Hidden Traumatic Brain Injury Symptoms: Signs Missed

Hidden Traumatic Brain Injury (TBI) Symptoms: How an Integrative Chiropractic + Nurse Practitioner Team Finds What Others Miss
Overview
Many traumatic brain injuries (TBIs)—especially mild TBIs or concussions—go unnoticed at first. Symptoms can be subtle, delayed, or brushed off as stress, fatigue, or “just getting older.” A careful clinician can catch what others miss by taking a thorough patient history and asking targeted questions that explore cognitive, emotional, sensory, sleep, and balance changes. (Mayo Clinic, n.d.; BrainLine, 2017). Mayo Clinic+1
This article explains:
- A chiropractor or nurse practitioner may uncover hidden symptoms through a thorough history and structured questioning.
- Why TBIs get missed, and how to avoid that.
- A step-by-step diagnostic ladder, from basic screens to advanced tools, matched to symptom complexity.
- An integrative care plan, combining chiropractic care for the spine, neck, and vestibular system with nurse practitioner (NP) medical oversight for whole-person recovery.
We also provide clinical insights that align with the combined approach of Dr. Alexander Jimenez, DC, APRN, FNP-BC, who focuses on thorough patient history, functional exams, and gradual plans for returning to work and activities (DrAlexJimenez.com; LinkedIn). El Paso, TX Doctor Of Chiropractic+1
Why TBIs Are Easy to Miss
- Symptoms can be delayed or vague. People may notice headaches, brain fog, irritability, or sleep changes days or weeks after the event. Sensory issues such as changes in smell or taste and sensitivity to light or noise also occur, and patients often don’t connect them to a past bump, crash, or whiplash. (BrainLine, 2017; Mayo Clinic, n.d.). BrainLine+1
- Imaging can be normal. Standard CT or MRI may look fine in mild TBI, yet symptoms persist. That’s why history and examination are crucial—and why advanced tools are sometimes needed later. (Mayo Clinic, n.d.). Mayo Clinic
- Invisible wounds. Military and civilian clinicians stress that TBIs often present as “invisible injuries.” Without active screening, they are easy to overlook. (Hanscom AFB/AFMS; Health.mil). Hanscom Air Force Base+1
Hidden Symptoms To Ask About (And Why)
A skilled chiropractor or NP will conduct a thorough examination. Along with open-ended conversation, they use symptom checklists and guided probes that reveal patterns across body systems.
Cognitive and emotional
- Trouble focusing, slowed thinking, memory lapses, “losing the thread” mid-task
- Irritability, mood swings, anxiety, or depression
- Feeling “not like myself,” “foggy,” or overwhelmed in busy environments
(BrainLine, 2017). BrainLine
Sensory
- Loss or change in smell or taste
- Light/noise sensitivity; blurred vision; “seeing stars”
- Ringing in the ears (tinnitus)
(BrainLine, 2017). BrainLine
Physical
- Headaches (especially new, worsening, or “pressure-type”)
- Dizziness, vertigo, balance problems, coordination changes
- Fatigue; neck pain that worsens with screens or reading
(Mayo Clinic, n.d.; BrainLine, 2017). Mayo Clinic+1
Sleep and autonomic
- Difficulty falling or staying asleep; unusual daytime drowsiness
- Symptoms include orthostatic intolerance, which causes lightheadedness upon standing, as well as palpitations and heat or cold intolerance.
