Chiropractic Care Benefits for Migraines From Head Injuries
Understand the benefits of chiropractic care in addressing migraines and the impact of head injuries for many individuals.
Understanding Traumatic Brain Injury: How Head Injuries Cause Headaches, Migraines, and Cognitive Problems
Traumatic brain injury represents one of the most serious health conditions affecting millions of people each year. When someone experiences a blow to the head or a sudden jolt that shakes the brain inside the skull, the resulting damage can create a wide range of symptoms that affect daily life. Understanding how these injuries work and what symptoms they cause helps people recognize when they need medical attention and what treatment options are available.
What Is Traumatic Brain Injury?
Traumatic brain injury, commonly called TBI, occurs when an external force damages the brain. This injury happens when the head receives a sudden impact, causing the brain to move rapidly inside the skull. The Centers for Disease Control and Prevention reports that TBI represents a major cause of death and disability in the United States. These injuries range from mild concussions to severe brain damage that can permanently change a person’s life. mayoclinic+2
The brain sits protected inside the skull, surrounded by cerebrospinal fluid that acts like a cushion. When someone experiences a violent blow to the head, the brain can strike the inside of the skull, causing bruising, torn tissues, bleeding, and other physical damage. Sometimes the injury happens even without the head hitting anything directly—rapid acceleration or deceleration can shake the brain violently enough to cause damage. clevelandclinic+1
TBI occurs through several different mechanisms. Direct impact injuries happen when something strikes the head with force, such as during a fall, a sports collision, or an assault. Penetrating injuries occur when an object breaks through the skull and enters the brain tissue. Blast injuries, common in military settings, create pressure waves that damage brain structures. Motor vehicle accidents represent one of the leading causes of traumatic brain injury, often combining multiple injury mechanisms including impact, acceleration, and deceleration forces. americanbrainfoundation+2
Medical professionals classify TBI into three severity levels based on symptoms and diagnostic findings. Mild TBI, also known as a concussion, represents the most common form and may cause temporary confusion, headache, and other symptoms that typically resolve within weeks. Moderate TBI involves loss of consciousness lasting from several minutes to hours and confusion that can persist for days or weeks. Severe TBI results from crushing blows or penetrating injuries that cause extended unconsciousness, significant brain damage, and potentially permanent disability. mayoclinic+1
The immediate effects of TBI depend on which parts of the brain sustained damage and how severe that damage was. The frontal lobes, which control thinking, planning, and emotional regulation, are often affected by injury in TBI. Damage to the temporal lobes can affect memory and language. The brainstem, which controls basic life functions like breathing and heart rate, can be injured in severe TBI, creating life-threatening emergencies. alz+1
How TBI Causes Headaches and Migraines
Headaches represent one of the most common and persistent symptoms following traumatic brain injury. Research shows that between 30% and 90% of people who experience TBI develop headaches afterward. These post-traumatic headaches can begin immediately after the injury or develop days or even weeks later. Understanding why TBI causes headaches requires looking at the complex changes happening inside the brain and surrounding structures after injury. connectivity+3
When the brain experiences trauma, several physical and chemical changes occur that trigger headache pain. The initial impact can damage blood vessels in the brain, causing bleeding and inflammation. This inflammation triggers the release of pain-causing chemicals that activate nerve endings throughout the head and neck region. The meninges, the protective membranes that cover the brain, contain numerous pain-sensitive nerve fibers that respond to inflammation by sending pain signals. pmc.ncbi.nlm.nih+2
Brain tissue itself does not contain pain receptors, but the structures surrounding the brain are highly sensitive to pain. The blood vessels, meninges, and cranial nerves all possess pain receptors that can generate headache sensations. After a TBI, these structures may become more sensitive, a condition known as central sensitization, where the nervous system becomes hyperresponsive to pain signals. ncbi.nlm.nih+1
The connection between TBI and headaches also involves disruption of normal brain chemistry. The brain relies on neurotransmitters—chemical messengers that allow nerve cells to communicate—to function properly. Traumatic injury can disturb the balance of these neurotransmitters, particularly serotonin, which plays a crucial role in pain regulation. When serotonin levels drop or become imbalanced, the brain’s pain-filtering systems may not work correctly, allowing pain signals to reach consciousness more easily. migrainedisorders+2
Migraines represent a specific type of severe headache that many people develop after experiencing TBI. Research published in scientific journals demonstrates that people who have had a traumatic brain injury face a significantly increased risk of developing migraines compared to those who have never experienced head trauma. One study found that TBI approximately doubles the risk of developing new migraine headaches. pmc.ncbi.nlm.nih
The mechanisms linking TBI to migraines involve complex changes in brain function. The trigeminal nerve, which provides sensation to much of the face and head, becomes activated during migraines. This activation releases inflammatory substances called neuropeptides that cause blood vessel dilation and further inflammation. After TBI, the trigeminal nerve system may become more easily triggered, lowering the threshold for migraine attacks. emedicine.medscape+2
Brain imaging studies reveal that inflammation and altered connectivity between different brain regions persist long after the initial injury. These changes in how different parts of the brain communicate with each other can make the brain more susceptible to migraine triggers. The brain regions involved in pain processing, sensory filtering, and stress response show altered function in people with post-traumatic migraines. sciencedirect
Clinical Insights from Dr. Alexander Jimenez on Head Injury Assessment
Dr. Alexander Jimenez, a dual-credentialed chiropractor and nurse practitioner practicing in El Paso, brings a unique perspective to evaluating and treating patients with traumatic brain injury and post-traumatic headaches. His clinic specializes in treating injuries from various sources, including workplace accidents, sports injuries, personal injuries, and motor vehicle accidents. The dual-scope approach allows for a comprehensive assessment that combines chiropractic evaluation of neuromusculoskeletal function with advanced medical diagnostic capabilities. advantagehcs
When patients present with head injuries, Dr. Jimenez’s clinical approach emphasizes thorough neurological examination to identify the full extent of injury. This assessment includes evaluating cranial nerve function, testing reflexes, assessing balance and coordination, and screening for cognitive changes. The clinic utilizes advanced neuromusculoskeletal imaging to visualize structural damage that may contribute to ongoing symptoms. These imaging techniques include computed tomography (CT) scans, which excel at detecting skull fractures, bleeding, and swelling in the acute phase after injury. Magnetic resonance imaging (MRI) provides superior detail of soft tissue damage, including subtle brain injuries that may not appear on CT scans. pmc.ncbi.nlm.nih+4
Dr. Jimenez emphasizes that proper documentation of injuries plays a critical role, particularly in cases involving motor vehicle accidents or workplace injuries where legal and insurance considerations arise. Detailed medical records, which document the mechanism of injury, initial symptoms, physical examination findings, diagnostic test results, and treatment plans, serve essential functions in both patient care and legal proceedings. These records establish the connection between the traumatic event and the patient’s symptoms, which becomes crucial when seeking compensation for injuries. njadvocates+3
Cognitive Function Changes After TBI
The brain serves as the central control center for all mental processes, including thinking, learning, remembering, and decision-making. When traumatic injury damages brain tissue, these cognitive functions often become impaired. Understanding how TBI affects cognitive function helps patients and families recognize symptoms and seek appropriate treatment. pubmed.ncbi.nlm.nih+1
Cognitive impairment represents one of the most challenging consequences of traumatic brain injury because it affects so many aspects of daily life. The severity and pattern of cognitive problems depend on which brain regions sustained damage and how extensive that damage was. Research involving thousands of patients shows that cognitive impairment occurs across all severity levels of TBI, though more severe injuries generally produce more pronounced deficits. jamanetwork+1
Memory problems rank among the most common cognitive complaints after TBI. Short-term memory, which involves holding information in mind for brief periods, often becomes impaired. People may struggle to remember conversations, appointments, or where they placed items. Long-term memory, particularly the formation of new memories, can also be disrupted. The hippocampus, a brain structure critical for memory formation, is particularly vulnerable to injury during trauma. headway+1
