Gut Neuropathies: Holistic Healing at ChiroMed El Paso

Gut Neuropathies: Holistic Healing Through Integrated Medicine
Gut neuropathies, including enteric and autonomic neuropathies, occur when the nerves controlling digestion are damaged, leading to issues like gastroparesis, chronic constipation, or recurrent diarrhea. These conditions disrupt the digestive system’s ability to process food, absorb nutrients, and maintain overall health. Gut neuropathies are often connected to issues like diabetes, autoimmune diseases, or injuries, making them a complicated problem that requires a thorough treatment plan. At ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX, a blend of chiropractic care, naturopathy, nutrition counseling, and other integrative therapies addresses the root causes of these conditions to promote natural healing. This article reviews the causes, symptoms, diagnostics, and holistic management strategies for gut neuropathies, highlighting ChiroMed’s patient-centered care model.
Understanding the Gut’s Nervous System
The digestive system relies on the enteric nervous system (ENS), a network of millions of neurons embedded in the gut wall, often referred to as the “second brain.” The ENS regulates digestion by controlling muscle contractions, enzyme release, and waste elimination. When damaged—known as enteric neuropathy—it disrupts these processes, causing food to move too slowly (gastroparesis) or too quickly (diarrhea). Autonomic neuropathy, affecting involuntary functions, further impairs digestion by disrupting nerves like the vagus, which governs stomach emptying (Stanford Health Care, n.d.).
Nerve damage can weaken the gut barrier, leading to inflammation, bacterial overgrowth, or malabsorption. Research highlights that oxidative stress, immune-mediated damage, or nutrient deficiencies harm enteric neurons and glia, altering gut function and systemic health (McClurg et al., 2024). These disruptions often exacerbate chronic conditions, necessitating a holistic treatment approach.
Causes of Gut Neuropathies
Several factors trigger gut neuropathies. Diabetes is a primary culprit, with prolonged high blood sugar damaging nerve fibers and their blood supply, particularly in the gut. The result leads to slowed gastric motility and conditions like gastroparesis (Meldgaard et al., 2015). Autoimmune disorders, including rheumatoid arthritis and paraneoplastic syndromes, generate antibodies that assault gut nerves, resulting in motility disturbances or pseudo-obstruction (Camilleri et al., 2021).
Infections, including viral or bacterial gastroenteritis, can inflame nerves, resulting in persistent motility problems. Toxins like chemotherapy drugs or heavy metals directly harm neurons, while certain medications, such as opioids, disrupt nerve signaling (Caula et al., 2018). Chronic inflammation or malabsorption of nerve-critical nutrients like vitamin B12 can make inflammatory diseases like Crohn’s disease or celiac disease worse (Zhang et al., 2024).
Physical trauma, such as spinal injuries from motor vehicle accidents (MVAs) or workplace incidents, can compress autonomic nerves, indirectly affecting digestion (Kumar, n.d.). Aging reduces enteric neuron density, increasing risks for constipation or dysmotility (McClurg et al., 2024). These varied causes illustrate the importance of personalized care.
Symptoms of Gut Neuropathies
Symptoms depend on the affected digestive region. Upper gut issues, like gastroparesis, cause nausea, vomiting, bloating, and feeling full after small meals, often leading to weight loss or nutrient deficiencies (NIDDK, n.d.). Lower gut neuropathies result in constipation, diarrhea, or alternating patterns, with cramping, urgency, or incontinence. Small intestine dysfunction causes bloating, pain, and malabsorption, leading to fatigue or anemia (Pathways Consult Service, n.d.).
Severe cases may present as pseudo-obstruction, where motility halts, mimicking a physical blockage (Camilleri et al., 2021). Systemic symptoms, like dizziness or abnormal sweating, indicate broader autonomic involvement (Stanford Health Care, n.d.). In diabetes, erratic digestion complicates blood sugar control, worsening neuropathy (NIDDK, n.d.). These symptoms disrupt daily life, making it necessary to implement effective interventions.
Diagnosing Gut Neuropathies
Diagnosis begins with a detailed medical history to identify risk factors like diabetes, infections, or trauma. Blood tests assess glucose levels, autoantibodies, or deficiencies in nutrients like B12 or E. Motility tests, such as gastric emptying scintigraphy, use radioactive meals to track digestion speed. Breath tests detect bacterial overgrowth, and wireless motility capsules measure transit times (Meldgaard et al., 2015).