(Mayo Clinic, n.d.). Mayo Clinic
Key point: These symptoms are common after mild TBI—even with a normal CT—and they often overlap. A structured, curious interview is the quickest path to the right diagnosis. (Mayo Clinic, n.d.; Hanscom AFB). Mayo Clinic+1
The Power of a Thorough History: What to Ask
Example of Symptom Questionnaire:
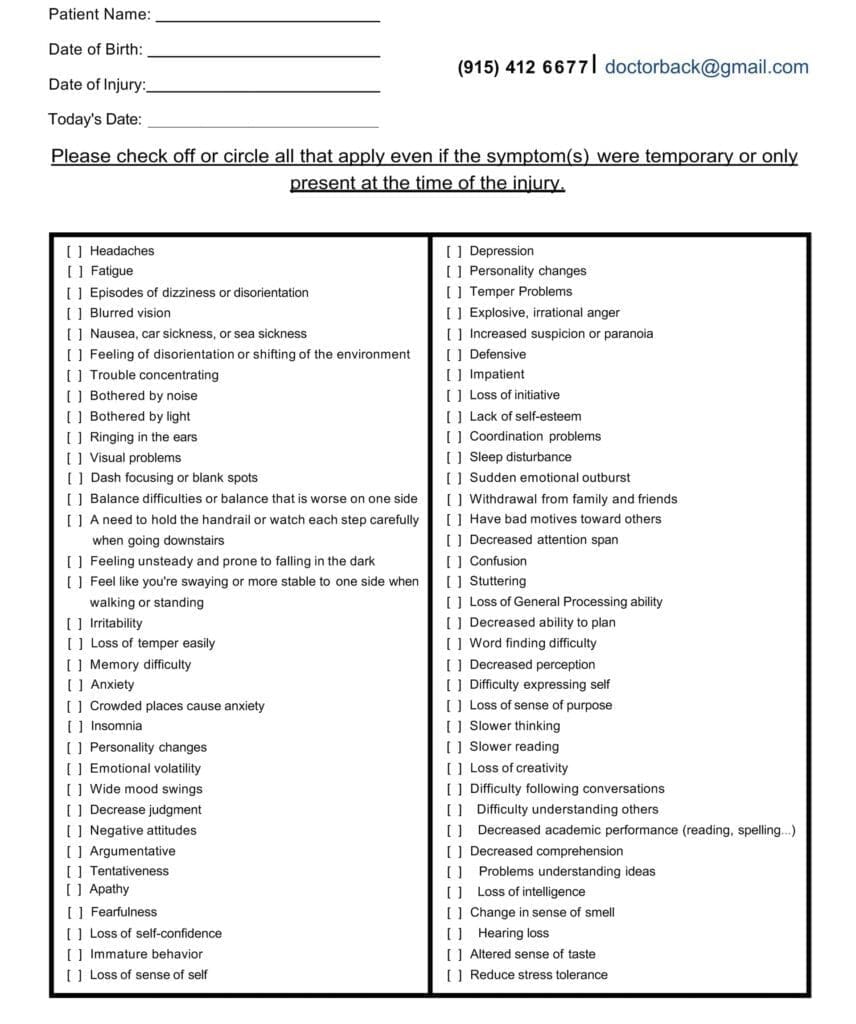
Below is a practical set of targeted questions clinicians use to uncover hidden TBI patterns. Patients and families can use this as a self-checklist to bring to appointments.
Mechanism and timeline
- What happened? (fall, car crash, sports, blast, whiplash, strike to head/neck?)
- Did you black out, feel dazed, or lose memory of events?
- When did symptoms begin—immediately, hours later, or days later? (Mayo Clinic, n.d.). Mayo Clinic
Headache and neck
- New or changing headaches? What triggers them (screens, reading, exercise, lack of sleep)?
- Neck pain or stiffness, pain during head movements, and neck fatigue throughout the day are all associated with cervicogenic headaches and vestibular problems. (Mayo Clinic, n.d.; BrainLine, 2017). Mayo Clinic+1
Cognition and mood
- Are you experiencing difficulty concentrating, slowed processing, or short-term memory slips?
- Are you experiencing irritability, mood swings, anxiety, depression, or emotional “numbness”? (BrainLine, 2017; Health.mil). BrainLine+1
Sensory
- Has there been a change in your sense of smell or taste?
- Have you noticed any new sensitivity to light or noise, experienced blurred or double vision, or experienced eye strain when reading? (BrainLine, 2017). BrainLine
Balance and dizziness
- Dizziness, vertigo, poor balance, and motion sensitivity (in a car or in a store) are common symptoms. Falls? (BrainLine, 2017). BrainLine
Sleep
- Trouble falling asleep, frequent waking, and feeling unrefreshed? (BrainLine, 2017; Mayo Clinic, n.d.). BrainLine+1
Function and safety
- Are you comfortable driving at night or at high speeds on the highway?
- Screen tolerance (work, school, phone)?
- Return to work/sport issues?
