Bromelain and Its Health Benefits on Inflammation
Discover the benefits of bromelain on inflammation for managing pain and improving recovery time.
Bromelain’s Fight Against Inflammation: Natural Relief, Integrative Recovery Strategies, and Everyday Wellness Tips
Greetings, wellness enthusiasts! Envision your body as a thriving community where inflammation sparks like a sudden power surge – essential for protection, but disruptive if it lingers and shorts out the system. Enter bromelain, the enzyme superstar from pineapples, ready to stabilize the grid and restore calm. In this comprehensive guide (over 5,000 words of clear, engaging insights), we’ll explore bromelain’s remarkable ability to soothe inflammation, backed by science with a touch of humor to keep it lively. We’ll cover inflammation’s dual role, environmental triggers, and how combining natural remedies with integrative care can address chronic issues, especially for those recovering from injuries or managing pain in vibrant communities like El Paso. Drawing from holistic health experts, we’ll share practical tweaks to boost your recovery and vitality. No quick fixes – just evidence-based, natural paths to thriving!
We’ll keep it straightforward and approachable, perfect for a high school reading level. If inflammation’s holding you back, bromelain might be your tropical ally. Let’s dive in!
What Is Inflammation and Its Role in a Healthy Body?
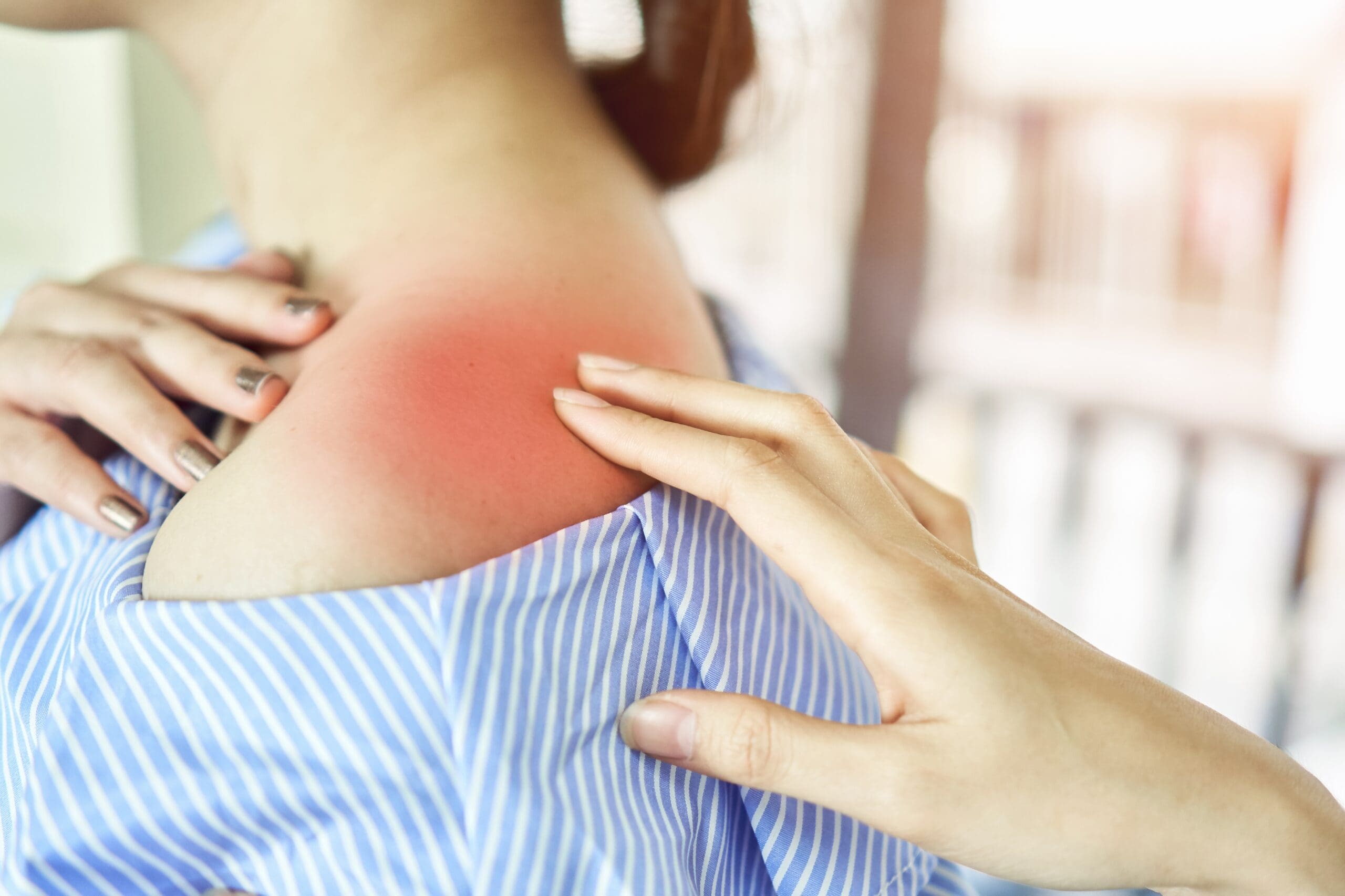
Let’s start with the essentials. Inflammation is your body’s built-in security system – like a rapid-response team tackling threats like injuries or infections. When activated, it sends cells, chemicals, and fluids to the site, causing redness, swelling, warmth, and sometimes pain (Cleveland Clinic, n.d.). In a healthy body, this is a lifesaver: it isolates dangers, clears damaged tissue, and kickstarts healing while maintaining balance, known as homeostasis (Yale Medicine, 2020).
Picture this: You strain your back during a weekend hike. Inflammation rushes in, delivering nutrient-rich blood to repair the damage. Without it, injuries could linger like unwelcome guests, and pathogens might take over. It regulates immunity, helping you resist daily germs, and even supports tissue repair post-exercise – your body’s way of saying, “Let’s rebuild stronger!” (Vanderbilt Medicine, 2015). But when it persists, it links to serious conditions like heart disease or chronic pain (Yale Medicine, 2022). In essence, inflammation is your body’s guardian – vital but needing oversight.
