Beat TBIs and Body Toxicity with Chiropractic Care

Healing from Within: How Traumatic Brain Injuries Create Body Toxicity and Integrative Care Supports Adult Recovery
Traumatic brain injuries, also known as TBIs, can abruptly alter a person’s life. For many adults, these injuries occur during a car crash on the way to work, a vicious hit in a weekend soccer game, or a fall at a construction site. These injuries do more than bruise the skull—they start a chain reaction of harm inside the body. This process creates a kind of “toxicity” that spreads from the brain to other organs, making recovery tough. But there’s hope. An integrative care approach, led by experts such as chiropractic nurse practitioners (CNPs), considers the whole person. It helps calm the body’s chaos, eases pain naturally, and builds strength for the long haul. Families and care teams also play a crucial role, providing emotional support and daily assistance. In this article, we’ll break down how TBIs cause this inner poison, why it matters for adults, and how team-based care can turn things around.
Imagine a 35-year-old office worker named Mark. He’s rear-ended in traffic, his head snaps back, and everything goes black for a moment. At first, it’s headaches and dizziness. Weeks later, gut issues and mood swings hit hard. The hidden side of TBI involves biochemical events that intensify over time. Research shows these effects can last weeks or years, raising risks for bigger problems like memory loss or even diseases like Alzheimer’s (Priester, 2025). But early, whole-body care changes the story. CNPs combine chiropractic adjustments with nursing expertise to reset the nervous system and combat inflammation. They guide adults like Mark back to work, play, and family life. This isn’t just medicine; it’s a roadmap for healing that honors the body’s own power.
For families, it’s personal. Spouses learn to spot warning signs, like when fatigue turns to frustration. Care teams coordinate visits, meals, and therapy sessions to ensure seamless care. Together, they tackle the toxicity head-on. As one study notes, addressing both the brain and body early can prevent long-term damage (Rauchman et al., 2023). Let’s dive into the science, simply explained, and see how recovery works in real life.
Understanding Traumatic Brain Injuries in Everyday Adult Life
Adults face TBIs more often than we think. In the U.S., over 2.8 million people seek emergency care each year, with motor vehicle accidents (MVAs) accounting for about 28%, falls at work for 20%, and sports-related injuries, such as those from football or boxing, making up another significant portion (Rauchman et al., 2023). A busy parent or factory worker can be out of work for months after a small slip or crash. Unlike children, adults often juggle jobs, bills, and family responsibilities, so recovery hits harder—lost wages, strained relationships, and endless doctor’s wait times.
A TBI starts with the primary injury: the direct hit. In an MVA, the brain slams against the skull, tearing blood vessels and nerves. Sports concussions come from rotational forces, twisting the brain like a wet towel. Workplace incidents, like dropping tools on the head, add blunt force. Right away, symptoms appear: confusion, nausea, and blurred vision. However, the real danger lies in the seconds that follow—the brain swells, pressure builds, and oxygen levels drop (Salehi et al., 2017).
Take Sarah, a 42-year-old soccer coach. A header in a pickup game leaves her with a mild concussion. She pushes through practices, but soon battles insomnia and irritability. Her family notices she’s “off.” This is common; mild TBIs affect 80% of cases, yet many adults ignore them, thinking it’s just a bump (Laskowitz & Grant, 2016). Men in their 30s and 40s, often in high-risk jobs or sports, make up the bulk. Women post-childbirth or in caregiving roles face extra stress, slowing healing.
Why does this matter? TBIs don’t stay in the head. They spark a body-wide alarm, releasing stress hormones that tax the heart and gut. Without quick care, simple tasks like driving become scary. But spotting it early helps. Doctors use CT scans for severe cases, but for mild ones, it’s a history and physical examination. Families step in here—tracking symptoms in a journal, urging rest. Workplaces can adapt with flexible hours or ergonomic fixes.
