Common Motor Vehicle Accidents in El Paso

Recovery with Integrative Care at ChiroMed – Integrated Medicine Holistic Healthcare
Motor vehicle accidents occur frequently in El Paso, Texas. The city’s position near the U.S.-Mexico border creates heavy traffic from cars and large trucks. This leads to many crashes each year. In recent data, El Paso County reported thousands of collisions, some resulting in serious injuries or fatalities. These accidents can cause a range of harms, from minor neck strain to severe conditions. At ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX, patients receive comprehensive, natural support for recovery. The clinic combines chiropractic adjustments, nurse practitioner care, rehabilitation, nutrition, and other holistic methods to address injuries fully and promote lasting wellness.
Common Types of Motor Vehicle Accidents in El Paso
El Paso’s roads face unique pressures. Major highways like I-10 and Loop 375 handle constant flow from border crossings. Trucks add extra risks due to their size and weight.
- Rear-End Collisions — These often occur when drivers tailgate or get distracted, especially during rush hour on Loop 375 or near busy areas like Cielo Vista Mall.
- Intersection Crashes — Busy crossings on streets like Mesa or Sunland Park see many wrecks from running red lights or failing to yield the right of way.
- Truck Accidents — Commercial vehicles on I-10 cause severe impacts. Border traffic increases these events, with heavy loads making outcomes more serious.
- Pedestrian Incidents — Walkers face dangers in downtown zones or near campuses when drivers speed or fail to check blind spots.
- Head-On and Side-Impact Collisions — These occur on rural roads or at intersections, often from wrong-way driving or failure to stop.
High-traffic areas like I-10, Loop 375, Montana Avenue, and Zaragoza Road account for the most incidents. Construction zones and dust storms add further hazards.
Main Causes of Accidents in El Paso
Several factors contribute to crashes in the area. Driver errors combine with road conditions and border-related traffic.
- Distracted Driving — Texting, eating, or using devices leads to many collisions, especially at intersections.
- Impaired Driving — Alcohol or drugs slow reactions, with spikes near entertainment districts on weekends.
- Speeding — Exceeding limits on highways like Loop 375 increases crash severity.
- Failure to Yield or Obey Signals — Common at stop signs and lights, causing angle impacts.
- Fatigue and Reckless Actions — Long-haul truckers may drive tired, while tailgating or lane weaving adds danger.
Weather issues, poor visibility, and construction further raise risks. These elements make El Paso a challenging place to drive safely.
Typical Injuries from Motor Vehicle Accidents
The force of a crash jolts the body suddenly, leading to various injuries. Symptoms may appear right away or develop over time.
- Whiplash — Rapid neck movement causes pain, stiffness, and headaches.
- Neck and Back Sprains/Strains — Muscle and ligament damage result in ongoing discomfort.
- Fractures — Broken bones, including ribs or limbs, from direct impact.
- Traumatic Brain Injuries (TBIs) — Concussions or more severe head trauma lead to dizziness, confusion, or memory issues.
- Soft Tissue Damage — Bruises, tears in muscles or tendons, and swelling.
- Herniated Discs — Spinal discs shift, pressing on nerves and causing radiating pain.
- Other Issues — Knee injuries from dashboard contact, shoulder strains, or emotional effects like anxiety.
Many victims experience chronic pain if not addressed early. Back and neck problems rank high among El Paso accident cases.
How ChiroMed – Integrated Medicine Supports Recovery
At ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX, care goes beyond basic treatment. The clinic uses an integrative approach that treats the whole person—body, mind, and lifestyle. Led by experts including Dr. Alexander Jimenez, DC, APRN, FNP-BC, the team blends chiropractic, functional medicine, rehabilitation, and nutrition for natural healing.
ChiroMed avoids heavy reliance on drugs or surgery. Instead, it focuses on root causes to restore balance and function.
- Chiropractic Adjustments — Gentle spinal corrections relieve nerve pressure, improve alignment, and reduce pain from whiplash or disc issues.
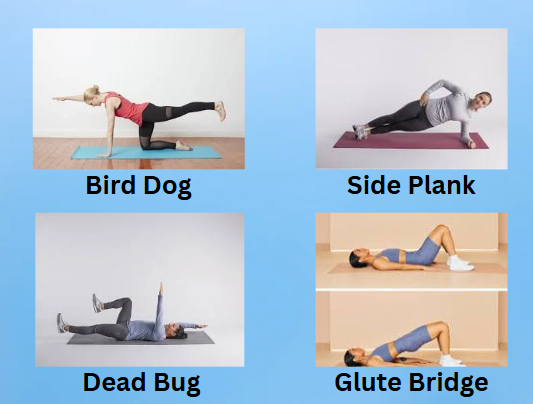
- Spinal Decompression and Rehabilitation — Non-invasive therapy eases disc pressure and builds strength through targeted exercises.