Attention and concentration difficulties create significant challenges for people recovering from TBI. The ability to focus on tasks, filter out distractions, and shift attention between different activities may be compromised. These problems make it difficult to perform work duties, follow conversations, or engage in activities that require sustained mental effort. Divided attention—the ability to manage multiple tasks simultaneously—becomes especially problematic. uwmsktc.washington+1
Processing speed, which refers to how quickly the brain can take in information, understand it, and respond, typically slows after TBI. This slowing affects many aspects of functioning, from reading comprehension to reaction times while driving. Simple tasks that once seemed automatic may now require conscious effort and extra time. jamanetwork
Executive functions encompass higher-level cognitive abilities, including planning, organizing, problem-solving, and self-monitoring. The frontal lobes, which control these functions, are often damaged in TBI. Impairment of executive functions can make it difficult to manage daily responsibilities, make appropriate decisions, or adapt to changing situations. People may struggle with initiating tasks, following multi-step instructions, or recognizing and correcting errors. alz+1
Language and communication abilities can be affected by TBI, although the specific deficits vary depending on the location of the injury. Some people struggle to find the right words, form sentences, or comprehend complex language. Others may struggle with the social aspects of communication, such as interpreting social cues, taking turns in conversation, or adapting their communication style to different situations. uwmsktc.washington+1
Head Symptoms Associated with Cognitive Impairment
The cognitive changes that occur after TBI often coincide with physical symptoms affecting the head. These symptoms interconnect in ways that compound difficulties and interfere with recovery. Headaches themselves can worsen cognitive function by creating pain that distracts from mental tasks and disrupts concentration. The constant presence of head pain makes it harder to think clearly, remember information, or engage in problem-solving. pmc.ncbi.nlm.nih+2
Mental fog or clouded thinking represents a common complaint among people with TBI. This sensation of thinking through a haze makes mental tasks feel effortful and exhausting. The brain appears to operate more slowly, and thoughts may feel disorganized or disjointed. This mental fog often accompanies headaches and worsens with mental exertion. concussionalliance+1
Dizziness and balance problems frequently occur after TBI, creating a sense of instability or spinning that originates from dysfunction in the vestibular system. The inner ear structures that control balance can be damaged during head trauma, or the brain regions that process balance information may become impaired. These balance problems affect the ability to walk steadily, drive safely, or perform activities requiring coordination. mentalhealth.va+2
Pressure sensations inside the head trouble many people with TBI. This feeling of tightness, fullness, or pressure can be localized to specific areas or felt throughout the entire head. Sometimes, this pressure sensation accompanies actual changes in intracranial pressure due to swelling or fluid accumulation; however, it often represents altered sensory processing rather than true pressure changes. connectivity
Facial pain and jaw discomfort can develop after head trauma, particularly when the temporomandibular joint (TMJ) sustains injury during the trauma. The TMJ connects the jawbone to the skull, allowing for chewing and speaking. Injury to this joint or the surrounding muscles can create pain that radiates throughout the face, head, and neck. elizabethsandelmd+1
Types of Headaches Following Traumatic Brain Injury
Post-traumatic headaches can take several different forms, each with distinct characteristics and mechanisms. Recognizing the type of headache helps guide the development of appropriate treatment strategies. The International Classification of Headache Disorders provides standardized criteria for diagnosing different headache types, which healthcare providers use to categorize post-traumatic headaches. nature+2
Acute Post-Traumatic Headache
Acute post-traumatic headache develops within seven days of the injury or within seven days of regaining consciousness after the injury. These headaches typically resolve within three months of their onset. The pain may feel dull and constant or sharp and intermittent, depending on the underlying cause. Acute post-traumatic headaches often accompany other symptoms such as nausea, dizziness, sensitivity to light and sound, and cognitive difficulties. ncbi.nlm.nih+1
Persistent Post-Traumatic Headache
When headaches continue beyond three months after the traumatic injury, they are classified as persistent or chronic post-traumatic headaches. Research indicates that approximately 20% to 50% of people who develop headaches after TBI continue experiencing them long-term. These persistent headaches can last for months or even years after the initial injury. The chronic nature of these headaches has a significant impact on quality of life, interfering with work, relationships, and daily activities. ichd-3+3
Persistent post-traumatic headaches can evolve over time, changing in frequency, intensity, or character. Some people experience daily headaches, while others have episodic attacks separated by pain-free periods. The unpredictability of these headaches creates additional stress and anxiety, which can further worsen the headache pattern. pmc.ncbi.nlm.nih+1
Migraine-Type Post-Traumatic Headaches
Many post-traumatic headaches display characteristics typical of migraines. These headaches involve moderate to severe throbbing or pulsating pain, usually affecting one side of the head. The pain intensifies with physical activity such as walking or climbing stairs. Nausea and vomiting commonly accompany migraine-type headaches. Sensitivity to light (photophobia) and sound (phonophobia) makes it difficult to tolerate normal environmental stimuli. neurology+3
Migraine headaches can include an aura phase, which involves temporary neurological symptoms that typically develop before the headache pain begins. Visual auras are most common and may include seeing flashing lights, zigzag lines, or temporary blind spots. Some people experience sensory auras characterized by tingling or numbness, typically affecting one side of the body. Language disturbances or difficulty speaking can occur during the aura phase. mayoclinic+1
The relationship between TBI and migraines extends beyond the immediate post-injury period. People who experience migraines after TBI often develop chronic migraine disorder, defined as having headache on 15 or more days per month, with at least eight days meeting migraine criteria. This chronic pattern significantly disrupts functioning and requires comprehensive management strategies. pmc.ncbi.nlm.nih
Tension-Type Headaches After TBI
Tension-type headaches represent another common pattern of post-traumatic headache. These headaches create a sensation of pressure or tightness, often described as feeling like a tight band around the head. The pain is typically mild to moderate in intensity and affects both sides of the head. Unlike migraines, tension-type headaches usually do not cause nausea or vomiting and do not worsen significantly with routine physical activity. americanmigrainefoundation+3
Muscle tension in the head, neck, and shoulder regions contributes to tension-type headaches. After TBI, muscle tightness often increases due to several factors, including pain, altered posture, stress, and direct muscle injury during the trauma. This muscle tension creates sustained contraction that generates pain signals and reduces blood flow to affected tissues. physio-pedia+3
The psychological stress associated with recovering from TBI can trigger or worsen tension-type headaches. Anxiety about symptoms, worry about returning to normal activities, and frustration with ongoing limitations create emotional tension that manifests as physical muscle tightness. Sleep disturbances, common after TBI, also contribute to tension-type headaches by preventing adequate rest and recovery. aafp+1
Cervicogenic Headaches
Cervicogenic headaches originate from problems in the neck (cervical spine) but are experienced as headaches in the head. These headaches are particularly common after motor vehicle accidents and other traumas that create whiplash-type injuries to the neck. The sudden acceleration-deceleration forces during these injuries can damage the joints, ligaments, muscles, and nerves of the cervical spine. pmc.ncbi.nlm.nih+3
Cervicogenic headaches typically affect one side of the head and may be accompanied by neck pain and stiffness. The pain often starts at the base of the skull and radiates forward toward the forehead, temple, or area around the eye. Certain neck movements or sustained neck positions can trigger or worsen these headaches. Pressing on specific tender points in the neck may reproduce the headache pain, helping healthcare providers identify cervicogenic headaches. clevelandclinic+1
The upper cervical spine, particularly the C1-C3 vertebrae and their associated nerves, plays a crucial role in cervicogenic headaches. These upper cervical nerves share connections with the trigeminal nerve, which provides sensation to much of the head and face. When injury or dysfunction affects the upper cervical spine, pain signals can be referred along these nerve connections, creating headache sensations. physio-pedia