Quick chuckle: Why does inflammation cause swelling? It’s your body puffing up like a life preserver to trap the bad stuff – but it needs to deflate eventually!
References
- Cleveland Clinic. (n.d.). What is inflammation? Types, causes & treatment. https://my.clevelandclinic.org/health/symptoms/21660-inflammation
- Yale Medicine. (2020). Inflammation: A double-edged sword for the immune system. https://medicine.yale.edu/news/yale-medicine-magazine/article/inflammation-a-double-edged-sword-for-the-immune-system/
- Yale Medicine. (2022). How inflammation affects your health. https://www.yalemedicine.org/news/how-inflammation-affects-your-health
- Vanderbilt Medicine. (2015). The good, the bad and the ugly of inflammation. https://medschool.vanderbilt.edu/vanderbilt-medicine/the-good-the-bad-and-the-ugly-of-inflammation/
Acute vs. Chronic Inflammation: The Key Differences
Let’s distinguish the two: acute and chronic inflammation. Acute is the quick responder – like a first-aid crew handling a crisis in hours or days before exiting (Harvard Health, 2020). Think of a twisted ankle: brief swelling and pain, then resolved. It’s beneficial, boosting blood flow and immune cells for fast recovery.
Chronic inflammation, however, is the lingering issue, quietly persisting for months or years and potentially harming tissues (Cleveland Clinic, n.d.). Causes include autoimmune mix-ups, ongoing irritants, or unresolved acute injuries, possibly fueling conditions like chronic back pain or joint issues (NCBI, 2023).
Main distinctions: Acute is temporary, helpful, and fades; chronic is prolonged, harmful, and pervasive. Acute aids healing through enhanced circulation and cleanup (Physiopedia, n.d.). Chronic drains energy, causing persistent discomfort and higher health risks (Encompass Health, 2021). Laugh moment: Acute inflammation is a quick warm-up – intense but done. Chronic? A marathon with no finish line, leaving you sore!
This understanding guides recovery: Rest for acute flares, integrative strategies for chronic challenges.