Endoscopy or manometry evaluates muscle and nerve function, while biopsies confirm nerve damage in severe cases. Antibody tests target autoimmune markers like anti-Hu (Camilleri et al., 2021). Advanced imaging, such as MRI or digital motion X-rays, checks for spinal misalignments affecting autonomic nerves, particularly post-injury (Jimenez, n.d.a). Skin biopsies identify small fiber neuropathy linked to gut issues (Pathways Consult Service, n.d.).
Conventional Management Strategies
Treatment targets underlying causes and symptom relief. For diabetic neuropathy, strict blood sugar control slows progression (NIDDK, n.d.). Dietary changes—small, low-fat meals for gastroparesis or fiber-rich foods for constipation—support motility. Prokinetics like erythromycin stimulate gut movement, while laxatives or antidiarrheals manage bowel issues (Stanford Health Care, n.d.).
Autoimmune cases may respond to immunosuppressants like corticosteroids or IVIG (Caula et al., 2018). Supplements address nutrient deficiencies, aiding nerve repair. Severe gastroparesis may require gastric stimulators or feeding tubes. Neuropathic pain is managed with targeted medications (Kumar, n.d.). Chronic cases focus on long-term symptom management with lifestyle adjustments (Piedmont Healthcare, n.d.).
Integrated Medicine at ChiroMed
ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX, offers a comprehensive approach to gut neuropathies, blending chiropractic care, naturopathy, nutrition counseling, acupuncture, and rehabilitation. This combined approach, guided by Dr. Alexander Jimenez, focuses on finding and treating the main issues with personalized, natural methods.
Chiropractic adjustments fix problems in the spine that can press on nerves, which may help the vagus nerve work better and improve Naturopathy and nutrition counseling emphasize anti-inflammatory diets—rich in omega-3s, antioxidants, and fiber—to reduce nerve-damaging inflammation. Nutraceuticals like B12, vitamin E, or alpha-lipoic acid support nerve regeneration, tailored to lab results identifying deficiencies or inflammation markers (Jimenez, n.d.a).
Acupuncture works on nerve pathways to ease pain and improve gut function. In order to aid in digestion, rehabilitation exercises target the pelvic and core muscles. For patients with nerve pain from injuries (like car accidents, sports, or work-related incidents), ChiroMed uses advanced imaging techniques, like MRI or digital motion X-rays, to find where nerves are being pinched.
Dr. Jimenez’s dual expertise as a chiropractor and nurse practitioner enables thorough assessments. Personalized nutrition plans help people with diabetic neuropathy keep their blood sugar levels stable, which lowers oxidative stress. Post-MVA patients with whiplash may experience vagus nerve irritation and worsening gastroparesis; adjustments and soft tissue therapy alleviate this. Targeted rehab addresses workplace repetitive strains or sports injuries that misalign the spine, while holistic protocols reduce systemic inflammation for personal injuries.
ChiroMed provides detailed medical-legal documentation for insurance, workers’ compensation, or personal injury claims, ensuring seamless care coordination (Jimenez, n.d.b). Patients report reduced digestive discomfort, improved energy, and enhanced mobility, reflecting the clinic’s commitment to holistic healing.
The Spine-Gut Connection
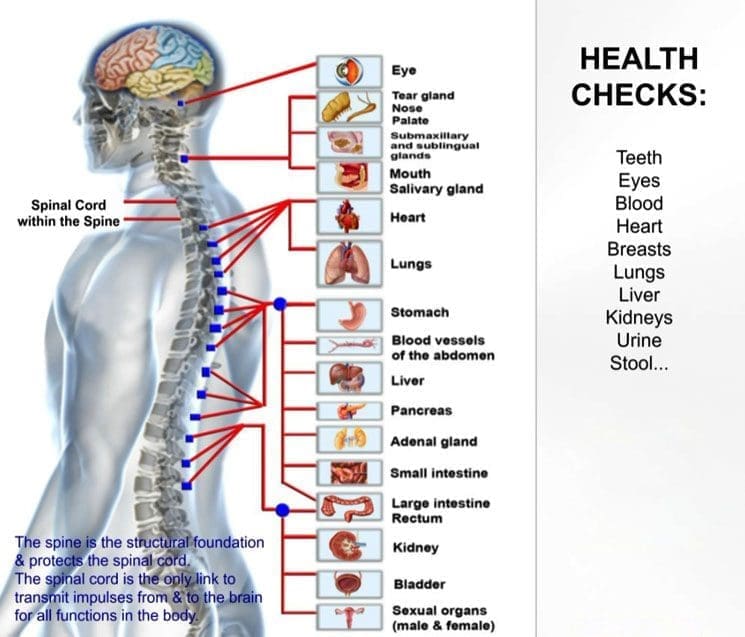
The spine, brain, and gut are interconnected via autonomic nerves, including the vagus. Misalignments or trauma can disrupt these pathways, aggravating gut neuropathy (Kumar, n.d.). ChiroMed’s holistic approach to health includes nutrition and acupuncture to help the spine stay in line, reduce inflammation, and support nerve health. This process improves communication between the gut and the brain.