Dr. Jimenez’s clinic places particular emphasis on evaluating cervical spine involvement in patients presenting with post-traumatic headaches. The dual chiropractic and medical training allows for comprehensive assessment of both spinal mechanics and neurological function. This evaluation includes examining neck range of motion, palpating for areas of tenderness or restriction, testing nerve function, and reviewing imaging studies to identify structural problems. pubmed.ncbi.nlm.nih+3
Cluster Headaches and Trigeminal Autonomic Cephalalgias
Though less common than other headache types, cluster headaches and related conditions can occasionally develop after traumatic brain injury. Cluster headaches create severe, excruciating pain localized around one eye or on one side of the head. The pain reaches maximum intensity quickly and typically lasts 15 minutes to three hours. During attacks, people often feel restless and agitated rather than still, which distinguishes cluster headaches from migraines. pmc.ncbi.nlm.nih+2
Cluster headaches earn their name because they occur in clusters or cycles, with multiple attacks happening daily for weeks or months, followed by periods of remission. The attacks often occur at the same time each day and may wake people from sleep. Autonomic symptoms accompany the pain, including tearing, redness of the eye, nasal congestion or runny nose, eyelid drooping, and sweating on the affected side of the face. practicalneurology+2
The trigeminal autonomic reflex pathway, which connects the trigeminal nerve with autonomic nerve centers in the brainstem, becomes activated during these headaches. This activation causes autonomic symptoms, such as tearing and nasal congestion. Head trauma can potentially damage or alter the function of these neural pathways, though the exact mechanisms linking TBI to cluster headaches require further research. pmc.ncbi.nlm.nih
Sensory Dysfunction and Associated Head and Neck Symptoms
Traumatic brain injury often damages the sensory systems that allow people to perceive and interpret information from their environment. These sensory problems create significant challenges and often contribute to headaches and other symptoms affecting the head and neck region. Understanding these sensory changes helps explain why people with TBI experience such complex and varied symptoms. tbi.vcu+2
Light Sensitivity (Photophobia)
Sensitivity to light represents one of the most common and distressing sensory problems after TBI. Research indicates that between 40% and 80% of people with traumatic brain injury develop photophobia. This heightened sensitivity makes normal lighting levels feel uncomfortably bright or even painful. Indoor lighting, computer screens, and especially sunlight can trigger discomfort, eye pain, squinting, and worsening of headaches. connectivity+1
The mechanisms underlying photophobia after TBI involve several interconnected systems. The visual pathways that transmit light information from the eyes to the brain can become hypersensitive after injury. The trigeminal nerve, which provides sensation to the eyes and face, becomes more reactive to light stimulation. This nerve connects directly to pain-processing regions in the brain, explaining why bright light can trigger or worsen headaches. theraspecs+1
Brain regions involved in processing visual information and filtering sensory input may function abnormally after TBI. The brain normally filters out irrelevant sensory information, allowing people to focus on important stimuli while ignoring background noise or changes in lighting. After traumatic injury, this filtering system may malfunction, causing the brain to become overwhelmed by sensory input that would normally be manageable. connectivity+1
Photophobia significantly impacts daily functioning. Many people need to wear sunglasses even indoors, avoid bright environments, and limit screen time. These restrictions can interfere with work, social activities, and leisure pursuits. The constant need to manage light exposure can create additional stress and contribute to social isolation. theraspecs+1
Sound Sensitivity (Phonophobia)
Increased sensitivity to sound, called phonophobia or hyperacusis, commonly occurs alongside light sensitivity after TBI. Everyday sounds such as traffic noise, conversations, music, or household appliances may seem unbearably loud. This heightened sensitivity can trigger headaches, increase stress, and make it difficult to concentrate. mindeye+1
The auditory system processes sound through complex pathways that involve the inner ear, the auditory nerve, and multiple brain regions. After TBI, any component of this system may become damaged or dysfunctional. The cochlea in the inner ear can be injured by traumatic forces, resulting in hearing loss or tinnitus. The auditory nerve pathways may be stretched or damaged, which can alter how sound signals are transmitted to the brain. tbi.vcu
Central auditory processing, which involves how the brain interprets and makes sense of sounds, often becomes impaired after TBI. People may have difficulty distinguishing speech from background noise, determining the direction of sounds, or processing rapid sequences of auditory information. These processing problems make noisy environments particularly challenging and exhausting. tbi.vcu+1
The brain regions that regulate sensory gating—the ability to filter out unimportant sounds—may not function normally after TBI. This filtering failure means that all sounds reach consciousness with similar intensity, creating a sense of being bombarded by noise. The constant sensory overload contributes to mental fatigue, stress, and headaches. mindeye+1
Visual Disturbances
Visual problems affect approximately 40% to 50% of people with traumatic brain injury. These problems range from difficulty focusing to double vision, blurred vision, and loss of visual field. The visual system relies on precise coordination between the eyes, the muscles that move them, and the brain regions that process visual information. Trauma can disrupt any part of this complex system. salusuhealth+1
Eye movement problems create particular difficulties after TBI. The cranial nerves that control the muscles of the eye may be damaged, causing weakness or incoordination of eye movements. This can result in double vision (diplopia), where the two eyes do not align properly, creating separate images. Reading becomes exhausting because the eyes struggle to track smoothly across lines of text. frontiersin+2
Visual processing deficits affect how the brain interprets visual information, even when the eyes themselves function normally. People may experience difficulty with depth perception, making it challenging to judge distances or navigate stairs. Visual memory problems can make it hard to recognize faces or remember visual information. Visual attention deficits affect the ability to scan the environment effectively and notice important visual details. salusuhealth+1
The connection between vision and balance becomes apparent when visual problems contribute to dizziness and instability. The brain relies on visual information to maintain balance and orient the body in space. When visual input becomes distorted or unreliable after TBI, balance systems struggle to compensate, creating feelings of unsteadiness. frontiersin
Balance and Vestibular Dysfunction
The vestibular system, located in the inner ear, detects head movements and helps maintain balance and spatial orientation. This system can be damaged during head trauma, creating persistent dizziness, vertigo, and balance problems. Vestibular dysfunction affects approximately 30% to 65% of people with TBI. pmc.ncbi.nlm.nih+2
Vertigo, the sensation that the environment is spinning or moving when it is actually still, creates significant distress and disability. This spinning sensation can be constant or triggered by specific head movements. Benign paroxysmal positional vertigo (BPPV), which occurs when calcium crystals in the inner ear become displaced, commonly develops after head trauma. pmc.ncbi.nlm.nih
Balance problems make it difficult to walk steadily, especially on uneven surfaces or in low-light conditions when visual cues are limited. The brain normally integrates information from the vestibular system, vision, and sensors in muscles and joints to maintain balance. When one of these systems becomes impaired after TBI, the brain struggles to compensate, creating unsteadiness and increasing fall risk. frontiersin
Post-traumatic dizziness often worsens with head movements, busy visual environments, and cognitive demands. This dizziness can trigger or worsen headaches, creating a cycle where headache and dizziness reinforce each other. The constant sense of imbalance creates anxiety and limits activities, contributing to deconditioning and further functional decline. pmc.ncbi.nlm.nih+1
Altered Sensation in the Head and Neck
Changes in sensation throughout the head and neck region are commonly experienced following a TBI. These changes can include numbness, tingling, burning sensations, or areas of increased sensitivity. The cranial nerves, which provide sensation to the face, scalp, and neck, may be damaged during trauma. matrixneurological+1
The trigeminal nerve, the largest cranial nerve, supplies sensation to most of the face and head. This nerve has three main branches that provide feeling to the forehead and eyes, the cheeks and nose, and the jaw and chin. Injury to any branch of the trigeminal nerve can create altered sensation in the corresponding region. pmc.ncbi.nlm.nih
The occipital nerves, which emerge from the upper cervical spine and travel up the back of the head to the scalp, often become irritated or compressed after neck injuries. This creates pain, numbness, or tingling in the back of the head and sometimes radiates over the top of the head toward the forehead. Occipital neuralgia, inflammation or injury to these nerves, causes sharp, shooting, electric-shock-like pains in the distribution of the nerve. physio-pedia