Red flags (urgent referral)
- Symptoms that require urgent referral include worsening headache, repeated vomiting, weakness or numbness, slurred speech, seizures, extreme drowsiness, new confusion, and unequal pupils. (Mayo Clinic, n.d.). Mayo Clinic
Where Chiropractic Care Fits (with NP Supervision)
Chiropractors often see patients after car crashes, sports injuries, and falls. They evaluate the cervical spine, posture, proprioception, and vestibular-ocular systems—all of which can drive headaches, dizziness, and cognitive fatigue after TBI. A growing body of interprofessional work suggests that chiropractors can play a role in screening, referral, and rehabilitative care for concussion-related neck and balance disorders, especially when working as part of a team. (NW Health/Chiropractic Economics piece; peer commentary on chiropractors’ role in SRC). Northwestern Health Sciences University+1
Nurse practitioners provide medical oversight, screen for red flags, coordinate imaging and lab tests, and manage sleep, mood, metabolic, and medication issues that often complicate recovery. Nursing literature emphasizes neuromonitoring, family education, and prevention of secondary injury, even outside the ICU. (Figueiredo et al., 2024). MDPI
A collaborative care model improves symptom tracking and coordination—especially for chronic pain and persistent symptoms after TBI. (Curran et al., 2024; Ilkhani et al., 2024). PMC+1
Clinical note (consistent with Dr. Jimenez’s approach): Combine careful history and targeted exams with staged spinal care, vestibular/oculomotor rehab, aerobic re-conditioning, and nutrition/sleep coaching—while the NP manages medical needs and coordinates imaging or biomarkers when indicated. (DrAlexJimenez.com). El Paso, TX Doctor Of Chiropractic
Diagnostic Tools for TBI: From Basic to Advanced
Think of assessment as a ladder. Start simple; climb only as needed, based on red flags, symptom persistence, and functional limits.
1) Basic bedside screening (every visit)
- Symptom scales
- PCSS (Post-Concussion Symptom Scale) – quick 22-item rating; easy to trend over time. (Intermountain Health PDF; Langevin et al., 2022). Intermountain Healthcare+1
- RPQ (Rivermead Post-Concussion Symptoms Questionnaire) – useful if scored as RPQ-3 and RPQ-13 subscales. (Eyres et al., 2005; Zeldovich et al., 2023). PubMed+1
- Sport Concussion Assessment Tool (SCAT5) – standardized sideline/clinic tool (13+ years); includes PCSS, balance, and cognitive screens. (BJSM SCAT5; BMX SCAT5). British Journal of Sports Medicine+1
- Cognitive screen
- MoCA (Montreal Cognitive Assessment) – sensitive for subtle deficits; faster and more sensitive than MMSE in TBI populations. (Waldron-Perrine et al., 2019). PMC
- Vestibular-ocular screen
- VOMS – brief test provoking symptoms with pursuits/saccades, near-point convergence, and vestibulo-ocular reflex. Highly practical after a concussion. (Mucha et al., 2014). PMC
- Balance
- BESS (Balance Error Scoring System) – simple stance tests scored by errors. (NCAA/Atrium manuals; APTA summary). fs.ncaa.org+2Atrium Health+2
- Cranial nerve + smell/taste queries
- Ask directly about smell/taste changes, and test if possible. These sensory shifts are common but under-reported. (BrainLine, 2017). BrainLine
Why this matters: Many mild TBIs won’t show on CT/MRI. These low-cost tools at the point of care catch patterns and guide next steps. (Mayo Clinic, n.d.). Mayo Clinic
2) Intermediate testing (when symptoms persist or are complex)
- Comprehensive vestibular assessment
- Videonystagmography (VNG), oculomotor testing, and computerized dynamic posturography / Sensory Organization Test (SOT) to quantify balance control and track rehab response. (UHC policy summary; RehabMeasures; related trial). UHC Provider+2Shirley Ryan AbilityLab+2
- Neurocognitive testing
- If cognitive loads (work, school, and driving) remain limited, consider using formal batteries (clinic-based or computerized). (SCAT5 framework). British Journal of Sports Medicine
- Mental health screening
- Depression, anxiety, and PTSD screens to address “invisible” sequelae early—important for prognosis and adherence. (Health.mil). Military Health System
3) Advanced diagnostics (selected cases)
- Conventional neuroimaging
- Non-contrast CT for acute red flags (rule out bleed/skull fracture).
- MRI (with appropriate sequences) if symptoms persist or focal deficits appear. (Mayo Clinic, n.d.). Mayo Clinic
- Advanced MRI sequences
- DTI (Diffusion Tensor Imaging): detects white matter microstructural changes not seen on routine MRI; can improve prognostic models in mTBI with normal CT. (Patil et al., 2025; Richter et al., 2024; Paolini et al., 2025). PMC+2The Lancet+2
- SWI (Susceptibility-Weighted Imaging): sensitive to traumatic microbleeds and diffuse axonal injury; the presence of microbleeds may relate to persistent complaints in some patients. (Hsu et al., 2023; Hageman et al., 2022; Eldeş et al., 2020). PubMed+2PubMed+2
- fMRI (task-based or resting-state): research and selected clinical programs use it to map functional disruptions after concussion. (Irimia et al., 2015; Jantzen et al., 2004). PMC+1
- Electrophysiology
- EEG/qEEG plays an evolving role in detecting or monitoring changes in networks associated with traumatic brain injury (TBI) and should be conducted according to professional guidelines, with interpretations placed in a clinical context. (Haneef et al., 2013; ACNS guideline, 2020; Stevens et al., 2024). PMC+2acns.org+2
- Blood biomarkers
- Blood tests for GFAP and UCH-L1 are FDA-approved to help determine whether adults with suspected mild traumatic brain injury need a CT scan, and labs are now offering these tests (JAMA Netw Open, 2024; bioMérieux press release, 2024). JAMA Network+1
Bottom line: Start with history and bedside tools. Escalate to advanced testing when symptoms persist, red flags emerge, or functional demands require precise guidance.