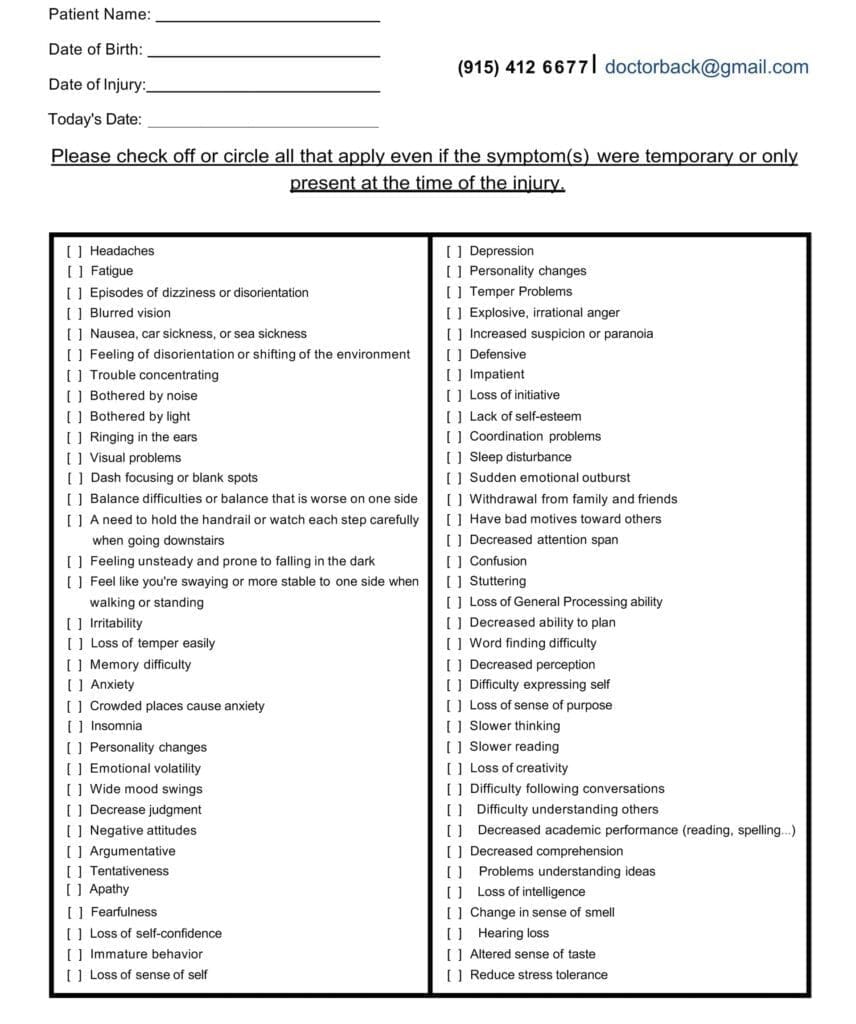
Symptom Questionnaire:
The positive news is that there are solutions available. Most adults recover well with support. One review found that 70% of patients return to normal within three months if treated holistically (Schimmel et al., 2017). That means blending rest, therapy, and family encouragement. For Mark from the intro, his wife joined therapy sessions, learning cues to de-escalate his frustration. It’s not just survival; it’s reclaiming life.
The Toxic Cascade: How TBIs Poison the Brain and Body
A TBI isn’t a one-and-done event. The initial impact, known as the primary injury, initiates a cascade of biochemical complications. This “cascade” turns the brain into a toxic zone, harming cells and spreading chaos to the gut, blood, and beyond. It’s like a fire that starts small but burns hot if unchecked. Understanding this helps adults and their teams fight back smarter.
Firstly, consider the initial impact. In an MVA, rapid deceleration shears axons—the brain’s wiring—like pulling threads from fabric. Sports-related impacts stretch tissue, while falling objects from work crush it. This releases danger signals, known as damage-associated molecular patterns (DAMPs), which alert the immune system (McKee & Lukens, 2016). Blood vessels break, starving cells of oxygen. Swelling, or edema, follows fast. There are two main types: cytotoxic, where cells suck up water like sponges due to pump failures, and vasogenic, where the blood-brain barrier (BBB) leaks like a busted dam, flooding tissue with proteins and fluid (Salehi et al., 2017). In adults, this raises skull pressure, squeezing the brain and risking more death. One study in mice showed edema peaking days after impact, mirroring human cases (Priester, 2025).