Dr. Jimenez notes that patients with spinal injuries often report bloating or irregular bowels, which improve with chiropractic care and naturopathic interventions. Lab work identifies inflammation, guides dietary adjustments, and optimizes outcomes.
Preventing Gut Neuropathies
Prevention involves managing risk factors: controlling blood sugar, eating nutrient-rich foods, and avoiding toxins like excessive alcohol. Regular exercise and stress reduction support nerve health (Piedmont Healthcare, n.d.). Early intervention post-injury prevents chronic nerve dysfunction, with ChiroMed’s integrative strategies promoting resilience.
Conclusion
Gut neuropathies, driven by nerve damage from diabetes, autoimmunity, or trauma, challenge digestion and well-being. ChiroMed – Integrated Medicine Holistic Healthcare in El Paso, TX, offers a patient-centered path to relief through chiropractic care, naturopathy, and nutrition. By addressing root causes, this integrative approach restores gut health and enhances overall wellness.
References
Caula, C., Pellicano, R., & Fagoonee, S. (2018). Peripheral neuropathy and gastroenterologic disorders: An overview on an underrecognized association. European Journal of Gastroenterology & Hepatology, 30(7), 698–702. https://pmc.ncbi.nlm.nih.gov/articles/PMC6502186/
Camilleri, M., Chedid, V., & Ford, A. C. (2021). Gastrointestinal motility disorders in neurologic disease. Journal of Clinical Investigation, 131(4), e143768. https://pmc.ncbi.nlm.nih.gov/articles/PMC7880310/
Jimenez, A. (n.d.a). Injury specialists. DrAlexJimenez.com. Retrieved October 20, 2025, from https://dralexjimenez.com/
Jimenez, A. (n.d.b). Dr. Alexander Jimenez [LinkedIn profile]. LinkedIn. Retrieved October 20, 2025, from https://www.linkedin.com/in/dralexjimenez/
Kumar, A. (n.d.). The link between digestion problems and neuropathy. Advanced Pain Management. Retrieved October 20, 2025, from https://www.advpainmd.com/blog/the-link-between-digestion-problems-and-neuropathy
McClurg, D., Harris, F., & Emmanuel, A. (2024). Mechanisms of enteric neuropathy in diverse contexts of gastrointestinal dysfunction. Gut, 73(10), 1718–1730. https://pmc.ncbi.nlm.nih.gov/articles/PMC12287894/
Meldgaard, T., Keller, J., & Olesen, S. S. (2015). Diabetic neuropathy in the gut: Pathogenesis and diagnosis. Diabetologia, 59(3), 404–408. https://link.springer.com/article/10.1007/s00125-015-3831-1
National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Autonomic neuropathy. Retrieved October 20, 2025, from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy
Pathways Consult Service. (n.d.). Small fiber neuropathy and recurrent GI infections. Massachusetts General Hospital Advances. Retrieved October 20, 2025, from https://advances.massgeneral.org/research-and-innovation/case-study.aspx?id=1020
Piedmont Healthcare. (n.d.). The most common causes of peripheral neuropathy. Retrieved October 20, 2025, from https://www.piedmont.org/living-real-change/the-most-common-causes-of-peripheral-neuropathy
Stanford Health Care. (n.d.). Autonomic neuropathy. Retrieved October 20, 2025, from https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/autonomic-neuropathy.html
Zhang, Y., Liu, X., & Wang, J. (2024). Enteric neuropathy in diabetes: Implications for gastrointestinal function. World Journal of Diabetes, 15(6), 1042–1056. https://pmc.ncbi.nlm.nih.gov/articles/PMC11212710/