Neck pain and stiffness frequently accompany head symptoms after TBI, particularly when cervical spine injury occurred during the trauma. The neck muscles may go into spasm as a protective response to injury, creating sustained tension that contributes to both neck pain and headaches. Ligament injuries in the cervical spine can lead to instability and persistent pain. Intervertebral disc injuries, including herniation or bulging, may compress nerve roots and create radiating pain into the arms along with headaches. elizabethsandelmd+1
Dr. Jimenez’s integrative approach emphasizes thorough evaluation of these sensory symptoms and their relationship to neuromusculoskeletal dysfunction. His clinical observations note that addressing cervical spine dysfunction through targeted chiropractic care often improves not only neck pain but also associated headaches and sensory symptoms. The neck and head share extensive neural connections, meaning that problems in one region frequently affect the other. wilbeckchiro+4
Understanding Migraines: Causes, Symptoms, and Connection to TBI
Migraines represent more than just severe headaches—they are complex neurological events involving multiple brain systems. Understanding what happens during a migraine helps explain why they become more common after traumatic brain injury and how to manage them effectively. ncbi.nlm.nih+1
What Happens in the Brain During a Migraine
Migraines involve a cascade of neurological changes that unfold over hours or even days. The process typically begins in the brainstem and hypothalamus, brain regions that regulate pain, arousal, and autonomic functions. These areas show altered activity even before headache pain begins. migrainedisorders+1
The cortical spreading depression represents a key mechanism in migraine pathogenesis. This phenomenon involves a wave of electrical silence that spreads across the brain’s surface at a rate of 2 to 3 millimeters per minute. As this wave passes through different brain regions, it temporarily suppresses normal brain activity. When the wave affects visual areas, it creates the visual aura symptoms that some people experience. The spreading depression also triggers inflammatory responses that contribute to headache pain. migrainedisorders
The trigeminal vascular system plays a central role in generating migraine pain. The trigeminal nerve sends branches to blood vessels surrounding the brain and in the meninges. When these nerve endings become activated, they release inflammatory substances, including calcitonin gene-related peptide (CGRP), substance P, and neurokinin A. These neuropeptides cause blood vessels to dilate, increase blood flow, and trigger inflammatory responses. The combination of vascular changes and inflammation activates pain receptors, creating the throbbing headache pain characteristic of migraines. emedicine.medscape+1
Neurotransmitter imbalances contribute significantly to migraine development. Serotonin, a neurotransmitter involved in pain regulation, mood, and blood vessel control, shows abnormal levels during migraines. Serotonin levels typically drop during migraine attacks, and this decrease may trigger the cascade of events that produce headache pain. Other neurotransmitters, including dopamine, norepinephrine, and glutamate, also show altered function during migraines. emedicine.medscape+1
Migraine Triggers and Risk Factors
Migraines can be triggered by numerous factors that vary from individual to individual. Common triggers include hormonal changes, particularly fluctuations in estrogen levels that occur during menstrual cycles. Many women experience migraines specifically related to their menstrual periods. Stress and emotional tension represent frequent migraine triggers, as does the relief after stress ends. Sleep disturbances, whether too little sleep, too much sleep, or irregular sleep patterns, often precipitate migraine attacks. clevelandclinic+1
Dietary factors can trigger migraines in individuals who are susceptible to them. Common food triggers include aged cheeses, processed meats containing nitrates, chocolate, alcohol (especially red wine), and foods containing monosodium glutamate (MSG). Skipping meals or fasting can also trigger migraines in some people. Caffeine presents a paradox—regular consumption followed by sudden withdrawal can trigger migraines, but caffeine can also help treat migraine pain when taken appropriately. mayoclinic
Environmental factors, including bright lights, loud sounds, strong smells, and changes in weather or barometric pressure, trigger migraines in many people. These sensory triggers become particularly problematic for people with TBI, who already experience heightened sensory sensitivity. The combination of post-TBI sensory dysfunction and migraine susceptibility creates a situation where many everyday environmental factors can trigger debilitating headaches. nature+4
Phases of a Migraine Attack
Migraines typically progress through distinct phases, though not every person experiences all phases or experiences them in the same order. The prodrome phase occurs hours or days before the onset of headache pain. During this phase, people may notice subtle changes, including mood alterations, food cravings, increased thirst, frequent urination, or neck stiffness. These prodrome symptoms result from changes in the hypothalamus and other brain regions that precede the headache. mayoclinic+1
The aura phase, which occurs in approximately 25% to 30% of people with migraines, involves temporary neurological symptoms that typically last between 5 and 60 minutes. Visual auras are the most common and may include seeing bright spots, flashing lights, zigzag lines, or the development of blind spots in the visual field. Sensory auras cause tingling or numbness that typically starts in the hand and spreads up the arm to the face. Speech and language disturbances can occur, making it difficult to find words or speak clearly. emedicine.medscape+1
The headache phase brings the characteristic migraine pain—moderate to severe, typically pulsating or throbbing, usually affecting one side of the head. The pain often intensifies with physical activity. Nausea and vomiting commonly accompany the headache. Photophobia and phonophobia make it difficult to tolerate light and sound. Many people need to lie down in a dark, quiet room during this phase. The headache phase typically lasts 4 to 72 hours if untreated. mayoclinic
The postdrome phase follows the resolution of headache pain. People often describe feeling drained, exhausted, or as if they are “hungover” during this phase. Some experience lingering head discomfort or unusual sensations. Mood changes, difficulty concentrating, and fatigue can persist for a day or more after the headache resolves. mayoclinic
How TBI Changes Migraine Patterns
Traumatic brain injury can transform migraine patterns in several ways. People who never experienced migraines before their injury may develop new-onset migraines afterward. Those who had occasional migraines before TBI often find that their migraines become more frequent, severe, or difficult to treat after injury. The study of TBI patients shows that injury severity correlates with increased migraine risk—more severe injuries create a higher likelihood of developing post-traumatic migraines. neurology+1
The mechanisms linking TBI to altered migraine patterns involve lasting changes in brain structure and function. Inflammation in the brain can persist for months or years after the initial injury. This ongoing inflammation lowers the threshold for migraine attacks, making them easier to trigger. Damage to brain regions involved in pain processing and sensory filtering creates hypersensitivity that contributes to both more frequent migraines and heightened sensitivity to migraine triggers. nature+1
Post-traumatic migraines often prove more difficult to treat than migraines unrelated to injury. Standard migraine medications may be less effective, and patients may require combination approaches involving multiple treatment modalities. The presence of other post-TBI symptoms, including cognitive impairment, mood changes, sleep disturbances, and neck pain, complicates treatment and may interfere with recovery from migraines. pmc.ncbi.nlm.nih+1
Diagnostic Assessment and Imaging for TBI and Headaches
Proper diagnosis of traumatic brain injury and post-traumatic headaches requires a comprehensive evaluation combining clinical assessment with appropriate imaging studies. Dr. Jimenez’s dual-scope practice enables thorough diagnostic workups that address both neurological and neuromusculoskeletal aspects of patient injuries. ncbi.nlm.nih+2
Clinical Evaluation
The diagnostic process begins with a detailed history-taking. Healthcare providers need to understand the mechanism of injury—how the trauma occurred, what forces were involved, whether loss of consciousness occurred, and what symptoms developed immediately afterward. Information about symptom progression helps distinguish between the effects of acute injury and complications that develop over time.advantagehcs+1
Neurological examination assesses multiple domains of function. Mental status testing evaluates the level of consciousness, orientation, memory, and cognitive abilities. Cranial nerve examination tests the function of the twelve nerve pairs that emerge from the brain and control functions including vision, eye movements, facial sensation and movement, hearing, and swallowing. Motor examination assesses muscle strength, tone, and coordination. Sensory testing evaluates the ability to perceive touch, temperature, pain, and position sense. Reflex testing provides information about the integrity of nerve pathways. ncbi.nlm.nih