Now, the secondary storm—the real toxicity builder. It unfolds in phases: minutes, hours, days. Enter excitotoxicity. Damaged neurons release glutamate, the brain’s “go” signal, into the space. Normally, this excites cells briefly. However, in traumatic brain injury (TBI), it triggers a massive surge of glutamate. Glutamate overworks receptors, letting calcium rush in like floodwater. This calcium revs up destructive enzymes, which rip membranes and shred DNA. Cells swell, burst, and die in a chain reaction (Waters, n.d.). It’s why symptoms like seizures or coma are delayed. In car crashes, this “glutamate storm” spreads from impact zones, killing healthy neighbors (Rauchman et al., 2023). Adults in high-stress jobs often experience chronic fatigue, as their brains remain in overdrive.
Next, oxidative stress amps up the damage. The brain guzzles oxygen but has weak defenses. TBI sparks reactive oxygen species (ROS)—unstable molecules like superoxide or hydroxyl radicals—from busted mitochondria and fired-up immune cells. These ROS (reactive oxygen species) chew lipids in cell walls, creating toxic byproducts like 4-hydroxynonenal, which poison proteins and genes (Fesharaki-Zadeh, 2022). Iron from burst blood vessels fuels this process via Fenton reactions, generating more radicals. In sports concussions, repeated hits build ROS over time, explaining why pros face early Parkinson’s risks (Wu et al., 2022). One mouse study found that ROS stayed around for weeks after the infection, changing proteins and DNA in ways that are similar to the long-term symptoms of adults with persistent cognitive impairment (Priester, 2025).
Neuroinflammation piles on. Microglia, the brain’s guards, wake up and call in troops: monocytes via CCR2 signals and neutrophils, which release cytokines such as TNF-α and IL-1β (McKee & Lukens, 2016). This “fire” initially clears debris, but it then veers off course and attacks healthy tissue. In work injuries, chronic low-grade inflammation lingers, turning acute pain into a daily ache. Microglia also accumulate amyloid proteins, which serve as seeds for plaques in Alzheimer’s disease (Denniss & Barker, 2023). Cytokines breach the BBB, worsening leaks and edema. Adults report mood dips here—irritability from inflamed pathways mimicking depression.
Keep in mind the disruption of the gut-brain axis. The vagus nerve and microbes facilitate communication between the brain and gut. TBI shocks this link, slowing gut motility and poking holes in the intestinal wall—”leaky gut” (Faden et al., 2021). Bacteria enter the bloodstream, triggering sepsis or a body-wide inflammatory response. In MVAs, stress hormones like cortisol halt digestion, causing ulcers or symptoms similar to IBS (Heuer Fischer, P.A., n.d.). One study linked TBI-induced gut changes to worse brain swelling, as toxins circulate back via the blood (Cannon et al., 2023). For a construction worker, a post-fall condition means nausea on top of headaches, which can delay their return to the site.
These events interconnect: excitotoxicity generates ROS; inflammation widens the BBB cracks; gut leaks fuel the fire. The BBB, that tight shield of endothelial cells and astrocyte feet, frays from the action of matrix metalloproteinases (MMPs) and VEGF surges, allowing toxins to enter (Laskowitz & Grant, 2016a). Edema follows, compressing vessels and depriving cells of oxygen. In adults, this cascade hits harder—aging brains have less reserve, per one review (Salehi et al., 2017). However, is it possible to detect it at an early stage? Antioxidants, such as those in a new polymer, reduce ROS by 50% in mice, suggesting potential benefits in humans (Priester, 2025).