References
- Cleveland Clinic. (n.d.). What is inflammation? Types, causes & treatment. https://my.clevelandclinic.org/health/symptoms/21660-inflammation
- Harvard Health. (2020). Understanding acute and chronic inflammation. https://www.health.harvard.edu/staying-healthy/understanding-acute-and-chronic-inflammation
- Encompass Health. (2021). Acute inflammation vs. chronic inflammation. https://www.encompasshealth.com/health-resources/articles/acute-inflammation-vs-chronic-inflammation
- NCBI. (2023). Chronic inflammation – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493173/
- Physiopedia. (n.d.). Inflammation acute and chronic. https://www.physio-pedia.com/Inflammation_Acute_and_Chronic
Environmental Factors Driving Inflammation
Your environment isn’t just a backdrop – it actively shapes inflammation levels. Factors like pollution, diet, stress, and location can escalate it (Nature Medicine, 2019). Air pollution introduces toxins, sparking systemic stress and swelling (The University of Queensland, n.d.). It’s like inhaling tiny disruptors that agitate your defenses.
Nutrition plays a big role: Processed foods and unhealthy fats fuel inflammation, while antioxidant-rich produce like fruits and veggies cools it (PMC, 2019). Toxins from pesticides or metals disrupt gut barriers, spreading inflammation (ScienceDirect, 2013). Stress spikes cortisol, which, over time, intensifies inflammation (Northwestern University, 2017).
Other triggers: Smoking irritates tissues, excess weight sends inflammatory signals from fat stores, and early-life exposures like poor nutrition increase later risks (PMC, 2019). In conditions like gut disorders, environmental factors alter integrity and microbial balance, heightening chances (CGH Journal, 2024). Fun thought: City pollution? It’s like your body hosting an uninvited inflammation rave – time to shut it down with healthier habits!
Counter these with tweaks like clean eating or stress management – more from integrative health experts ahead.
References
- PMC. (2019). Impact of nutritional and environmental factors on inflammation. https://pmc.ncbi.nlm.nih.gov/articles/PMC6652064/
- Nature Medicine. (2019). Chronic inflammation in the etiology of disease across the life span. https://www.nature.com/articles/s41591-019-0675-0
- ScienceDirect. (2013). Causes and consequences of chronic systemic low-grade inflammation. https://www.sciencedirect.com/science/article/pii/S0955286313000545
- The University of Queensland. (n.d.). The dangerous century. https://stories.uq.edu.au/imb/the-edge/inflammation/the-dangerous-century/index.html
- Northwestern University. (2017). How babies’ environments lead to poor health later. https://news.northwestern.edu/stories/2017/july/babies-environments-poor-health-later-study/
- CGH Journal. (2024). Environmental factors associated with risk of Crohn’s disease development. https://www.cghjournal.org/article/S1542-3565%2824%2900450-6/fulltext
Fighting Inflammation Naturally- Video
Bromelain: Nature’s Inflammation Soother
Bromelain – not a sci-fi antagonist, but a potent enzyme from pineapple stems and juice, long used in traditional remedies and now validated for calming inflammation (Agrawal, 2022). It’s nature’s gentle healer, breaking down proteins, reducing swelling, and balancing immune responses.
It excels in easing joint pain or post-injury recovery, often with fewer side effects than medications (Varilla et al., 2023). Quirky fact: Eating pineapple helps, but supplements deliver the real punch – don’t expect a fruit smoothie to fix your aches overnight!
Why Bromelain Clinically Reduces Inflammation
The science: Bromelain tames inflammation by blocking pro-inflammatory agents like prostaglandins and cytokines, reducing swelling and discomfort (Hikisz & Bernasinska-Slomczewska, 2021). It promotes fibrinolysis, clearing clots to improve blood flow and remove debris (Chakraborty et al., 2024).
In clinical settings, it breaks down proteins trapping fluids, speeding recovery from injuries or sinus issues (Varilla et al., 2023). For chronic inflammation, it moderates immune overreactions (Kargutkar et al., 2024). Why it’s effective? It targets root causes naturally, avoiding the downsides of some drugs.
Humor: Bromelain’s like your body’s tropical masseuse, kneading out inflammation with a pineapple twist.
Deep dive: It inhibits NF-kB, a major inflammation trigger, and boosts protective enzymes. It aids disc recovery by calming responses, which is key for spinal health (Cunha et al., 2018). Similar to curcumin for post-injury soreness, but with a fruity edge (Fernández-Lázaro et al., 2020).