Specialized testing may include vestibular evaluation for balance problems, vision testing for visual disturbances, and cognitive screening tools to identify specific areas of impairment. Headache characteristics are carefully documented, including location, quality, intensity, duration, frequency, triggers, and associated symptoms. This information helps classify the type of headache and guide treatment selection. ncbi.nlm.nih+1
Imaging Studies
Computed tomography (CT) scans represent the first-line imaging study for acute traumatic brain injury. CT excels at detecting skull fractures, bleeding inside or around the brain, brain swelling, and other acute complications requiring immediate intervention. The speed of CT scanning makes it ideal for the emergency evaluation of head-injured patients. CT provides excellent visualization of bone structures, helping identify fractures that may contribute to ongoing symptoms. elementimaging+1
Magnetic resonance imaging (MRI) provides superior detail of brain tissue and detects injuries that may not appear on CT scans. MRI is particularly valuable for evaluating mild to moderate TBI, where CT may appear normal despite ongoing symptoms. Different MRI sequences highlight distinct tissue characteristics, enabling a comprehensive assessment of structural damage. Diffusion tensor imaging (DTI), an advanced MRI technique, can detect damage to white matter tracts—the nerve fiber bundles that connect different brain regions. This technique helps explain persistent symptoms when conventional imaging appears normal. pubmed.ncbi.nlm.nih+1
Cervical spine imaging plays an important role when neck injury accompanies head trauma. X-rays provide a basic evaluation of cervical vertebral alignment and identify obvious fractures or dislocations. CT offers more detailed bone visualization and can detect subtle fractures that are often missed on X-rays. MRI excels at showing soft tissue injuries, including ligament tears, disc herniations, and spinal cord damage. These cervical spine imaging studies help identify structural problems contributing to neck pain and cervicogenic headaches. pmc.ncbi.nlm.nih+2
Dr. Jimenez’s clinic utilizes advanced neuromusculoskeletal imaging as part of a comprehensive patient evaluation. This imaging approach examines not only the brain and skull but also the cervical spine, surrounding soft tissues, and musculoskeletal structures that may contribute to symptoms. The integration of imaging findings with clinical examination results enables an accurate diagnosis that informs treatment planning. advantagehcs+1
Functional Assessment
Beyond structural imaging, functional assessments evaluate how injuries affect daily activities and quality of life. Standardized questionnaires assess the impact of headaches, cognitive function, emotional well-being, and the ability to perform work, social, and recreational activities. These assessments provide objective measures of symptom severity, helping to track recovery progress over time. ncbi.nlm.nih
Neuropsychological testing provides a comprehensive evaluation of cognitive abilities, encompassing attention, memory, language, visual-spatial skills, and executive functions. These tests identify specific areas of impairment and help develop targeted rehabilitation strategies to address them. Serial testing over time documents cognitive recovery and helps determine readiness to return to work or other demanding activities. pubmed.ncbi.nlm.nih+2
Treatment Approaches: Integrative Medicine for TBI and Headaches
Managing traumatic brain injury and post-traumatic headaches requires comprehensive approaches that address multiple aspects of the condition. Dr. Jimenez’s integrative medicine practice in El Paso combines chiropractic care, medical management, physical rehabilitation, and complementary therapies to promote natural healing and optimal recovery. northwestfloridaphysiciansgroup+3
Chiropractic Care for Post-Traumatic Headaches and Neck Pain
Chiropractic treatment focuses on addressing neuromusculoskeletal dysfunction that contributes to pain and other symptoms. Following TBI, particularly when accompanied by whiplash or neck injury, the cervical spine often develops misalignments, restricted motion, and muscle tension that contribute to headaches. Chiropractic evaluation identifies these mechanical problems through a physical examination and a review of imaging. pubmed.ncbi.nlm.nih+3
Spinal manipulation, the hallmark of chiropractic treatment, involves applying controlled forces to joints to restore normal motion and alignment. For post-traumatic headaches, chiropractors typically focus on the cervical spine, particularly the upper cervical region, where dysfunction commonly contributes to head pain. Research supports the effectiveness of spinal manipulation for certain types of headaches, particularly tension-type and cervicogenic headaches. Evidence-based guidelines recommend chiropractic manipulation as a treatment option for adults with cervicogenic headaches. oakbrookmedicalgroup+4
Soft tissue techniques address muscle tension, trigger points, and fascial restrictions that contribute to pain and discomfort. These techniques may include massage, myofascial release, and instrument-assisted soft tissue mobilization. Releasing tight muscles and improving tissue quality helps reduce pain, improve range of motion, and support healing. drjeffreystinson+2
Dr. Jimenez’s chiropractic approach emphasizes gentle, specific adjustments tailored to each patient’s condition and tolerance. Following TBI, care must be taken to avoid aggressive treatment that could worsen symptoms. The dual medical training allows Dr. Jimenez to recognize situations where chiropractic care should be modified or delayed pending further medical evaluation. northwestfloridaphysiciansgroup+1
Exercise Therapy and Physical Rehabilitation
Exercise therapy plays a crucial role in the recovery from TBI. Research demonstrates that appropriate exercise can enhance neuroplasticity—the brain’s ability to reorganize and form new neural connections. This neuroplasticity represents the foundation for recovery, allowing undamaged brain regions to compensate for injured areas. pmc.ncbi.nlm.nih+3
Aerobic exercise provides multiple benefits for people recovering from TBI. Cardiovascular activity increases blood flow to the brain, delivering oxygen and nutrients needed for healing. Exercise stimulates the release of brain-derived neurotrophic factor (BDNF), a protein that supports neuron survival and growth. Regular aerobic exercise can help reduce headache frequency and intensity, while also improving mood, sleep, and cognitive function. flintrehab+2
Strength training helps restore muscle function that may have declined during the acute injury phase. Building strength in the neck and shoulder muscles provides better support for the cervical spine, reducing mechanical stress that contributes to cervicogenic headaches. Core strengthening improves posture and reduces compensatory muscle tension. rehabpartners+1
Balance and coordination exercises help address vestibular dysfunction and reduce the risk of falls. These exercises typically begin with simple activities and progress to more challenging tasks as abilities improve. Vestibular rehabilitation specifically targets the balance system through exercises that retrain the brain to process vestibular information correctly. physio-pedia+2
Cognitive exercises help restore mental functions affected by TBI. These activities challenge attention, memory, processing speed, and executive functions in a progressive and structured manner. The principle of neuroplasticity applies to cognitive recovery—repeatedly practicing specific mental tasks strengthens the neural pathways supporting those abilities. psychiatrictimes+3
Dr. Jimenez’s clinic incorporates targeted exercise programs as a central component of rehabilitation. Exercise prescriptions are tailored to each patient’s specific impairments, functional goals, and symptom tolerance. The programs typically start conservatively and progress gradually, respecting the principle that excessive exertion can worsen post-traumatic symptoms, particularly headaches. flintrehab+2
Massage Therapy for Pain Relief and Healing
Massage therapy offers multiple benefits for people recovering from traumatic injuries. Therapeutic massage reduces muscle tension, improves circulation, decreases pain, and promotes relaxation. These effects make massage particularly valuable for managing post-traumatic headaches, especially tension-type and cervicogenic headaches linked to muscle dysfunction.excelsiainjurycare+2
The mechanisms through which massage therapy provides benefits involve both local and systemic effects. Locally, massage increases blood flow to treated tissues, delivering oxygen and nutrients while removing metabolic waste products. Massage helps release trigger points—hyperirritable spots in muscle tissue that create local and referred pain. Breaking up fascial adhesions and scar tissue improves tissue mobility and reduces pain.news.harvard+2
Systemically, massage therapy influences the nervous system in ways that reduce pain perception and promote healing. Massage activates sensory receptors that send signals to the spinal cord, where they can inhibit pain signals from reaching the brain. This mechanism, sometimes referred to as “closing the gate,” helps explain how massage therapy provides pain relief. Massage also triggers the release of endorphins, the body’s natural pain-relieving chemicals. multicaremedicalcenters+1
Research demonstrates that massage therapy accelerates muscle healing after injury. Studies show that massage reduces inflammation in injured muscles while promoting the development of new mitochondria—the cellular structures responsible for producing energy. These effects translate to faster recovery and stronger healed tissue. news.harvard