This toxicity isn’t abstract. For Sarah, the coach, it meant experiencing gut cramps and sidelining drills. Mark’s family adjusted meals to ease inflammation. Knowing the cascade empowers choice—enabling rest, consuming anti-inflammatory foods, and receiving targeted care. It’s the body’s cry for balance, and integrative pros listen.
Long-Term Risks: From Acute Toxicity to Lasting Brain Changes
If unchecked, TBI’s toxic wave doesn’t fade—it reshapes the brain. Weeks after the hit, waste like tau proteins piles up because the glymphatic system, the brain’s drain, clogs (Plog & Nedergaard, 2018). This mirrors the aging process or Alzheimer’s, where toxins spread, forming plaques. In adults, repeated sports hits can cause chronic traumatic encephalopathy (CTE)—mood swings, aggression, and dementia decades later (Priester, 2025).
Oxidative scars mutate genes; inflammation scars tissue with glial walls, blocking repair (Denniss & Barker, 2023). Gut leaks let endotoxins fuel chronic fatigue. One study tied early BBB breaks to poor outcomes years on (Laskowitz & Grant, 2016a). For work-hardened adults, this means early retirement and family strain. But mitigation works—lifestyle tweaks cut risks by 30% (Schimmel et al., 2017). It’s a wake-up: Act now, or pay later.
An Integrative Path to Recovery: The Role of Chiropractic Nurse Practitioners
Integrative care challenges the conventional understanding of TBI toxicity. It’s not just pills or scalpels—it’s a team that weaves chiropractic, nursing, nutrition, and therapy into one comprehensive plan. At the heart? Chiropractic nurse practitioners (CNPs). Trained in both fields, they identify spine-brain connections, adjust misalignments, and promote holistic healing. For adults post-MVA or concussion, this means less toxicity and more resilience.
Why chiropractic? The spine houses the nervous system; it conveys, constricts, and conveys signals. Adjustments realign the vertebrae, easing nerve pressure and resetting the “fight-or-flight” mode to a calm state (Sea Change Wellness Chiropractic, n.d.). One clinic notes it boosts cerebrospinal fluid (CSF) flow, the brain’s bath that clears toxins (Apex Chiropractic, n.d.). In workplace falls, this reduces headaches by 60%, according to patient reports (Northwest Florida Physicians Group, LLC, n.d.). CNPs add nursing layers by monitoring vitals, adjusting medications, and teaching self-care.
Dr. Alexander Jimenez, DC, APRN, FNP-BC, embodies this. At his El Paso clinic, he treats auto accident victims with spinal decompression and functional nutrition, targeting root causes like inflammation (Jimenez, n.d.a). “We restore normal functions after injuries without drugs,” he says, blending adjustments with omega-3s to douse ROS (Jimenez, n.d.b). His cases? A truck driver post-crash regained focus via neuropathy protocols; a golfer shook sports fog with vagus nerve stim via adjustments. Over 30 years, he’s seen integrative plans slash recovery time, empowering adults to ditch painkillers.
This approach hits all cascades. For excitotoxicity, gentle cranial work calms glutamate storms (Dr. Kal, n.d.). Oxidative stress? CNPs promote the uptake of antioxidants—such as berries and vitamin E—to neutralize ROS, a finding supported by mouse studies (Wu et al., 2022). Neuroinflammation can be alleviated with posture adjustments, thereby reducing cytokine triggers (Serenity Healthcare Partners, n.d.). Gut-brain? Probiotics and vagus-focused breathing mend leaks (Faden et al., 2021). BBB heals via better circulation from alignments.
Integrated therapies shine. Physical therapy helps rebuild balance, while CBT tames anxiety (Peixoto et al., 2025). Nutrition—anti-inflammatory diets—fuels repair (Serenity Healthcare Partners, n.d.). Emerging technologies, such as EMF stimulation in swine models, restore brain waves, hinting at potential human applications (Brazdzionis et al., 2023). CNPs coordinate, personalizing for a 50-year-old welder’s shifts or a mom’s school runs.
