Cobb Angle: From Measurement to Treatment Decisions
The Cobb angle is a mathematical measurement tool for assessing the curvature of the spine. Along with physical exams and other tests, how is it used to evaluate scoliosis and kyphosis of the spine?
Cobb Angle
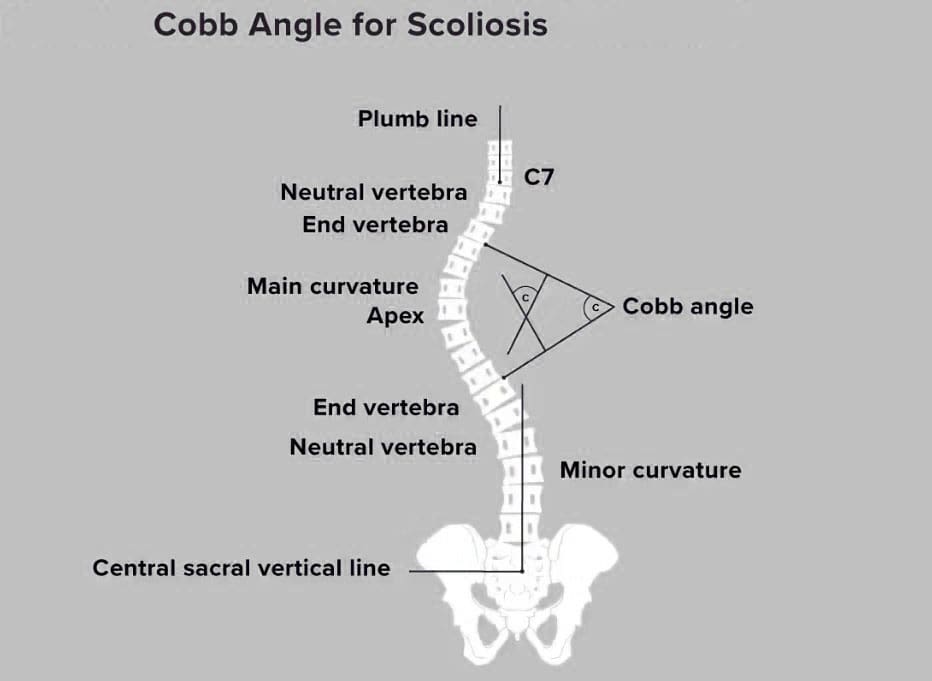
The Cobb angle is used to quantify the curvature of the spine, particularly in conditions like scoliosis. It measures the degree of side-to-side spinal curvature, a deformity called scoliosis. The angle’s size helps determine what kind of treatment is needed. Monitoring may be all that’s necessary for mild curvature. With severe scoliosis, treatment may require spinal fusion surgery. Named for orthopedic surgery pioneer John Robert Cobb, it describes the distance a scoliotic curve may deviate from being straight. (Botterbush K. S. et al., 2023) Generally, it takes at least 10 degrees of deviation from straight before scoliosis is confirmed.
X-Ray and Interpretation
An X-ray is taken to measure the Cobb angle. Side and back views are taken. The healthcare provider or examiner then views the X-rays and locates the most affected vertebra in the curve, called the apical vertebra. In a scoliotic curve, the apical vertebra is the spinal bone with the greatest degree of rotation that takes the biggest curve away from the center of a normal spine column.
Visualizing the Angle
The apical vertebra is where two lines drawn from the X-rays meet. Two lines are drawn along the edge of the top and bottom bones of the curve. The lines extend out as follows:
- On the top bone, the line starts on the high side, continues along the top edge, and then slopes down according to the angle of the vertebra. (Jin, C. et al., 2022)
- On the bottom vertebra, the line starts on the low side, continues along the bottom edge, and slopes upward.
- The Cobb angle is found by measuring the angle of the two intersecting lines where they meet.