For TBI patients, massage therapy addresses both direct head and neck injuries and secondary muscle tension that develops as the body compensates for pain and dysfunction. The relaxation effects of massage help reduce stress and anxiety, which commonly worsen after TBI and can trigger or intensify headaches. Many patients report improved sleep quality after massage therapy, and better sleep supports overall healing. lhphysicaltherapy+3
Dr. Jimenez’s integrative approach includes massage therapy as part of comprehensive treatment plans. Licensed massage therapists work in coordination with other healthcare providers to address soft tissue dysfunction that contributes to patient symptoms. Treatment frequency and techniques are adjusted according to the patient’s response and treatment goals. dominguezinjurycenters+2
Acupuncture for Neurological Recovery
Acupuncture, a component of traditional Chinese medicine, involves inserting thin needles into specific points on the body to influence health and healing. Growing research evidence supports acupuncture’s effectiveness for treating various conditions related to TBI, including headaches, pain, cognitive impairment, and emotional disturbances. iamdesignedtoheal+1
Multiple mechanisms appear to mediate the effects of acupuncture on the nervous system. Acupuncture stimulation influences neurotransmitter levels, including the increase of serotonin and endorphins that help regulate pain and mood. Functional brain imaging studies demonstrate that acupuncture modulates activity in brain regions associated with pain processing, emotional regulation, and sensory integration. These changes help explain how acupuncture can reduce pain, improve mood, and enhance cognitive function. pmc.ncbi.nlm.nih+1
For TBI specifically, research suggests that acupuncture may promote neurological recovery through several pathways. Acupuncture appears to reduce neuroinflammation, a type of brain inflammation that persists after injury and contributes to ongoing symptoms. Studies in animal models demonstrate that acupuncture can enhance neuroplasticity, supporting the brain’s natural healing processes. Acupuncture also improves cerebral blood flow, ensuring adequate oxygen and nutrient delivery to healing brain tissue. pmc.ncbi.nlm.nih
Clinical studies report positive outcomes when acupuncture is incorporated into TBI rehabilitation programs. Patients receiving acupuncture show improvements in consciousness levels, cognitive function, motor abilities, and quality of life compared to those receiving standard care alone. For post-traumatic headaches, acupuncture demonstrates effectiveness comparable to or exceeding conventional treatments, often with fewer side effects. iamdesignedtoheal+1
Acupuncture treatment for TBI typically involves multiple sessions over weeks or months. Specific acupuncture points are selected based on the patient’s symptoms and treatment goals. The treatment is generally safe when performed by qualified practitioners, with minimal risk of adverse effects. iamdesignedtoheal+1
Dr. Jimenez’s clinic offers acupuncture as part of integrated treatment protocols for TBI and post-traumatic headaches. The combination of acupuncture with chiropractic care, exercise therapy, and massage therapy provides comprehensive support for healing and symptom management. This multimodal approach addresses injury causes through multiple pathways, enhancing overall treatment effectiveness. dominguezinjurycenters+1
Chiropractic Care for Healing After Trauma- Video
Managing Injury Cases: Documentation and Coordinated Care
Traumatic brain injuries often occur in contexts requiring careful documentation and coordination between healthcare providers, employers, insurance companies, and legal professionals. Dr. Jimenez’s practice handles injuries from multiple sources and provides comprehensive medical and legal documentation needed for these cases. gbw+4
Work-Related Injuries
Workplace injuries, including those causing TBI, require specific procedures and documentation. Employers must provide workers’ compensation coverage that pays for medical treatment and lost wages resulting from work-related injuries. Proper documentation establishes that the injury occurred at work and defines the scope of medical treatment needed. koszdin+2
Immediate documentation begins at the time of injury. Employees should report injuries to their supervisor as soon as possible, providing details about how the injury occurred. Employers must complete incident reports that document the circumstances of the injury. Seeking prompt medical evaluation creates an official record of injuries and symptoms. jobsitecare+1
Healthcare providers treating work injuries must document the mechanism of injury, examination findings, diagnoses, treatment plans, work restrictions, and prognosis. This documentation guides workers’ compensation case management and determines which treatments receive coverage. Detailed records establish causation—the connection between workplace activities and resulting injuries. aafp+1
Dr. Jimenez’s clinic has extensive experience managing work-related injuries, including TBI from falls, struck-by accidents, and other workplace incidents. The practice provides thorough documentation meeting workers’ compensation requirements while ensuring patients receive comprehensive, evidence-based care. Clear communication with employers and case managers facilitates the appropriate authorization of treatment and planning for return to work. axiomllc+2
Sports Injuries
Athletic activities create a significant risk for traumatic brain injury, particularly in contact sports. Proper management of sports-related TBI requires expertise in both acute injury assessment and rehabilitation planning. Return-to-play decisions must strike a balance between the athlete’s desire to compete and safety considerations aimed at preventing reinjury. austinoi+2
Sports injury assessment begins with determining the severity of the injury and identifying factors that require immediate intervention. Athletes showing signs of serious TBI, including prolonged loss of consciousness, worsening symptoms, seizures, or neurological deficits, require emergency medical evaluation. For mild concussions, initial management emphasizes rest and gradual return to activities. physio-pedia+2
Rehabilitation for sports injuries follows a structured progression that gradually increases physical and cognitive demands. Athletes typically begin with gentle aerobic exercise that does not provoke symptoms, then progress through sport-specific drills, non-contact practice, and finally full-contact practice before returning to competition. Each stage should be completed without symptom recurrence before proceeding to the next stage. aspenridgephysicaltherapy+3
Documentation of sports injuries supports the provision of appropriate care and protects against premature return to play. Medical clearance from qualified healthcare providers is essential before athletes resume full participation. Some jurisdictions have laws requiring medical clearance for athletes who have sustained concussions. rehabpartners+1
Dr. Jimenez’s practice specializes in treating athletes from various sports, offering comprehensive evaluation and rehabilitation services. The clinic’s integrative approach combines medical assessment, imaging when needed, chiropractic care for associated musculoskeletal injuries, and targeted rehabilitation programs. This coordinated care supports a safe and effective return to athletic activities while minimizing the risk of reinjury. austinoi+3
Motor Vehicle Accident Injuries
Motor vehicle accidents represent a leading cause of traumatic brain injury. These incidents often combine multiple injury mechanisms, including direct head impact, rapid acceleration-deceleration forces, and whiplash-type neck injuries. The complex nature of MVA injuries requires comprehensive evaluation and treatment. cdc+3
TBI from motor vehicle accidents may not be immediately apparent. People can sustain concussions even without hitting their heads, as the rapid motion alone can injure the brain. Delayed symptom onset is common—some symptoms may not appear until hours or days after the accident. This delayed presentation highlights the importance of a thorough medical evaluation, even when initial symptoms appear minor. clevelandclinic+2
Legal and insurance considerations add complexity to MVA injury cases. Establishing the connection between the accident and resulting injuries requires detailed documentation. Medical records must describe the accident mechanism, the timing of symptom onset, examination findings, diagnostic test results, treatment provided, and any resulting functional limitations. This documentation supports insurance claims and potential legal actions. baumgartnerlawyers+3
Dr. Jimenez’s clinic regularly treats patients injured in motor vehicle accidents, providing both medical care and necessary documentation to support their claims. The practice recognizes the importance of a thorough initial evaluation to identify all injuries, including those that may not manifest immediately. Detailed records document the full scope of injuries and their impact on function. The clinic coordinates care with other specialists when needed and communicates with insurance companies and legal representatives as appropriate. njadvocates+2
Personal Injury Cases
Personal injuries from falls, assaults, or other incidents may result in TBI requiring medical treatment and potentially legal action. These cases require careful documentation linking injuries to the incident in question. Medical records provide crucial evidence establishing injury severity, necessary treatment, and prognosis. halemonico+3
