Auto Accident Tips for Safe Driving Practices To Prevent WAD
Stay informed about the causes and effects of WAD (whiplash-associated disorder) from an auto accident to enhance your road awareness.
Whiplash-Associated Disorders and Cervical Spine Injuries from Motor Vehicle Accidents: A Comprehensive Guide
Whiplash-associated disorders (WAD) are no laughing matter, but let’s face it—your neck getting an unexpected rollercoaster ride during a car crash sounds like something out of a cartoon! Unfortunately, the reality is far less amusing. Motor vehicle accidents (MVAs) are a leading cause of neck injuries, particularly those affecting the cervical spine, and they can leave you feeling like you’ve been through a wrestling match with a gorilla. In this comprehensive guide, we’ll dive deep into why WAD and cervical spine injuries are so closely tied to MVAs, how they wreak havoc on your body, and what you can do to recover. We’ll also spotlight Dr. Alexander Jimenez, DC, APRN, FNP-BC, a rockstar chiropractor and nurse practitioner in El Paso, Texas, who’s helping accident victims get back on their feet with his unique blend of clinical expertise and legal know-how. Buckle up (safely, of course) for a journey through the science, symptoms, and solutions for WAD, with a sprinkle of humor to keep things light!
Why Whiplash and the Cervical Spine Take a Hit in MVAs
Picture this: you’re stopped at a red light, singing along to your favorite tune, when—BAM!—a distracted driver rear-ends you. Your body lurches forward, but your head? It’s still enjoying the karaoke moment, snapping back and forth like a bobblehead on a bumpy road. This rapid motion is the hallmark of whiplash, and it’s why the cervical spine (the seven vertebrae in your neck) often bears the brunt of MVAs.
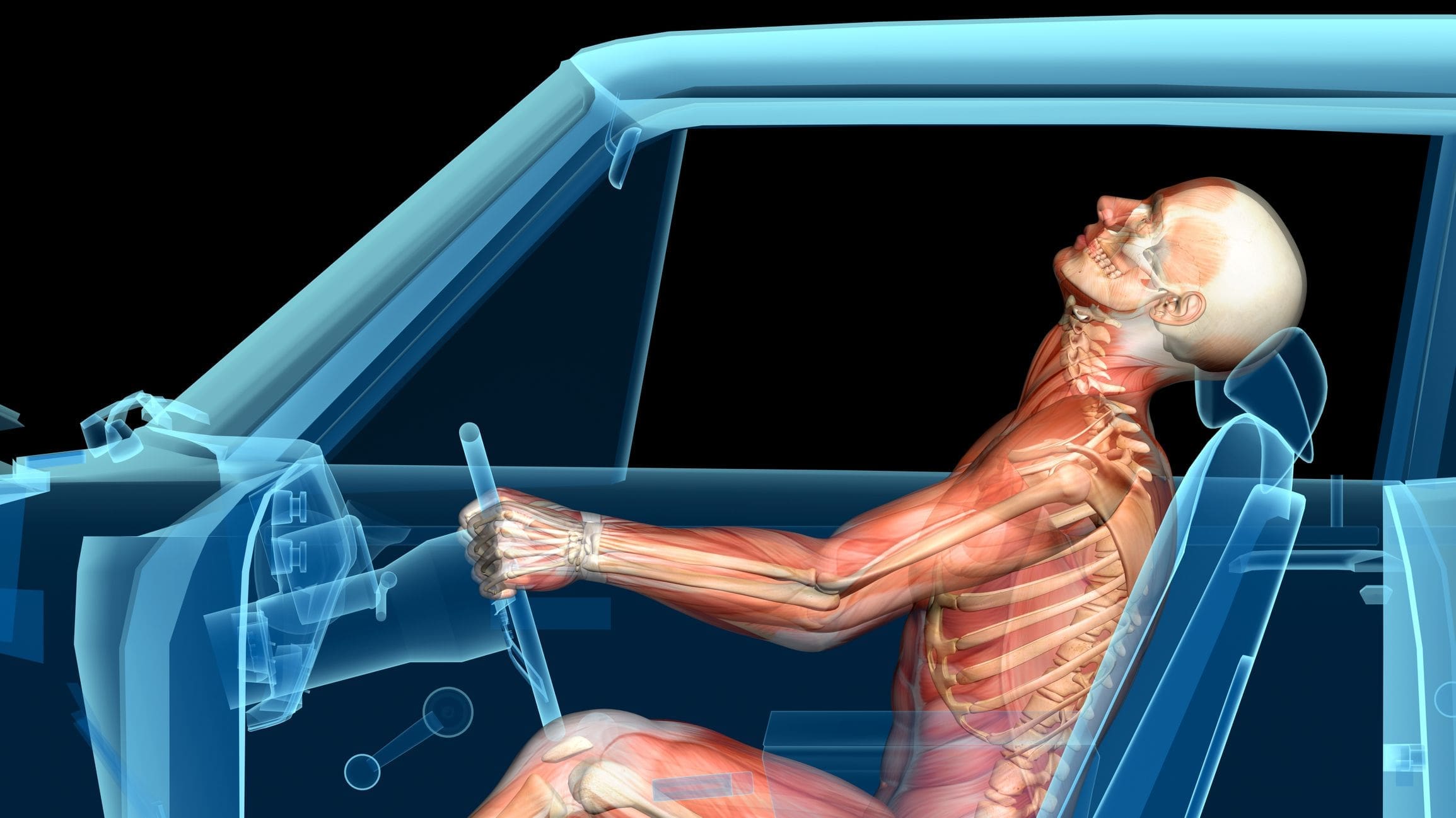
The Biomechanics of Whiplash
Whiplash occurs when the neck experiences a sudden acceleration-deceleration force, typically in rear-end collisions. The cervical spine, which supports your head (a 10-12 pound bowling ball, basically), isn’t designed for this kind of abuse. During a crash, the lower cervical vertebrae hyperextend (bend backward). In contrast, the upper ones flex forward, creating an S-shaped curve that exceeds the spine’s normal range of motion (Physiopedia, n.d.). This can strain or tear muscles, ligaments, tendons, and even discs, leading to a range of symptoms collectively known as whiplash-associated disorders.