Then, the top and bottom vertebrae of the side-to-side curve are identified to create a number for the Cobb angle. These bones have the most tilt but the least rotation and displacement and are located above and below the apical vertebra. Computer software is commonly used to calculate the Cobb angle. (Jin, C. et al., 2022) Treatment is based on the:
- Angle size
- Gender: Scoliosis is more common and likely to progress in females
- Probability of progression (National Scoliosis Foundation, 2015)
10 Degrees Cobb Angle
Scoliosis is diagnosed when the Cobb angle reaches 10 degrees or more. However, this is not generally considered a significant curvature (American Association of Neurological Surgeons, 2024). In around 80% of cases, the scoliosis is considered idiopathic or without congenital or other underlying causes.
Less Than 25 Degrees Cobb Angle
If a scoliotic curve is less than 25 degrees, individuals may only need to visit their healthcare provider periodically so long as the scoliosis is monitored. These are mild cases, often without symptoms, but there is a chance that the curvature can progress. This usually means reassessing the Cobb angle every four to six months in a growing child or adolescent. (National Scoliosis Foundation, 2015) A 5-degree or more progression can change the diagnosis and treatment. (Jin, C. et al., 2022)
Between 25 and 40 Degrees Cobb Angle
A Cobb angle of 25 to 40 degrees usually requires wearing a back brace and intensive physical therapy. The goal of these treatments is to help halt the curve’s progression. Braces are generally worn 16 to 23 hours every day. (National Scoliosis Foundation, 2015) The healthcare provider will provide a referral for physical therapy. Many report excellent results with the Schroth or other scoliosis-specific exercise methods. A study found that core stabilization exercise programs can decrease Cobb angles in adolescents with idiopathic scoliosis. (Ko K. J. & Kang S. J. 2017)
Scoliosis in Adults
Scoliosis is diagnosed in adults, usually in those who have had the condition, treated or not, that was identified in their youth. A study that followed various cases for 20 years found disease progression occurred in 40% of adults but was usually less than one degree per year. However, degenerative scoliosis can also occur in individuals aged 65 and older. (American Association of Neurological Surgeons, 2024)
40 Degrees or More Cobb Angle
Surgery may be recommended once the Cobb angle reaches 40 to 50 degrees. A spinal fusion is often used to force the curve to stop developing. In adults, surgery may be needed if the angle reaches 50 degrees and they experience complications, such as nerve damage or bowel/bladder dysfunction. Risk factors in adults include older age, a history of smoking, and a diagnosis of other conditions, including being overweight. (American Association of Neurological Surgeons, 2024)
Variations
Variations occur in measuring scoliosis, and it is important to understand the difference between a change in scoliosis and a change in the tools or measurement. Equipment errors, imaging errors, and the subjective reading of the healthcare provider can change the values. (Jin, C. et al., 2022) Scoliosis measurement software and intelligent medical devices continue to improve how scoliosis is evaluated and treated. Physical exams, symptoms, and careful monitoring of changes in posture or function are still critical to an accurate diagnosis. The healthcare provider will explain the Cobb angle and other test results.
Injury Medical Chiropractic & Functional Medicine Clinic
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues.
Academic Low Back Pain: Impact and Chiropractic Solutions
References
Botterbush, K. S., Zhang, J. K., Chimakurty, P. S., Mercier, P., & Mattei, T. A. (2023). The life and legacy of John Robert Cobb: the man behind the angle. Journal of neurosurgery. Spine, 39(6), 839–846. https://doi.org/10.3171/2023.7.SPINE23146
Jin, C., Wang, S., Yang, G., Li, E., & Liang, Z. (2022). A Review of the Methods on Cobb Angle Measurements for Spinal Curvature. Sensors (Basel, Switzerland), 22(9), 3258. https://doi.org/10.3390/s22093258
National Scoliosis Foundation. (2015). Scoliosis Media & Community Guide. https://www.scoliosis.org/nsf2/wp-content/uploads/2015/06/ScoliMediaGuide_9June3.pdf
American Association of Neurological Surgeons. (2024). Scoliosis. https://www.aans.org/patients/conditions-treatments/scoliosis/
Ko, K. J., & Kang, S. J. (2017). Effects of 12-week core stabilization exercise on the Cobb angle and lumbar muscle strength of adolescents with idiopathic scoliosis. Journal of Exercise Rehabilitation, 13(2), 244–249. https://doi.org/10.12965/jer.1734952.476



 Digital Pulleys
Digital Pulleys