The “Reset” Pain After Holding an Awkward Position

What It’s Called, Why It Happens, and How ChiroMed Integrative Care Can Help
Have you ever sat, stood, or twisted in a position that felt “fine” at first, but when you moved back to normal, you felt a sharp discomfort, stiffness, or a strange “reset” sensation in a muscle or joint? Sometimes it feels like something releases, and then you need a minute for the area to calm down.
This is a very common body experience. Most of the time, it is not mysterious. It is your nervous system and soft tissues reacting to being held in a stressful position and then quickly returning to neutral.
Clinically, this experience is usually explained by a combination of:
- Postural strain (overload from posture)
- Muscle tightness and muscle guarding (protective tension)
- Trigger points (sensitive, tight spots in muscle)
- Myofascial restriction (stiffer, less mobile fascia)
- Temporary joint restriction (a joint not gliding normally)
At ChiroMed, this is often approached as a “whole system” issue: joints, muscles, fascia, and the nervous system all influence how you move and how you feel, especially after long periods of sitting, working, driving, or sleeping in a poor position (ChiroMed, n.d.-a; Mayo Clinic, 2024). https://chiromed.com/ ; https://www.mayoclinic.org/tests-procedures/chiropractic-adjustment/about/pac-20393513
What is this feeling called?
People describe it in different ways:
- “My back locked up”
- “My neck was stuck and then it popped”
- “I moved and it had to reset”
- “It felt like a cramp, then it let go”
- “It hurts when I come back to normal”
From a clinical point of view, the most accurate labels usually include:
- Postural strain
- Muscle guarding (protective stiffness)
- Trigger point flare (myofascial pain)
- Joint restriction or joint dysfunction (reduced joint motion)
- Myofascial restriction (fascia not gliding well)
You may also hear chiropractic terms like “restricted segmental motion” or “functional joint restriction.” Some people use the word “subluxation” to describe a motion problem, but in most everyday posture cases, the key issue is not a dislocation. It is a temporary movement limitation and soft-tissue tightness that causes pain when you return to neutral (Mayo Clinic, 2024). https://www.mayoclinic.org/tests-procedures/chiropractic-adjustment/about/pac-20393513
Why it happens: the simple explanation
Your body is built for variety in movement. When you stay in one awkward position too long, your body adapts to protect you. That protection can feel like tightness, stiffness, and pain when you move back.
A practical way to think about it:
- You hold a stressful posture.
- Some tissues get compressed and irritated.
- Muscles tighten to stabilize you (guarding).
- Fascia becomes less “slippery” and more stiff.
- A joint may stop gliding normally.
- When you return to neutral, everything has to “reorganize” fast.
- You feel a “reset” sensation, along with short-term discomfort.
Fascia matters here because it is a connective tissue network that surrounds muscles and helps them glide. When fascia gets irritated or less mobile, it can feel like tightness, pulling, or stiffness (Johns Hopkins Medicine, n.d.). https://www.hopkinsmedicine.org/health/wellness-and-prevention/muscle-pain-it-may-actually-be-your-fascia
The key parts of the “reset” experience
Tight muscles or protective guarding
Muscle guarding is your nervous system trying to prevent movement it perceives as unsafe. It can happen after:
- Long sitting
- Repetitive work
- Stress and poor sleep
- Minor strains
- Old injuries that make you move differently
Muscle stiffness and soreness after inactivity are common symptoms and can improve as tissues warm up and circulation increases (Cleveland Clinic, 2023). https://my.clevelandclinic.org/health/symptoms/25147-muscle-stiffness
Trigger points
Trigger points are sensitive, tight spots inside a muscle. When you change position, the muscle length changes, and the trigger point can “complain.”