According to the National Highway Traffic Safety Administration, over 2.1 million people in the U.S. sustain injuries in car crashes annually, with whiplash being one of the most common (NHTSA, 2023). The forces involved in even low-speed collisions (think 10-15 mph) can generate enough energy to cause soft tissue damage, nerve irritation, or spinal misalignments. It’s like your neck is trying to do gymnastics without any training!
The Cervical Spine’s Vulnerability
The cervical spine is a marvel of engineering, but it’s also a bit of a diva—delicate and prone to drama. Its vertebrae (C1-C7) are smaller and more mobile than those in the thoracic or lumbar spine, making them susceptible to injury. The muscles, ligaments, and discs in this area work together to provide flexibility and support, but they’re no match for the sudden, violent forces of an MVA. Common injuries include:
- Soft Tissue Damage: Strained muscles (like the sternocleidomastoid) and sprained ligaments can cause pain and stiffness.
- Disc Injuries: Herniated or bulging discs may compress nerves, leading to radiating pain or numbness.
- Nerve Irritation: Compressed or stretched nerves can cause tingling, weakness, or sciatica-like symptoms.
- Facet Joint Injuries: These small joints in the spine can become inflamed or misaligned, contributing to chronic pain.
These injuries don’t always show up on standard X-rays, which is why advanced imaging is critical (more on that later). Left untreated, they can lead to chronic pain, reduced mobility, and even psychological issues like post-traumatic stress disorder (PTSD) (Jimenez, 2025a).
References
- National Highway Traffic Safety Administration. (2023). Traffic Safety Facts Annual Report. https://www.nhtsa.gov
- Physiopedia. (n.d.). Whiplash-associated disorders. https://www.physio-pedia.com/Whiplash_Associated_Disorders[](https://www.physio-pedia.com/Whiplash_Associated_Disorders)
- Jimenez, A. (2025a). PTSD: Essential insights on auto accidents and severe whiplash. El Paso Back Clinic. https://elpasobackclinic.com/ptsd-essential-insights-auto-accidents-severe-whiplash/[](https://elpasobackclinic.com/ptsd-essential-insights-on-auto-accidents-and-severe-whiplash/amp/)
How Whiplash-Associated Disorders Develop
WAD isn’t just a fancy term for a sore neck—it’s a spectrum of symptoms that can range from mildly annoying to downright debilitating. The Quebec Task Force classifies WAD into four grades based on severity:
- Grade 1: Neck pain, stiffness, or tenderness with no physical signs.