A timely medical evaluation after an injury strengthens personal injury claims. Delays between injury and medical care can create questions about whether symptoms truly resulted from the incident or developed from other causes. Comprehensive initial evaluation documents all injuries and establishes the baseline from which recovery will be measured. baumgartnerlawyers+1
Ongoing documentation tracks recovery progress, treatment effectiveness, and remaining limitations. This information establishes damages—the losses and expenses resulting from the injury. Medical records that describe pain, functional limitations, treatment requirements, and the impact on daily activities support compensation claims. gbw+2
Dr. Jimenez provides a thorough medical and chiropractic evaluation for patients with personal injuries. The practice creates detailed records suitable for legal proceedings while maintaining focus on optimal patient care. Expert testimony may be provided when cases proceed to litigation, explaining injuries, treatment, and prognosis to judges and juries. njadvocates+2
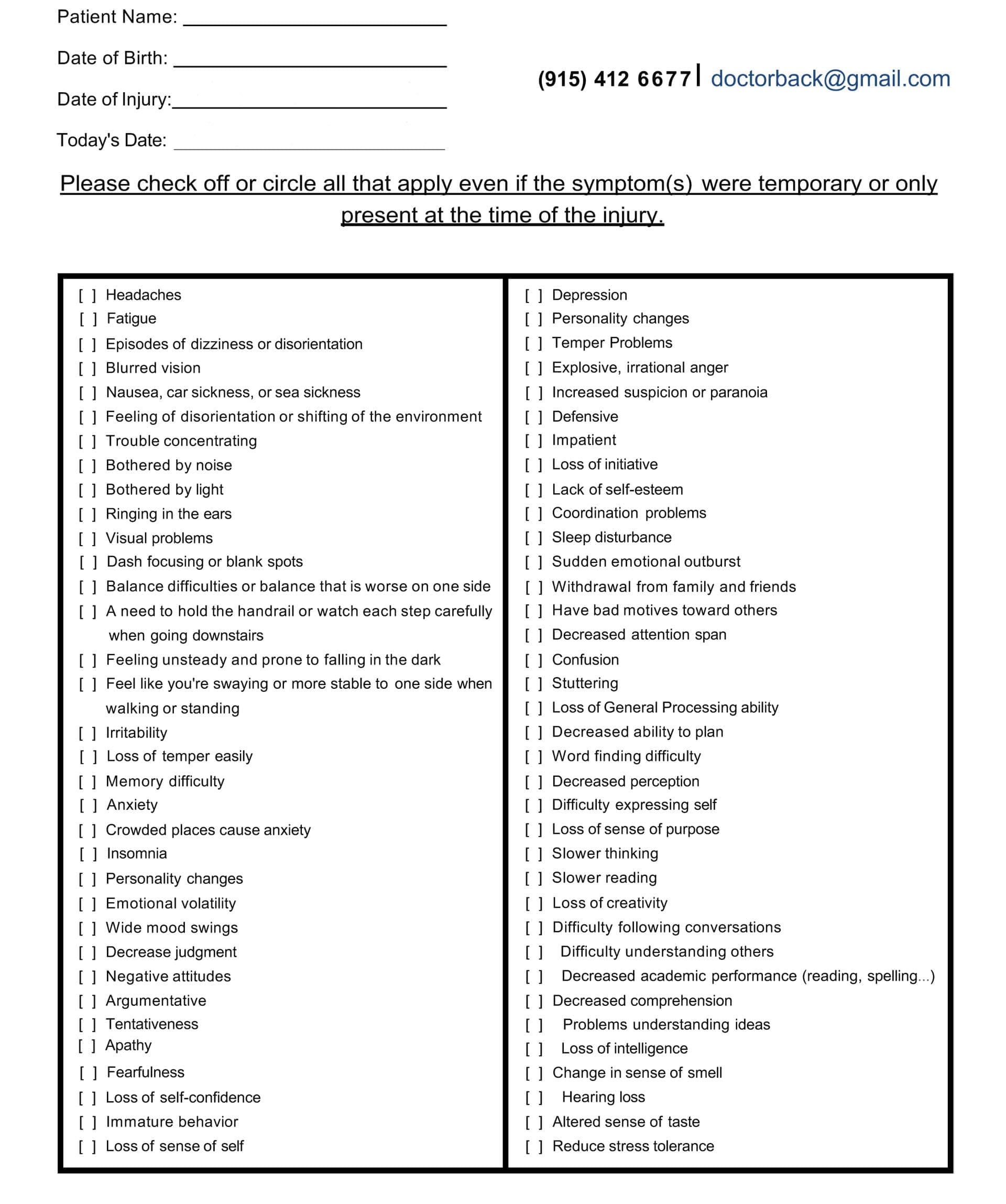
A Questionnaire Example for TBI Symptoms

Preventing Long-Term Problems Through Comprehensive Care
The integrated, patient-centered approach to TBI and post-traumatic headache management aims to prevent chronic problems that can persist for years. Early, comprehensive intervention provides the best opportunity for complete recovery. Understanding the principles that guide effective rehabilitation enables patients and their families to engage actively in the healing process. frontiersin+4
Addressing Root Causes
Effective treatment must address the underlying causes of symptoms rather than simply masking pain or other manifestations. For post-traumatic headaches, this means identifying and treating all contributing factors, including cervical spine dysfunction, muscle tension, neurological impairments, and sensory processing problems. Symptom management alone, without addressing root causes, often leads to persistent, treatment-resistant problems. traditionhealth+3
Dr. Jimenez’s diagnostic approach aims to identify all factors contributing to a patient’s symptoms. This comprehensive evaluation considers not only the direct effects of head trauma but also associated injuries to the neck, effects on posture and movement patterns, nutritional status, sleep quality, stress levels, and other factors influencing healing. Treatment plans target identified problems through appropriate interventions. traditionhealth+2
The functional medicine perspective emphasizes that optimal healing requires addressing the body’s overall health status. Nutrition provides building blocks for tissue repair and neurotransmitter production. Sleep allows the brain to clear metabolic waste products and consolidate memories. Stress management prevents the chronic activation of stress response systems, which can worsen symptoms and impair healing. Physical activity promotes neuroplasticity and cardiovascular health. This holistic view acknowledges that seemingly unrelated factors can have a significant impact on recovery from TBI. elevatewellnesschiro+2
Promoting Natural Healing
The body possesses a remarkable capacity for healing when provided with appropriate support. Neuroplasticity allows the brain to reorganize after injury, with undamaged regions developing new capabilities to compensate for lost functions. This recovery process is most effective when patients receive proper treatment and actively engage in rehabilitation. pmc.ncbi.nlm.nih+2
Chiropractic care supports natural healing by restoring normal biomechanics, reducing pain, and eliminating interference with the nervous system’s function. Manual therapy enhances joint mobility, alleviates muscle tension, and promotes healing responses. These treatments work in conjunction with the body’s inherent healing mechanisms, rather than suppressing symptoms artificially. jacksonhealingarts+3
Integrative medicine combines the best of conventional medical care with evidence-based complementary therapies. This approach recognizes that different treatment modalities offer unique benefits, and combining them often produces superior results compared to any single intervention. For TBI, this may involve using medications to manage severe symptoms while also employing chiropractic care, exercise therapy, acupuncture, and massage to address the root causes and promote healing. drestner+3
Patient Education and Empowerment
Education empowers patients to actively participate in their own recovery. Understanding their condition, what to expect during recovery, and how different treatments work helps patients make informed decisions and maintain motivation. Dr. Jimenez’s practice emphasizes patient education, ensuring people understand their diagnoses, treatment options, and self-care strategies. newmedicalchoices+2
Self-management skills are essential for long-term success. Patients learn to identify and avoid triggers that exacerbate symptoms, recognize warning signs that require medical attention, and implement strategies for managing symptoms when they occur. Activity pacing—balancing activity with rest to avoid symptom exacerbation—helps people gradually expand their functional capacity without creating setbacks. physio-pedia+2
Lifestyle modifications support healing and prevent future problems. This may include adjusting work or school schedules to accommodate cognitive limitations, modifying physical activities to reduce the risk of injury, implementing stress management techniques, improving sleep hygiene, and optimizing nutrition. These changes create an environment conducive to healing and help prevent chronic disability. elevatewellnesschiro+1
Long-Term Follow-Up and Monitoring
Recovery from TBI often takes months or years, requiring ongoing monitoring and treatment adjustment. Some symptoms resolve quickly while others persist or develop later. Regular follow-up visits enable healthcare providers to monitor progress, identify emerging issues, adjust treatments as necessary, and offer ongoing support. krwlawyers+3
Functional outcome assessment measures recovery in terms of real-world abilities, rather than relying solely on symptom checklists. Can the person return to work or school? Can they drive safely? Can they manage household responsibilities? Can they participate in social and recreational activities? These functional measures provide meaningful indicators of recovery and help identify areas needing continued intervention. krwlawyers
Preventing secondary complications represents an important aspect of long-term care. Depression, anxiety, social isolation, physical deconditioning, and chronic pain syndromes can develop after TBI, creating additional barriers to recovery. Early identification and treatment of these complications prevents them from becoming entrenched problems. mayoclinic+3
Dr. Jimenez’s practice provides continued support throughout the recovery process. The clinic’s comprehensive approach addresses not only physical symptoms but also the cognitive, emotional, and social challenges that accompany TBI. Coordination with other specialists ensures patients receive all needed services. The goal is complete recovery, allowing people to return to their previous level of function or achieve the best possible outcome given the severity of their injuries. advantagehcs
Conclusion
Traumatic brain injury creates complex challenges affecting physical, cognitive, and emotional functioning. Headaches and migraines represent some of the most common and disabling symptoms following TBI, resulting from inflammation, altered brain chemistry, sensory processing dysfunction, and associated neck injuries. Understanding how these symptoms develop and interconnect provides the foundation for effective treatment. Post-traumatic headaches take various forms, including migraine-type headaches, tension-type headaches, cervicogenic headaches, and others. Each headache type involves distinct mechanisms and responds best to targeted interventions. A comprehensive diagnostic evaluation identifies the specific factors contributing to an individual’s symptoms, enabling personalized treatment planning. The integrative medicine approach employed by Dr. Alexander Jimenez in El Paso combines chiropractic care, medical management, physical rehabilitation, massage therapy, and acupuncture to address the multifaceted aspects of TBI and its associated consequences. This coordinated, multimodal treatment strategy targets root causes rather than simply masking symptoms, promoting natural healing and preventing chronic disability.
Proper management of TBI requires not only skilled clinical care but also careful documentation, particularly for injuries occurring in work, sports, or motor vehicle accident contexts. Comprehensive medical records establish the connection between traumatic events and resulting symptoms, support insurance claims, and provide evidence in legal proceedings when necessary. Early, aggressive intervention provides the best opportunity for complete recovery from TBI. The brain’s neuroplasticity—its ability to reorganize and form new connections—represents the foundation for healing. Appropriate exercise, manual therapies, cognitive rehabilitation, and other interventions enhance neuroplasticity and support functional recovery. Patient education and empowerment facilitate active participation in the healing process, leading to improved outcomes and reduced long-term complications. Recovery from traumatic brain injury and post-traumatic headaches often requires patience and persistence. While some symptoms resolve quickly, others may persist for months or years. Comprehensive, patient-centered care addresses the full range of physical, cognitive, and emotional challenges, helping people achieve the best possible outcomes and return to meaningful, productive lives.