Common clues you are dealing with trigger points:
- A tender spot that hurts when pressed
- A tight band feeling in the muscle
- Pain that can refer to nearby areas
Myofascial pain patterns like this are widely described in patient education and often respond best to a mix of movement, soft-tissue care, and addressing the underlying cause (WebMD, 2024a). https://www.webmd.com/pain-management/myofascial-pain-syndrome
Fascia restriction and “sticky” glide
Fascia is not just wrapping. It has nerves, it responds to stress and movement, and it can contribute to pain when irritated (Johns Hopkins Medicine, n.d.). https://www.hopkinsmedicine.org/health/wellness-and-prevention/muscle-pain-it-may-actually-be-your-fascia
When fascia is restricted, you may notice:
- You feel stiff even when you stretch
- The area feels “stuck” more than “tight”
- You feel pulling or discomfort with certain angles
Stretching alone does not always resolve stiffness, according to some rehab sources. Often, you need mobility, strength, and better movement patterns (NYDN Rehab, 2019). https://nydnrehab.com/blog/feeling-stiff-why-stretching-may-not-be-the-best-solution/
Joint restriction and the “pop”
If a joint has not been moving normally, it can feel like it “catches” or pinches at the end range. When it finally moves again (whether naturally or through an adjustment), some people feel a release or hear a pop.
Patient education materials commonly explain that a pop can involve a pressure change and gas release in the joint (often called cavitation) (Spine Stop, 2025; Peak Performance, n.d.).
https://www.spinestop.com/blog/what-happens-during-a-chiropractic-adjustment
https://peakperformancefranklin.com/faq/
What is happening inside your body when you move back to neutral?
Joint fixation or motion loss
A joint that does not glide well can create:
- Pain when you “push it” back to neutral
- A sudden release sensation when it finally moves
- Short-term soreness after movement returns
Proprioceptive “reset”
Proprioception is your body’s sense of position. When you stay in a posture too long, your nervous system may temporarily treat it as the new normal. When you return to neutral, the brain and muscles recalibrate. That recalibration can feel weird, stiff, or briefly painful, then it settles.
Short-term soreness afterward
After a release, you may feel:
- A warm ache
- Mild soreness
- Less restriction, but tenderness for a few hours
This can be normal, especially if the tissues were irritated and are now moving again (Health.com, 2023; Mayo Clinic, 2024).
https://www.health.com/chiropractor-7554177
https://www.mayoclinic.org/tests-procedures/chiropractic-adjustment/about/pac-20393513
Why posture is often the root driver
Poor posture is not about looking a certain way. It is about how the load is distributed over time.
When posture is off for long periods, it can lead to:
- Muscle strain and overuse in some areas
- Weakness or underuse in other areas
- Joint stress and reduced motion
- Higher chance of recurring tightness
Several clinics and rehab resources discuss poor posture as a common contributor to tension and discomfort (Calhoun Spine Care, n.d.; Blackburn Chiropractic Clinic, n.d.; Physis Rehab, n.d.).
https://calhounspinecare.com/postures-impact-on-back-pain-treatment-success-3/
https://blackburnchiropractor.ca/conditions/postural-alterations/
https://www.physisrehab.com/poor-posture-the-main-culprit-behind-muscle-tension/
What about “somatic soreness” and stress-based tension?
Sometimes the “locked” feeling is not only mechanical. Stress can raise baseline muscle tension and make your nervous system more protective.
Some writers use the term “somatic soreness” to describe body tension that can be influenced by emotional stress and nervous system activation (On The Go Wellness, n.d.). https://onthegowellness.com/somatic-soreness-the-overlooked-difference-between-muscle-pain-and-emotional-tension-stored-in-the-body/
This does not mean the pain is imaginary. It means your system may be:
- More sensitive to pressure and movement
- More likely to guard and brace
- Slower to relax after strain
An integrative plan can still help because it targets both motion and nervous system calm.