- Grade 2: Neck pain with musculoskeletal signs like decreased range of motion or tenderness.
- Grade 3: Neck pain with neurological symptoms (e.g., numbness, weakness, or tingling).
- Grade 4: Neck pain with fractures or dislocations (Physiopedia, n.d.).
The Pathophysiology of WAD
When your neck gets whipped around in an MVA, the damage isn’t always immediate. Microtears in muscles or ligaments can lead to inflammation, which irritates nearby nerves. This can cause a domino effect: inflammation leads to muscle spasms, which restrict movement, which causes more pain. It’s like your neck is throwing a tantrum and refusing to cooperate.
In some cases, the cervical spine’s facet joints or intervertebral discs take a hit. Disc herniations, for example, can press on nerve roots, causing radiculopathy (radiating pain) or even sciatica if the lower cervical nerves are involved (Jimenez, 2016). Studies show that whiplash can also alter the brain’s pain processing, leading to widespread sensory hypersensitivity in chronic cases (Sterling, 2004).
Delayed Symptoms: The Sneaky Side of WAD
Here’s the kicker: whiplash symptoms often play hide-and-seek. You might walk away from a fender-bender feeling fine, only to wake up the next day with a neck that feels like it’s been through a meat grinder. This delay is often due to adrenaline, which floods your system during a crash and masks pain. Other times, microtraumas compound over days or weeks, turning minor discomfort into a major problem (Jimenez, 2016).
Psychological Impact
WAD isn’t just physical—it can mess with your head, too. The trauma of an MVA can trigger PTSD, anxiety, or depression, especially if pain persists. Chronic pain and emotional stress feed off each other, creating a vicious cycle that’s harder to break than a bad habit (Jimenez, 2025a). In El Paso, where car accidents are all too common, addressing both the physical and mental aspects of WAD is crucial for recovery.
References
- Jimenez, A. (2016). Recovering from whiplash-associated disorders. El Paso Chiropractor Blog. https://www.elpasochiropractorblog.com/2016/08/recovering-from-whiplash-associated.html
- Physiopedia. (n.d.). Whiplash-associated disorders. https://www.physio-pedia.com/Whiplash_Associated_Disorders[](https://www.physio-pedia.com/Whiplash_Associated_Disorders)
- Sterling, M. (2004). A proposed new classification system for whiplash-associated disorders—implications for assessment and management. Manual Therapy, 9(2), 60-70. https://doi.org/10.1016/j.math.2004.01.006
- Jimenez, A. (2025a). PTSD: Essential insights on auto accidents and severe whiplash. El Paso Back Clinic. https://elpasobackclinic.com/ptsd-essential-insights-auto-accidents-severe-whiplash/[](https://elpasobackclinic.com/ptsd-essential-insights-on-auto-accidents-and-severe-whiplash/amp/)
The Science of Motion- Video
The Impact of Auto Injuries on the Cervical Spine and Neck
MVAs don’t just cause whiplash—they can unleash a whole parade of cervical spine injuries. Let’s break down the most common culprits and how they turn your neck into a grumpy old man who complains about everything.
Common Cervical Spine Injuries
- Whiplash: The poster child of MVA injuries, whiplash affects up to 80% of crash victims (Jimenez, 2025b). It’s like your neck decided to audition for a stunt double role without your permission.
- Herniated Discs: Trauma can cause discs to bulge or rupture, pressing on nerves and causing pain that radiates to the shoulders, arms, or hands (Jimenez, 2016).
- Spinal Misalignments (Subluxations): Vertebrae can shift out of place, disrupting nerve function and causing pain or stiffness.
- Fractures: High-impact crashes can crack vertebrae, especially in the cervical or thoracic spine. These are rare but serious (Jimenez, 2025c).
- Nerve Damage: Compressed or stretched nerves can lead to numbness, tingling, or weakness, sometimes mimicking sciatica (Jimenez, 2025b).
Long-Term Consequences
If left untreated, these injuries can lead to chronic pain, reduced mobility, and posture problems. Imagine trying to turn your head to check your blind spot but feeling like a rusty robot instead. Chronic WAD can also contribute to conditions like cervical spondylosis (arthritis of the neck) or fibromyalgia, making daily activities a chore (Sterling, 2006).