For Mark, CNP-led sessions mixed adjustments with family nutrition classes. Sarah added yoga for gut calm. Results? Sarah experienced faster clarity and fewer trips to the emergency room. Dr. Jimenez’s webinars stress this: “Functional medicine reverses imbalances—oxidative stress, gut dysbiosis—for true recovery” (Jimenez, n.d.b). It’s empowering, natural, and effective.
Supporting the Journey: Families and Care Teams in Adult TBI Recovery
Recovery isn’t solo. Families and care teams are the glue, turning plans into action. Spouses track moods, spotting toxicity flares like irritability from inflammation. Kids adapt games for dad’s fatigue; siblings share chores. This buffer cuts depression risks by 40% (Peixoto et al., 2025).
Care teams—CNPs, therapists, and docs—huddle weekly, adjusting for work stress or sports urges. Families attend education sessions to learn about edema signs or gut-friendly meal options. One family’s story: Post-concussion, they mapped “rest zones” at home, easing Mark’s load. Emotional tools, such as support groups, build resilience. As Dr. Jimenez notes, “Holistic care includes mind and spirit—families amplify healing” (Jimenez, n.d.a). It’s a shared victory.
Conclusion: Reclaiming Life After the Storm
TBIs from crashes, games, or jobs unleash a toxic cascade—excitotoxicity flooding cells, ROS scorching tissues, inflammation raging, and gut links breaking. For adults, it’s a body-wide battle, but integrative care, spearheaded by CNPs, counters it. Adjustments reset nerves, nutrition quells fires, and teams sustain hope. With families involved, recovery isn’t just possible—it’s transformative. As research evolves, from antioxidants to EMF, the path brightens. Adults like Mark and Sarah prove: Healing starts within but thrives together. Seek care early; your future self will thank you.
References
Apex Chiropractic. (n.d.). How chiropractic care can treat a traumatic brain injury. https://apexchiroco.com/updates/how-chiropractic-care-can-treat-a-traumatic-brain-injury/
Brazdzionis, J., Radwan, M. M., Thankam, F., Lal, M. R., Baron, D., Connett, D. A., Agrawal, D. K., & Miulli, D. E. (2023). A swine model of traumatic brain injury: Effects of neuronally generated electromagnetic fields and electromagnetic field stimulation on traumatic brain injury-related changes. Cureus, 15(11), e48992. https://doi.org/10.7759/cureus.48992
Cannon, A. R., Anderson, L. J., Galicia, K., Murray, M. G., Kamran, A. S., Li, X., Gonzalez, R. P., & Choudhry, M. A. (2023). Traumatic brain injury induced inflammation and GI motility dysfunction. Brain Sciences, 13(3), 414. https://doi.org/10.3390/brainsci13030414
Denniss, R. J., & Barker, L. A. (2023). Brain trauma and the secondary cascade in humans: Review of the potential role of vitamins in reparative processes and functional outcome. Neuropsychiatric Disease and Treatment, 19, 1693–1707. https://doi.org/10.2147/NDT.S415943
Dr. Kal. (n.d.). Chiropractic relief for accident head injuries. https://drkal.com/chiropractic-relief-for-accident-head-injuries/
Faden, A. I., Barrett, J. P., Stoica, B. A., & Henry, R. J. (2021). Bi-directional brain-systemic interactions and outcomes after TBI. Trends in Neurosciences, 44(5), 406–418. https://doi.org/10.1016/j.tins.2020.12.004
Fesharaki-Zadeh, A. (2022). Oxidative stress in traumatic brain injury. International Journal of Molecular Sciences, 23(21), 13000. https://doi.org/10.3390/ijms232113000
Heuer Fischer, P.A. (n.d.). TBI and gut health. https://www.heuerfischer.com/firm-overview/blog/tbi-and-gut-health/
Jimenez, A. (n.d.a.). Injury specialists. https://dralexjimenez.com/