References
- Agrawal, P. (2022). Bromelain: A potent phytomedicine. https://pubmed.ncbi.nlm.nih.gov/36110474/
- Varilla, C., et al. (2023). Bromelain: A review of its mechanisms, pharmacological effects and potential applications. https://pubmed.ncbi.nlm.nih.gov/37650738/
- Arshad, N., et al. (2016). Role of antioxidants and natural products in inflammation. https://pubmed.ncbi.nlm.nih.gov/27803762/
- Kargutkar, S., et al. (2024). Exploring the therapeutic potential of bromelain: Applications, benefits, and mechanisms. https://pubmed.ncbi.nlm.nih.gov/38999808/
- Chakraborty, A. J., et al. (2024). Bromelain as a natural anti-inflammatory drug: A systematic review. https://pubmed.ncbi.nlm.nih.gov/38676413/
- Hikisz, P., & Bernasinska-Slomczewska, J. (2021). Beneficial properties of bromelain. https://pubmed.ncbi.nlm.nih.gov/34959865/
- Cunha, G. M., et al. (2018). The inflammatory response in the regression of lumbar disc herniation. https://pubmed.ncbi.nlm.nih.gov/30400975/
- Fernández-Lázaro, D., et al. (2020). Modulation of exercise-induced muscle damage, inflammation, and oxidative markers by curcumin supplementation. https://pubmed.ncbi.nlm.nih.gov/32075287/
Bromelain’s Benefits and Support for the Body
From key research (Hikisz & Bernasinska-Slomczewska, 2021), bromelain excels in protein digestion, swelling reduction, and clot prevention. It clears inflammatory debris, enhances digestion, and improves nutrient absorption.
Benefits: It eases joint discomfort, speeds wound healing, and clears sinus pathways by thinning mucus. It shows potential in targeting abnormal cells. Body-wide, it strengthens immunity, supports heart health by moderating pressure, and aids respiratory conditions by soothing airways.
How it helps: Balances immune signals to prevent chronic issues and supports digestive health for conditions like IBS. Jest: Bromelain’s pineapple pledge: “Eat me, and I’ll shrink the puffiness!”
More: Its antioxidants combat stress linked to inflammation (Arshad et al., 2016). It reduces post-injury soreness, similar to curcumin, making it ideal for recovery (Tan & Zhang, 2019).
References
- Hikisz, P., & Bernasinska-Slomczewska, J. (2021). Beneficial properties of bromelain. https://pubmed.ncbi.nlm.nih.gov/34959865/
- Arshad, N., et al. (2016). Role of antioxidants and natural products in inflammation. https://pubmed.ncbi.nlm.nih.gov/27803762/
- Tan, Y. Q., & Zhang, J. (2019). Effect of curcumin supplementation on exercise-induced oxidative stress, inflammation, muscle damage, and muscle soreness. https://pubmed.ncbi.nlm.nih.gov/31025894/
Integrative Care and Non-Invasive Strategies for Chronic Inflammation
Integrative care, combining chiropractic, nutrition, and holistic approaches, goes beyond quick fixes – it’s a tailored strategy for reducing chronic inflammation’s overlapping risks, especially for pain or mobility issues. Personalized plans optimize alignment, nutrition, and movement to lessen swelling (Cleveland Clinic, n.d.). Combined with natural remedies, exercise, or acupuncture, it targets interconnected factors like fatigue, joint stress, or pain cycles.
How it works: Corrects misalignments to lower systemic inflammation, benefiting conditions like back pain or nerve irritation (Western Reserve Hospital, n.d.). Complementary methods, like nutritional counseling and mobility programs, promote healing without medications (Driver Chiropractic, 2025).
For immune-related conditions, structured exercise plans help regulate inflammation (Sgreccia et al., 2022). Targeted techniques, like massage, relieve tension points for lasting comfort (Shah et al., 2015). Humor: Integrative pros are like wellness architects, building a foundation so inflammation doesn’t topple your health!
Clinics in vibrant communities like El Paso, inspired by integrative care models, offer customized sessions to combat inflammation through holistic recovery and musculoskeletal health.