In El Paso, where over 5.2 million MVAs occur annually across the U.S., the need for expert care is huge (NHTSA, 2023). That’s where Dr. Alexander Jimenez shines, using his dual expertise as a chiropractor and nurse practitioner to tackle these injuries head-on.
References
- Jimenez, A. (2016). Recovering from whiplash-associated disorders. El Paso Chiropractor Blog. https://www.elpasochiropractorblog.com/2016/08/recovering-from-whiplash-associated.html
- Jimenez, A. (2025b). Integrative MVA recovery strategies for lasting health. Dr. Alex Jimenez. https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/[](https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/amp/)
- Jimenez, A. (2025c). Motor vehicle accident recovery and integrative care. Personal Injury Doctors. https://personalinjurydoctorgroup.com/motor-vehicle-accident-recovery-and-integrative-care/[](https://personalinjurydoctorgroup.com/2025/06/26/motor-vehicle-accident-recovery-and-integrative-care/amp/)
- National Highway Traffic Safety Administration. (2023). Traffic Safety Facts Annual Report. https://www.nhtsa.gov
- Sterling, M., et al. (2006). Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain, 122, 102-108. https://doi.org/10.1016/j.pain.2006.01.014
Treatments and Recovery Strategies for WAD and Cervical Spine Injuries
Good news: you don’t have to live with a neck that feels like it’s auditioning for a horror movie. With the right treatments, you can kick WAD and cervical spine injuries to the curb. Dr. Alexander Jimenez and his team at Injury Medical & Chiropractic Clinic in El Paso offer a holistic, integrative approach that’s like a superhero team-up for your recovery.
Chiropractic Care
Chiropractic adjustments are the bread and butter of WAD treatment. Dr. Jimenez uses targeted spinal manipulations to correct misalignments, reduce nerve compression, and restore joint mobility. It’s like giving your spine a gentle nudge to get back in line. Studies show that chiropractic care can significantly reduce pain and improve range of motion in WAD patients (Dunning et al., 2016).
- Manual Adjustments: These realign the cervical spine, relieving pressure on nerves and easing pain.
- Soft Tissue Mobilization: Techniques like massage or myofascial release reduce muscle tension and inflammation.
Physical Therapy
Physical therapy (PT) is like a personal trainer for your neck. Dr. Jimenez designs customized PT programs to strengthen neck muscles, improve flexibility, and prevent re-injury. Exercises like cervical rotations or isometric holds can work wonders (Jimenez, 2025d).
- Early Mobilization: Recent studies suggest that early, gentle movement is better than immobilization for WAD recovery (Rosenfeld et al., 2003).
- Functional Strength Training: This builds resilience in the neck and shoulders, reducing the risk of chronic pain.
Advanced Diagnostics
Dr. Jimenez doesn’t just guess what’s wrong—he uses cutting-edge tools to get the full picture. Advanced imaging like MRI, CT scans, or digital motion X-rays (DMX) can detect subtle injuries like ligament tears or disc herniations that standard X-rays miss. Electromyography (EMG) and functional movement screens assess nerve function, ensuring no injury goes unnoticed (Jimenez, 2025b).
Integrative Therapies
Dr. Jimenez’s dual-scope approach combines chiropractic care with nurse practitioner expertise, nutrition counseling, and therapies like acupuncture or transcutaneous electrical nerve stimulation (TENS). It’s like a buffet of healing options tailored to your needs.
- Acupuncture: Reduces pain and inflammation by stimulating specific points.
- Nutrition Counseling: Anti-inflammatory diets can support healing and reduce systemic inflammation.
- TENS Therapy: Delivers mild electrical pulses to block pain signals.
Recovery Timeline
Most people recover from WAD within a few weeks to months, but severe cases can take longer. Dr. Jimenez emphasizes early intervention to prevent chronicity. “Undetected microtraumas can compound over time,” he says. “Catching them early with advanced diagnostics is key” (Jimenez, 2025b). Regular reassessments ensure your treatment plan evolves with your progress.