Jimenez, A. (n.d.b.). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛ – Injury Medical Clinic PA. https://www.linkedin.com/in/dralexjimenez/
Laskowitz, D., & Grant, G. (Eds.). (2016a). Blood–brain barrier pathophysiology following traumatic brain injury. In Translational research in traumatic brain injury. CRC Press/Taylor & Francis Group. https://www.ncbi.nlm.nih.gov/books/NBK326726/
Laskowitz, D., & Grant, G. (Eds.). (2016b). Neuroplasticity after traumatic brain injury. In Translational research in traumatic brain injury. CRC Press/Taylor & Francis Group. https://www.ncbi.nlm.nih.gov/books/NBK326735/
McKee, C. A., & Lukens, J. R. (2016). Emerging roles for the immune system in traumatic brain injury. Frontiers in Immunology, 7, 556. https://doi.org/10.3389/fimmu.2016.00556
Northwest Florida Physicians Group, LLC. (n.d.). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries/
Peixoto, B., Cruz, M., & Ustares, V. (2025). Traumatic brain injury and neuropsychiatric consequences. Current Psychiatry Reports, 27(1), 1–12. https://doi.org/10.1007/s11920-024-01523-4
Plog, B. A., & Nedergaard, M. (2018). The glymphatic system in CNS health and disease. Neuron, 98(6), 1095–1118. (From rehabpub.com summary)
Priester, A. (2025, February 13). Traumatic brain injuries have toxic effects that last weeks after initial impact − an antioxidant material reduces this damage in mice. The Conversation. https://theconversation.com/traumatic-brain-injuries-have-toxic-effects-that-last-weeks-after-initial-impact-an-antioxidant-material-reduces-this-damage-in-mice-247655
Rauchman, S. H., Zubair, A., Jacob, B., Rauchman, D., Pinkhasov, A., & Placantonakis, D. G. (2023). Traumatic brain injury: Mechanisms, manifestations, and visual sequelae. Frontiers in Neuroscience, 17, 1090672. https://doi.org/10.3389/fnins.2023.1090672
Salehi, A., Zhang, J. H., & Obenaus, A. (2017). Response of the cerebral vasculature following traumatic brain injury. Journal of Cerebral Blood Flow & Metabolism, 37(10), 2320–2339. https://doi.org/10.1177/0271678X17701660
Schimmel, S. J., Acosta, S., & Lozano, D. (2017). Neuroinflammation in traumatic brain injury: A chronic response to an acute injury. Journal of Neurotrauma, 34(13), 2139–2147. https://doi.org/10.1089/neu.2016.4648
Sea Change Wellness Chiropractic. (n.d.). How chiropractic helps reset the nervous system after car crash trauma. https://seachangechiropractic.com/how-chiropractic-helps-reset-the-nervous-system-after-car-crash-trauma/
Serenity Healthcare Partners. (n.d.). How integrated therapies enhance recovery from traumatic brain injuries. https://www.serenityhealthcarepartners.com/how-integrated-therapies-enhance-recovery-from-traumatic-brain-injuries/
Waters, C. (n.d.). Excitotoxicity: A secondary injury in traumatic brain damage. https://www.charliewaterslaw.com/brain-injury/excitotoxicity-a-secondary-injury-in-traumatic-brain-damage/
Wu, A.-G., Yong, Y.-Y., Pan, Y.-R., Zhang, L., Wu, J.-M., Zhang, Y., Tang, Y., Wei, J., Yu, L., Law, B. Y.-K., Yu, C.-L., Liu, J., Lan, C., Xu, R.-X., Zhou, X.-G., & Qin, D.-L. (2022). Targeting Nrf2-mediated oxidative stress response in traumatic brain injury: Therapeutic perspectives of phytochemicals. International Journal of Molecular Sciences, 23(7), 3771. https://doi.org/10.3390/ijms23073771
Post Disclaimer
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Beat TBIs and Body Toxicity with Chiropractic Care" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and facilitate clinical collaboration with specialists across disciplines. Each specialist is governed by their professional scope of practice and licensure jurisdiction. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRN: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card

