: Your Road to Recovery
Motor vehicle accidents can significantly disrupt your life, but chiropractic care and integrative medicine offer a path to recovery and healing. By addressing musculoskeletal injuries, nerve damage, and pain through spinal adjustments, soft tissue therapies, and holistic strategies, providers like Dr. Alexander Jimenez help patients recover fully. His use of advanced diagnostics, dual-scope procedures, and personalized care ensures both medical and legal needs are met. Whether you’re dealing with whiplash, back pain, or emotional stress, a comprehensive approach that includes nutrition and health coaching can restore your health and quality of life.
If you’ve been in an MVA, don’t wait to seek care. Contact a qualified chiropractor today to start your journey to recovery. In El Paso, Dr. Jimenez’s Injury Medical & Chiropractic Clinic is ready to help you live pain-free and thrive.
References
- Alexander Orthopaedics. (n.d.). 5 car accident treatments. Retrieved from https://alexanderorthopaedics.com/blog/5-car-accident-treatments/
- Apex Orthopedic Spine & Neurology. (n.d.). Should I see a chiropractor after a car accident? Retrieved from https://www.apexosn.com/should-i-see-chiropractor-after-a-car-accident/
- Arizona Chiropractic & Spine. (n.d.). How chiropractic care can be a lifesaver after an auto accident. Retrieved from https://www.arizonachiropracticspine.com/blog/1294001-how-chiropractic-care-can-be-a-lifesaver-after-an-auto-accident
- Brookdale Health. (n.d.). Why chiropractic care is essential after a car accident. Retrieved from https://www.brookdalehealth.com/blog/why-chiropractic-care-is-essential-after-a-car-accident.html
- Cesak Chiropractic. (n.d.). How chiropractic care can help after an auto accident injury. Retrieved from https://www.cesakchiropractic.com/blog/1276560-how-chiropractic-care-can-help-after-an-auto-accident-injury
- DeBruin Chiropractic. (n.d.). June newsletter: How chiropractic treatments can improve your range of motion. Retrieved from https://debruinchiropractic.com/articles/966741-june-newsletter-how-chiropractic-treatments-can-improve-your-range-of-motion
- Hannibal, K. E., & Bishop, M. D. (2019). Chronic stress, cortisol dysfunction, and pain: A psychoneuroendocrine rationale for stress management in pain rehabilitation. Journal of Clinical Endocrinology & Metabolism, 104(12), 5627-5636. https://doi.org/10.1210/jc.2019-00889
- Jackson Healing Arts. (n.d.). Why chiropractic care should be part of your post-car accident treatment plan. Retrieved from https://www.jacksonhealingarts.com/why-chiropractic-care-should-be-part-of-your-post-car-accident-treatment-plan/
- Jimenez, A. (2025). Clinical observations on motor vehicle accident injuries. Retrieved from https://dralexjimenez.com/
- Jimenez, A. (2025). Functional medicine protocols for MVA recovery. Retrieved from https://chiromed.com/
- Jimenez, A. (2025). Professional profile. Retrieved from https://www.linkedin.com/in/dralexjimenez/
- Miami Chiropractors. (n.d.). The role of chiropractic care in rehabilitation after a car accident. Retrieved from https://www.miami-chiropractors.com/the-role-of-chiropractic-care-in-rehabilitation-after-a-car-accident/
- Miami Chiropractors. (n.d.). Why you should see a chiropractor even for minor injuries after a car accident. Retrieved from https://www.miami-chiropractors.com/why-you-should-see-a-chiropractor-even-for-minor-injuries-after-a-car-accident/
- MVA MVP. (n.d.). Why chiropractic care is essential after a motor vehicle accident. Retrieved from https://mvamvp.com/why-chiropractic-care-is-essential-after-a-motor-vehicle-accident/
- Pacific Coast Injury Group. (2025). Chiropractic care for auto accident injuries. Retrieved from https://pacificcoastinjurygroup.com/2025/01/31/chiropractic-care-for-auto-accident-injuries/
- Quantum Chiropractic. (n.d.). 6 reasons chiropractic care can help after a car accident. Retrieved from https://quantumchiropt.com/6-reasons-chiropractic-care-can-help-after-a-car-accident/
- Rubinstein, S. M., de Zoete, A., van Middelkoop, M., Assendelft, W. J. J., de Boer, M. R., & van Tulder, M. W. (2020). Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: Systematic review and meta-analysis of randomised controlled trials. Spine Journal, 20(4), 602-614. https://doi.org/10.1016/j.spinee.2019.10.014
- Square One Health. (n.d.). Chiropractic care for back pain relief: How chiropractors can help. Retrieved from https://squareonehealth.com/chiropractic-care-for-back-pain-relief-how-chiropractors-can-help/
- The Winchester Institute. (n.d.). The role of chiropractic adjustments in treating car accident injuries. Retrieved from https://www.thewinchesterinstitute.com/chiropractor-dublin-ohio/wellness-blog/the-role-of-chiropractic-adjustments-in-treating-car-accident-injuries
- Total Vitality Medical. (n.d.). Car accident injuries treated by chiropractors. Retrieved from https://totalvitalitymedical.com/news/car-accident-injuries-treated-by-chiropractors/