References
- Dunning, J., et al. (2016). Effectiveness of thrust manipulation versus mobilization for neck pain. Journal of Manipulative and Physiological Therapeutics, 39(8), 551-561. https://doi.org/10.1016/j.jmpt.2016.08.002
- Jimenez, A. (2025b). Integrative MVA recovery strategies for lasting health. Dr. Alex Jimenez. https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/[](https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/amp/)
- Jimenez, A. (2025d). Post-car accident physical therapy approaches to recovery. Chiropractic Scientist. https://chiropracticscientist.com/post-car-accident-physical-therapy-approaches-to-recovery/[](https://chiropracticscientist.com/post-car-accident-physical-therapy-approaches-to-recovery/)
- Rosenfeld, M., et al. (2003). Early intervention in whiplash-associated disorders: A randomized clinical trial. Spine, 28(14), 1491-1498. https://doi.org/10.1097/01.BRS.0000076602.05659.4D
Dr. Alexander Jimenez: El Paso’s Personal Injury Hero
In El Paso, personal injury cases are a big deal. With millions of MVAs causing injuries each year, victims need more than just a pat on the back—they need expert care and legal support. Enter Dr. Alexander Jimenez, a board-certified chiropractor and family nurse practitioner with over 25 years of experience. His clinic, Injury Medical & Chiropractic Clinic, is a beacon of hope for accident victims.
Why Personal Injury Cases Matter
Personal injury cases often involve insurance claims or lawsuits to secure compensation for medical bills, lost wages, and pain and suffering. In El Paso, where car accidents are common, proving the link between an MVA and your injuries is critical. Dr. Jimenez excels at this, using his clinical expertise to produce detailed medical reports that hold up in court (Jimenez, 2025e).
Dr. Jimenez’s Unique Approach
Dr. Jimenez’s dual licensure as a chiropractor and nurse practitioner gives him a superpower: the ability to bridge biomechanical and systemic health. Here’s how he helps:
- Advanced Imaging: He uses MRI, CT, and DMX to detect injuries like ligament tears or disc herniations that might be missed otherwise. These objective findings validate claims and guide treatment (Jimenez, 2025b).
- Diagnostic Evaluations: EMG, nerve conduction studies, and functional movement screens provide a comprehensive picture of nerve and muscle function.
- Dual-Scope Procedures: Combining chiropractic adjustments with medical evaluations (e.g., metabolic or hormonal tests), Dr. Jimenez addresses both physical and physiological issues.
- Legal Documentation: His reports link injuries to the MVA with clinical and imaging evidence, making them gold for attorneys and insurance companies. He even provides expert testimony when needed (Jimenez, 2025e).
“Sometimes nerve involvement is missed in standard scans,” Dr. Jimenez explains. “That’s why we use advanced tools to track nerve conductivity and range of motion together” (Jimenez, 2025b). This meticulous approach ensures patients get the care and compensation they deserve.
A Liaison Between Medicine and Law
Dr. Jimenez acts as a translator between the medical and legal worlds. His ability to correlate injuries with objective findings makes him a trusted partner for personal injury attorneys. Whether it’s proving the extent of a whiplash injury or documenting chronic pain for a lawsuit, he’s got your back (and your neck).
References
- Jimenez, A. (2025b). Integrative MVA recovery strategies for lasting health. Dr. Alex Jimenez. https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/[](https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/amp/)
- Jimenez, A. (2025e). Personal injury chiropractic El Paso for accident recovery. EP Wellness & Functional Medicine Clinic. https://wellnessdoctorrx.com/personal-injury-chiropractic-el-paso-for-accident-recovery/[](https://wellnessdoctorrx.com/personal-injury-chiropractic-el-paso-for-accident-recovery/)
Preventing Further Damage to the Cervical Spine and Neck
Nobody wants their neck to feel like it’s stuck in a vice forever. Preventing further damage to the cervical spine and neck is all about proactive care and smart choices. Dr. Jimenez’s integrative approach ensures you’re not just treating symptoms but building a foundation for long-term health.
Early Intervention
The sooner you seek care, the better. Dr. Jimenez stresses that “undetected injuries can snowball into chronic conditions” (Jimenez, 2025b). Getting evaluated within 24-48 hours of an MVA can catch microtraumas before they become major issues.
Lifestyle Modifications
- Posture Control: Slouching is your neck’s worst enemy. Dr. Jimenez teaches patients how to maintain proper posture to reduce strain.
- Ergonomics: Adjust your car seat, desk, or computer to support your spine. Think of it as giving your neck a cozy hug.
- Exercise: Gentle neck stretches and strength exercises keep your cervical spine limber and strong.