How ChiroMed’s integrative approach can help
ChiroMed presents itself as an integrative clinic that combines chiropractic care with services such as nurse practitioner care, rehabilitation, nutrition, and acupuncture, aiming for a coordinated plan rather than a one-tool approach (ChiroMed, n.d.-a; ChiroMed, n.d.-b).
https://chiromed.com/
https://chiromed.com/about-us/
When you keep getting the “reset pain,” a useful plan typically includes four pillars:
Restore joint motion (adjustment or mobilization)
Chiropractic adjustment is commonly described as a controlled force applied to improve spinal or joint motion and reduce pain in certain conditions, such as neck or back pain (Mayo Clinic, 2024). https://www.mayoclinic.org/tests-procedures/chiropractic-adjustment/about/pac-20393513
Why it can help with the “reset” pattern:
- It helps a restricted joint move more normally
- It reduces the need for your body to “force” a painful release on its own
- It may decrease protective muscle guarding once motion feels safer
Address soft tissue and fascia (myofascial work)
If your pain is driven by trigger points or fascial restriction, soft tissue methods may be important:
- Myofascial release
- Trigger point techniques
- Gentle stretching paired with movement retraining
Myofascial pain education commonly includes these approaches, alongside exercise, posture, and repetitive strain management (WebMD, 2024a; WebMD, 2024b).
https://www.webmd.com/pain-management/myofascial-pain-syndrome
https://www.webmd.com/pain-management/what-to-know-myofascial-release-therapy
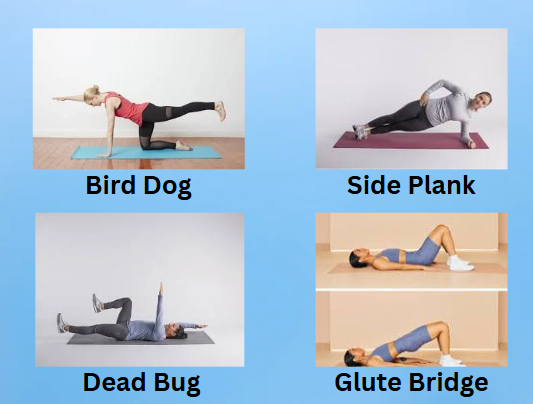
Rehab and exercise, so it does not keep coming back
If a joint keeps getting “stuck,” there is usually a reason:
- Weak stabilizers
- Poor motor control
- Limited mobility in a nearby area
- Repetitive posture habits
Rehab that combines mobility and strength often creates longer-lasting change than stretching alone (NYDN Rehab, 2019). https://nydnrehab.com/blog/feeling-stiff-why-stretching-may-not-be-the-best-solution/
Calm the nervous system (reduce guarding)
When pain decreases and movement feels safer, guarding can ease.
Supportive factors include:
- Better sleep
- Breath work
- Gentle daily movement
- A plan that progresses gradually (not too aggressive)
ChiroMed’s integrative model emphasizes multidisciplinary support and collaboration when needed (ChiroMed, n.d.-c). https://chiromed.com/elpaso-texas/
Clinical observations: Dr. Alexander Jimenez, DC, APRN, FNP-BC
ChiroMed’s website states it is led by Dr. Alex Jimenez and highlights a multidisciplinary approach that blends chiropractic care with nurse practitioner-level evaluation and integrative wellness strategies (ChiroMed, n.d.-d). https://chiromed.com/contact-us/
From an integrative clinical perspective, the “reset pain” pattern is often treated more effectively when the plan includes:
- A movement and posture assessment
- Joint mechanics plus soft tissue evaluation
- Progressive rehab to build stability
- Attention to nervous system load (stress, sleep, recovery)
This “full picture” approach is also consistent with how Dr. Jimenez presents integrative care across his professional platforms (ChiroMed, n.d.-d). https://chiromed.com/contact-us/
What you can do today: quick steps that reduce the “reset” problem
You do not have to wait until it is severe.