References
- Cleveland Clinic. (n.d.). Chiropractic adjustment care, treatment & benefits. https://my.clevelandclinic.org/health/treatments/21033-chiropractic-adjustment
- Western Reserve Hospital. (n.d.). Understanding chiropractic care for chronic pain. https://www.westernreservehospital.org/blog/understanding-chiropractic-care-chronic-pain
- Driver Chiropractic. (2025). Chiropractic treatment eases chronic inflammation & joint pain. https://www.driverchiropractic.com/2025/03/18/how-chiropractic-treatment-eases-chronic-inflammation-and-joint-pain/
- Shah, J. P., et al. (2015). Myofascial trigger points then and now: A historical and scientific perspective. https://pubmed.ncbi.nlm.nih.gov/25724849/
- Sgreccia, E., et al. (2022). The effect of exercise on patients with rheumatoid arthritis on the modulation of inflammation. https://pubmed.ncbi.nlm.nih.gov/34874837/
Expert Insights from Dr. Alexander Jimenez on Inflammation Management
In wellness-focused regions like El Paso, professionals like Dr. Alexander Jimenez, DC, APRN, FNP-BC, blend integrative care with holistic approaches to tackle inflammation (ChiroMed, n.d.). His philosophy: Address root causes like misalignments, nutrition gaps, or physical stressors to reduce chronic risks.
Practical tweaks: Incorporate anti-inflammatory foods (like bromelain-rich pineapple), regular mobility exercises, and stress-reducing practices like acupuncture. Functional movement drills build resilience (ChiroMed, n.d.). Advanced assessments create tailored recovery plans.
Fun quip: Dr. Jimenez is like an inflammation maestro – orchestrating relief with adjustments and nutrition, no baton needed!
Clients report improved mobility, reduced pain, and enhanced vitality through his integrative strategies, ideal for active lifestyles.
Managing Personal Injuries in El Paso: Specialized Integrative Support
El Paso’s dynamic community sees frequent injuries from accidents, work, or sports, where specialized integrative care excels in recovery (ChiroMed, n.d.). Experts like Dr. Jimenez connect injuries to advanced diagnostics, imaging, and comprehensive evaluations for precise recovery plans.
He bridges health services with legal documentation, providing thorough reports for claims or rehab needs. With extensive experience, he addresses issues from whiplash to complex spinal injuries using non-invasive methods like chiropractic and acupuncture (ChiroMed, n.d.).
Laugh: Injuries hit like a roadblock, but expert care turns “crash” into “cruise” like a wellness comeback!
Local clinics emphasize gentle, integrative recovery, collaborating with nutritionists and therapists for comprehensive support in injury scenarios.
Everyday Adjustments: Integrative Wisdom for Inflammation Control
Dr. Jimenez advises: Blend bromelain through pineapple or supplements into your diet. Add daily mobility work to temper inflammation; practice mindfulness or acupuncture for calm (ChiroMed, n.d.). Strengthen muscles and stay hydrated.
Track progress with assessments and avoid environmental toxins. These steps stack to reduce risks, fostering vitality (ChiroMed, n.d.).
Humor: Small changes? Like swapping junk food for greens – your body throws a gratitude party without the inflammation wreck!
References for Dr. Jimenez and Integrative Care Sections
- ChiroMed. (n.d.). Integrative medicine and holistic healthcare services. https://chiromed.com/
Conclusion
Concluding this deep dive into bromelain’s inflammation-fighting prowess, natural benefits, and synergy with integrative care and lifestyle tweaks, these approaches clearly pave the way for vibrant health. From bromelain’s evidence-based perks to holistic strategies easing chronic issues, these tools empower you to recover and thrive.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before starting new supplements, treatments, or lifestyle changes, especially with existing conditions. The content draws from research and should be taken seriously for informed health decisions. Results vary, and no outcomes are guaranteed.
[wp-embedder-pack width=”100%” height=”400px” download=”all” download-text=”” url=”http://file:///C:/Users/TeamsterInjuryMember/AppData/Local/Packages/5319275A.WhatsAppDesktop_cv1g1gvanyjgm/LocalState/sessions/8BE472A4F65E94BA0FF891772B88EA87F6CC6B3F/transfers/2025-41/nutrients-13-04313-with-cover.pdf” /]