Avoiding Re-Injury
- Safe Driving: Use headrests properly and avoid distractions to reduce the risk of another MVA.
- Gradual Return to Activity: Don’t jump back into heavy lifting or sports too soon. Follow Dr. Jimenez’s rehab plan to avoid setbacks.
- Stress Management: Chronic stress tightens neck muscles, worsening pain. Techniques like meditation or yoga can help.
Integrative Care
Dr. Jimenez’s clinic offers a one-stop shop for recovery. By combining chiropractic care, PT, acupuncture, and nutrition, he addresses the root causes of pain and prevents further damage. His “PUSH Functional Fitness System” is like CrossFit for your recovery, focusing on mobility, agility, and strength (Jimenez, 2025e).
References
- Jimenez, A. (2025b). Integrative MVA recovery strategies for lasting health. Dr. Alex Jimenez. https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/[](https://dralexjimenez.com/integrative-mva-recovery-strategies-for-lasting-health/amp/)
- Jimenez, A. (2025e). Personal injury chiropractic El Paso for accident recovery. EP Wellness & Functional Medicine Clinic. https://wellnessdoctorrx.com/personal-injury-chiropractic-el-paso-for-accident-recovery/[](https://wellnessdoctorrx.com/personal-injury-chiropractic-el-paso-for-accident-recovery/)
The Importance of Personal Injury Cases in El Paso
El Paso is no stranger to car accidents, and personal injury cases are a lifeline for victims. These cases ensure you’re not stuck footing the bill for someone else’s mistake. Dr. Jimenez’s expertise makes him a go-to practitioner for accident victims in the Borderland.
Why Personal Injury Cases Are Critical
- Financial Relief: Medical bills, lost wages, and rehab costs add up fast. Personal injury claims help cover these expenses.
- Justice: Holding negligent drivers accountable sends a message and promotes safer roads.
- Long-Term Care: Compensation can fund ongoing treatment for chronic injuries, ensuring you’re not left in pain.
Dr. Jimenez’s Role
Dr. Jimenez doesn’t just treat injuries—he builds a rock-solid case for you. His detailed reports, backed by advanced imaging and diagnostics, prove the link between your MVA and your injuries. This is crucial for insurance claims or lawsuits, especially when symptoms like pain or PTSD aren’t visible on standard tests (Jimenez, 2025a). His ability to provide expert testimony makes him a trusted ally in the courtroom.
El Paso’s Need for Expert Care
With over 2.2 million MVA injuries annually in the U.S., El Paso sees its fair share of victims (NHTSA, 2023). Dr. Jimenez’s clinic is a hub for integrative care, offering everything from chiropractic adjustments to legal coordination. His LinkedIn profile highlights his commitment to holistic healing and community service (Jimenez, 2023).
References
- Jimenez, A. (2023). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN. LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Jimenez, A. (2025a). PTSD: Essential insights on auto accidents and severe whiplash. El Paso Back Clinic. https://elpasobackclinic.com/ptsd-essential-insights-auto-accidents-severe-whiplash/[](https://elpasobackclinic.com/ptsd-essential-insights-on-auto-accidents-and-severe-whiplash/amp/)
- National Highway Traffic Safety Administration. (2023). Traffic Safety Facts Annual Report. https://www.nhtsa.gov
Conclusion
Whiplash-associated disorders and cervical spine injuries from motor vehicle accidents are serious conditions that require prompt, expert care. The cervical spine’s vulnerability to the violent forces of an MVA can lead to a range of injuries, from soft tissue strains to herniated discs and nerve damage. Left untreated, these can cause chronic pain, reduced mobility, and psychological distress. Dr. Alexander Jimenez, DC, APRN, FNP-BC, stands out as a leading practitioner in El Paso, offering integrative care that combines chiropractic adjustments, physical therapy, advanced diagnostics, and legal support. His dual-scope approach ensures comprehensive recovery while providing critical documentation for personal injury cases. Early intervention, personalized treatment plans, and lifestyle modifications are key to preventing long-term complications.
Disclaimer: This blog post is for informational purposes only and should not be taken as medical advice. Always consult a qualified healthcare provider, such as Dr. Alexander Jimenez, for diagnosis and treatment of whiplash-associated disorders or cervical spine injuries. The information provided is based on clinical insights and evidence-based practices, but is not a substitute for professional medical evaluation.