Movement habits that help
- Change positions every 30 to 60 minutes
- Take “movement snacks” during the day:
- 30 seconds of standing and walking
- gentle shoulder rolls
- easy neck turns (pain-free range)
- hip shifts or mini-squats
A simple 2-minute reset routine
- 5 slow breaths (longer exhale)
- 10 shoulder blade squeezes
- 10 gentle hip hinges or sit-to-stands
- 30 to 60 seconds of walking
Posture upgrades that matter
- Screen at eye level
- Feet supported
- Hips and knees comfortable (not tucked under)
- Avoid one-sided leaning for long periods
When you should get evaluated
Get checked sooner if you have:
- Numbness or tingling that is new or worsening
- Weakness in an arm or leg
- Severe pain after an accident or fall
- Fever, unexplained weight loss, or night pain
- Bowel or bladder changes
For severe, persistent, or unimproving back pain, patient guidance commonly recommends seeking evaluation from a qualified professional (Healthgrades, 2020). https://resources.healthgrades.com/right-care/back-pain/when-to-see-a-doctor-for-back-pain
Bottom line
The “reset” pain after holding an awkward position is usually a mix of:
- Postural strain
- Muscle guarding
- Trigger points
- Fascial restriction
- Temporary joint restriction
- A nervous system recalibrating proprioception
An integrative plan can help by restoring motion, treating soft-tissue restrictions, strengthening weak links, and reducing the nervous system’s need to guard. ChiroMed describes a multidisciplinary model that combines these strategies into a single coordinated plan (ChiroMed, n.d.-a; ChiroMed, n.d.-b).
https://chiromed.com/
https://chiromed.com/about-us/
References
- ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX (ChiroMed, n.d.-a). https://chiromed.com/
- About Us (ChiroMed, n.d.-b). https://chiromed.com/about-us/
- El Paso (ChiroMed, n.d.-c). https://chiromed.com/elpaso-texas/
- Contact Us (ChiroMed, n.d.-d). https://chiromed.com/contact-us/
- Chiropractic adjustment (Mayo Clinic, 2024). https://www.mayoclinic.org/tests-procedures/chiropractic-adjustment/about/pac-20393513
- Muscle pain: It may actually be your fascia (Johns Hopkins Medicine, n.d.). https://www.hopkinsmedicine.org/health/wellness-and-prevention/muscle-pain-it-may-actually-be-your-fascia
- Muscle stiffness: Causes and treatment (Cleveland Clinic, 2023). https://my.clevelandclinic.org/health/symptoms/25147-muscle-stiffness
- Myofascial pain syndrome (WebMD, 2024a). https://www.webmd.com/pain-management/myofascial-pain-syndrome
- What to know about myofascial release therapy (WebMD, 2024b). https://www.webmd.com/pain-management/what-to-know-myofascial-release-therapy
- Feeling stiff? Why stretching may not be the best solution (NYDN Rehab, 2019). https://nydnrehab.com/blog/feeling-stiff-why-stretching-may-not-be-the-best-solution/
- Posture’s impact on back pain treatment success (Calhoun Spine Care, n.d.). https://calhounspinecare.com/postures-impact-on-back-pain-treatment-success-3/
- Postural alterations (Blackburn Chiropractic Clinic, n.d.). https://blackburnchiropractor.ca/conditions/postural-alterations/
- Poor posture: The main culprit behind muscle tension (Physis Rehab, n.d.). https://www.physisrehab.com/poor-posture-the-main-culprit-behind-muscle-tension/
- Somatic soreness (On The Go Wellness, n.d.). https://onthegowellness.com/somatic-soreness-the-overlooked-difference-between-muscle-pain-and-emotional-tension-stored-in-the-body/
- What happens during a chiropractic adjustment? (Spine Stop, 2025). https://www.spinestop.com/blog/what-happens-during-a-chiropractic-adjustment
- FAQ (Peak Performance, n.d.). https://peakperformancefranklin.com/faq/
- When to see a doctor for back pain (Healthgrades, 2020). https://resources.healthgrades.com/right-care/back-pain/when-to-see-a-doctor-for-back-pain
- What you can expect from a chiropractic visit (Health.com, 2023). https://www.health.com/chiropractor-7554177