References
- American Brain Foundation. (2023, September 18). Common causes of brain injury. https://americanbrainfoundation.org/
- American Migraine Foundation. (2023, January 25). Tension-type headache: Symptoms, types and treatments. https://americanmigrainefoundation.org/
- Alzheimer’s Association. (2016, March 22). Traumatic brain injury | Symptoms & treatments. https://alz.org/
- Centers for Disease Control and Prevention. (2025, August 3). Facts about TBI | Traumatic brain injury & concussion. https://cdc.gov/
- Cleveland Clinic. (2025, October 19). TBI (traumatic brain injury): What it is, symptoms & treatment. https://my.clevelandclinic.org/
- Cleveland Clinic. (2025, September 25). Migraine: What it is, types, causes, symptoms & treatments. https://my.clevelandclinic.org/
- Cleveland Clinic. (2025, September 3). Cervicogenic headache: What it is, symptoms & treatment. https://my.clevelandclinic.org/
- Cleveland Clinic. (2025, June 1). Tension headache: What it is, causes, symptoms & treatment. https://my.clevelandclinic.org/
- Cleveland Clinic. (2025, September 25). Post-concussion syndrome: What it is, symptoms & treatment. https://my.clevelandclinic.org/
- Concussion Alliance. (2025, October 29). Persisting symptoms after concussion. https://concussionalliance.org/
- Connectivity. (2023, April 3). Headaches and migraines – Connectivity – Traumatic brain injury. https://connectivity.org.au/
- Connectivity. (2023, April 3). Sensitivity to light or sound – Connectivity – Traumatic brain injury. https://connectivity.org.au/
- Dominguez Injury Centers. (2025, January 21). How chiropractic care supports effective injury healing. https://dominguezinjurycenters.com/
- Dr. Alexander Jimenez. (n.d.). Injury specialists. https://dralexjimenez.com/
- Flint Rehab. (2025, July 31). Traumatic brain injury recovery exercises: 20 best TBI …. https://flintrehab.com/
- Franciscan Health. (2025, September 7). Post-concussion syndrome: Symptoms, risks and treatment. https://franciscanhealth.org/
- Frontiers in Neurology. (2023, September 13). Sensory functions and their relation to balance metrics. https://frontiersin.org/
- Headway UK. (2024, December 31). Cognitive effects of brain injury. https://headway.org.uk/
- Headway UK. (2024, December 31). Concussion. https://headway.org.uk/
- I Am Designed to Heal. (2024, December 11). How acupuncture supports recovery from traumatic brain injury (TBI). https://iamdesignedtoheal.com/
- International Classification of Headache Disorders. (2018, February 5). 5.2 Persistent headache attributed to traumatic injury to the head. https://ichd-3.org/
- JAMA Network. (2023, November 30). Profiles of cognitive functioning at 6 months after traumatic brain injury. https://jamanetwork.com/
- Mass General Brigham. (2024, March 26). What is post-concussion syndrome? https://massgeneralbrigham.org/
- Mayo Clinic. (2021, February 3). Traumatic brain injury – Symptoms & causes. https://mayoclinic.org/
- Mayo Clinic. (2025, July 7). Migraine – Symptoms and causes. https://mayoclinic.org/
- Mayo Clinic. (2023, September 25). Tension headache – Symptoms and causes. https://mayoclinic.org/
- Mayo Clinic. (2024, October 29). Persistent post-concussive symptoms (Post-concussion syndrome). https://mayoclinic.org/
- MedlinePlus. (1999, August 25). Traumatic brain injury | TBI. https://medlineplus.gov/
- Medscape. (2024, December 15). Migraine headache – Medscape reference. https://emedicine.medscape.com/
- National Institute of Neurological Disorders and Stroke. (2023, December 31). Traumatic brain injury (TBI). https://ninds.nih.gov/
- National Center for Biotechnology Information. (2023, January 8). Posttraumatic headache – StatPearls. https://ncbi.nlm.nih.gov/
- National Center for Biotechnology Information. (2024, July 4). Migraine headache – StatPearls. https://ncbi.nlm.nih.gov/
- Nature. (2022, February 8). Characterization of persistent post-traumatic headache and management. https://nature.com/
- Nature. (2019, September 24). Sensory sensitivity as a link between concussive traumatic brain injury. https://nature.com/
- Northwest Florida Physicians Group. (2025, October 30). Using chiropractic care to treat traumatic brain injuries. https://northwestfloridaphysiciansgroup.com/
- Penn Medicine. (2025, September 9). Tension headache – Symptoms and causes. https://pennmedicine.org/
- Physiopedia. (n.d.). Assessment and management of cervicogenic headaches post. https://physio-pedia.com/
- Physiopedia. (2024, December 31). Physical activity guidelines for traumatic brain injury. https://physio-pedia.com/
- Practical Neurology. (2025, November 9). Posttraumatic headache: A comprehensive approach. https://practicalneurology.com/
- Practical Neurology. (2025, November 10). Cluster headache and other trigeminal autonomic cephalalgias. https://practicalneurology.com/
- Practical Neurology. (2025, November 8). Neuroimaging traumatic brain injuries – TBI. https://practicalneurology.com/
- PubMed. (2002, January 21). Cognitive impairment following traumatic brain injury. https://pubmed.ncbi.nlm.nih.gov/
- PubMed. (2011, June 26). Evidence-based guidelines for the chiropractic treatment of adults. https://pubmed.ncbi.nlm.nih.gov/
- PubMed Central. (2016, July 25). Cervical spine involvement in mild traumatic brain injury: A review. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2013, December 31). Chronic post-traumatic headache: Clinical findings and possible. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2004, December 31). Chiropractic management of a patient with post-traumatic vertigo. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2017, January 23). Acupuncture improved neurological recovery after traumatic brain injury. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2022, May 25). Headaches in Traumatic Brain Injury: Improvement Over Time https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2023, February 14). Risk of migraine after traumatic brain injury and effects of injury. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2022, June 14). How to boost the effects of exercise to prevent traumatic brain injury. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2023, September 23). Adaptive neuroplasticity in brain injury recovery. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2016, August 9). Imaging evaluation of acute traumatic brain injury. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2013, December 23). Recovery after brain injury: Mechanisms and principles. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2011, December 31). Trigeminal autonomic cephalgias. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2016, December 31). Current concepts in sports injury rehabilitation. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2025, June 11). Deep tissue massage therapy: Effects on muscle recovery. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2011, January 7). Imaging for the diagnosis and management of traumatic brain injury. https://pmc.ncbi.nlm.nih.gov/
- PubMed Central. (2021, October 12). Post-concussion syndrome light sensitivity: A case report. https://pmc.ncbi.nlm.nih.gov/
- Queensland Brain Institute. (2024, October 22). How long does a concussion last: Long-term effects. https://qbi.uq.edu.au/
- Rehabilitation Partners. (2024, November 10). Sports Injury Rehabilitation: Techniques for a Speedy Recovery. https://rehabpartners.com/
- Sandel, E. (n.d.). Check the neck after a brain injury. https://elizabethsandelmd.com/
- Sciencedirect. (n.d.). Inflammation, brain connectivity, and neuromodulation in post. https://sciencedirect.com/
- TheraSpecs. (2025, October 19). Photophobia, light sensitivity after traumatic brain injury (TBI). https://theraspecs.com/
- Traumatic Brain Injury Model Systems. (2018, January 31). Sensory: Smell, taste, vision, hearing. https://tbi.vcu.edu/
- University of Washington. (n.d.). Cognitive problems after traumatic brain injury [PDF]. https://uwmsktc.washington.edu/
- U.S. Department of Veterans Affairs. (2018, November 28). TBI symptoms, effects & veteran support. https://mentalhealth.va.gov/
- Harvard News. (2021, October 5). Massage helps injured muscles heal more quickly and effectively. https://news.harvard.edu/
- Wilbeck Chiropractic. (2024, December 29). The benefits of chiropractic care for post-traumatic headaches. https://wilbeckchiro.com/