- Massage and Soft Tissue Therapies — These break up scar tissue, boost circulation, and ease stiffness in injured areas.
- Nurse Practitioner Services — Advanced assessments and care plans address complex needs, including pain management and overall health.
- Nutritional and Functional Medicine Support — Personalized plans with diet, supplements, and lifestyle guidance reduce inflammation and support healing from the inside.
- Holistic Elements — Techniques like acupuncture or electroacupuncture help with pain and stress, promoting emotional recovery too.
This combined method speeds recovery, restores mobility, and prevents long-term problems. Patients often report less pain and better daily function after starting care. Early visits—ideally within days of an accident—help catch hidden issues before they worsen.
ChiroMed’s facilities in El Paso, including locations on Vista Del Sol and others, offer modern tools like digital imaging and nerve testing. The multidisciplinary team tailors plans to each person’s needs, making recovery more effective and complete.
Expertise from Dr. Alexander Jimenez at ChiroMed
Dr. Alexander Jimenez brings extensive experience to ChiroMed. As a Doctor of Chiropractic (DC) and board-certified Family Nurse Practitioner (APRN, FNP-BC), along with certifications in functional medicine, he has practiced in El Paso for over 30 years. His dual training allows deep insight into injury recovery.
Dr. Jimenez observes that many MVA patients suffer from misalignments, inflammation, and nerve irritation, which can lead to conditions such as sciatica or chronic headaches. At ChiroMed, he uses evidence-based, non-invasive methods to address these. Adjustments, decompression, and integrative protocols help patients regain strength without invasive steps. His approach emphasizes natural restoration, with nutrition and wellness playing key roles in reducing the risk of recurrence.
Patients benefit from his focus on personalized, root-cause care that improves long-term quality of life.
Final Thoughts
Motor vehicle accidents remain a concern in El Paso due to traffic volume and border demands. Injuries like whiplash, back pain, and more can disrupt life significantly. ChiroMed – Integrated Medicine Holistic Healthcare provides a trusted path to recovery through chiropractic, nurse practitioner care, rehabilitation, and holistic support. This integrative model helps heal the body naturally while addressing emotional and lifestyle factors. If you’ve been in an accident, seeking prompt care at ChiroMed can make a real difference in your healing journey. Drive carefully, and prioritize safety on El Paso’s roads.
References
ChiroMed – Integrated Medicine Holistic Healthcare. (n.d.). Home. https://chiromed.com/
ChiroMed – Integrated Medicine Holistic Healthcare. (n.d.). Services. https://chiromed.com/services
Dr. Alexander Jimenez. (n.d.). Injury Specialists. https://dralexjimenez.com/
Jimenez, A. (n.d.). LinkedIn Profile. https://www.linkedin.com/in/dralexjimenez/
Labinoti Law Firm. (n.d.). El Paso Motor Vehicle Accident Attorney. https://www.labinotilaw.com/office-locations/el-paso/personal-injury/motor-vehicle-accident/
Harmonson Law Firm. (n.d.). El Paso Car Accident Lawyer. https://www.clarkharmonsonattorney.com/el-paso-tx/car-accident-lawyer/
Spectrum Therapy Consultants. (n.d.). Motor Vehicle Accident Injuries. https://spectrumtherapyconsultants.com/physical-therapy-services/motor-vehicle-accident-injuries/
Abrar and Vergara. (n.d.). El Paso Car Accident Statistics. https://theavlawyer.com/el-paso-car-accident-lawyer/statistics/
Arnold & Itkin. (n.d.). El Paso Truck Accidents. https://www.arnolditkin.com/el-paso-personal-injury/truck-accidents/
The Neck and Back Clinics. (n.d.). Chiropractic Treatment Options After a Car Accident. https://theneckandbackclinics.com/what-are-your-chiropractic-treatment-options-after-a-car-accident/
Altitude Health. (n.d.). Comprehensive Care for Motor Vehicle Accident Recovery. https://www.altitudehealth.ca/comprehensive-care-integrating-chiropractic-physiotherapy-naturopathy-and-more-for-motor-vehicle-accident-recovery/