The Integrative Plan: Chiropractic + Nurse Practitioner
Goals
- Reduce symptoms (headache, dizziness, neck pain, cognitive fatigue).
- Restore systems (cervical, vestibular-ocular, autonomic).
- Rebuild capacity (sleep, mood, fitness, cognition).
- Return to life (drive, work/school, sports) with safe progressions.
Chiropractic care (examples)
- Cervical spine evaluation and treatment to reduce neck-driven headaches and improve proprioception—often key for balance and eye-head coordination. (NW Health/Chiropractic Economics; Denver Chiropractic overview). Northwestern Health Sciences University+1
- Vestibular and oculomotor exercises (gaze stabilization, smooth pursuits, saccades, and convergence work) were built from VOMS findings. (Mucha et al., 2014). PMC
- Soft-tissue therapy and graded mobility to decrease pain-guarding patterns and improve movement tolerance for daily tasks.
Note: Some clinics describe additional mechanisms (e.g., effects on CSF flow). Evidence for such claims varies, and treatment plans should focus on function, symptoms, and measurable gains. (Pinnacle; Apex; NorthWest Florida Physicians Group). pinnaclehealthchiro.com+2Apex Chiropractic+2
Nurse practitioner oversight
- Medical screening & safety: identify red flags; determine need for CT/MRI; manage post-traumatic headache, sleep issues, and mood symptoms. (Mayo Clinic; Figueiredo et al., 2024). Mayo Clinic+1
- Metabolic support: address blood pressure, glucose, thyroid, anemia, hydration, and nutrition that affect brain recovery; coordinate referrals. (Figueiredo et al., 2024). MDPI
- Education and pacing should guide cognitive and physical pacing, facilitate a graded return to tasks, and provide family support. (Health.mil; Figueiredo et al., 2024). Military Health System+1
Collaborative care pays off. TBI programs using team-based models show better coordination and patient-centered outcomes, especially when pain and mood complicate recovery. (Curran et al., 2024; Ilkhani et al., 2024). PMC+1
How a Thorough Approach Uncovers the Missed Diagnosis
- History finds the pattern. A patient with “new headaches and irritability” might also report loss of smell, motion sensitivity in stores, and neck stiffness—indicating strong post-concussive and cervical/vestibular involvement. (BrainLine, 2017). BrainLine
- Bedside tests confirm direction. An abnormal VOMS (symptom spikes on saccades or VOR) and BESS errors cement the vestibular-ocular target for therapy. (Mucha et al., 2014; NCAA/Atrium). PMC+1
- Escalate only when needed. If symptoms persist despite progress—or if work/sport demands are high—consider advanced MRI (DTI/SWI), qEEG, or biomarkers to refine prognosis and guide next steps. (Patil et al., 2025; Hsu et al., 2023; ACNS, 2020; JAMA, 2024). JAMA Network+3PMC+3PubMed+3
A Practical, Staged Care Roadmap
This is a general template. Your plan should be individualized based on findings and safety.
Weeks 0–2: Calm and orient
- Education on pacing, hydration, and sleep hygiene; light neck mobility; sub-symptom aerobic activity (e.g., easy walks).
- Begin cervical care and gentle vestibular/oculomotor drills if tolerated.
- NP manages headache/sleep, screens mood, and ensures no red flags. (Mayo Clinic; Figueiredo et al., 2024). Mayo Clinic+1
Weeks 2–6: Re-train systems
- Progress cervical stabilization and posture work; expand gaze stabilization and convergence tasks; add balance progressions.
- Short bouts of cognitive-physical dual tasking (e.g., reciting while walking) as symptoms allow.
- Use PCSS or RPQ weekly to track trend lines. (Intermountain PCSS; Eyres et al., 2005). Intermountain Healthcare+1
Weeks 6–12: Build capacity
- Increase aerobic exercise toward moderate intensity; integrate return-to-drive and return-to-work checklists.
- If plateaus persist, consider intermediate/advanced assessments (SOT/posturography; DTI/SWI in selected cases). (RehabMeasures SOT; Patil et al., 2025). Shirley Ryan AbilityLab+1
Beyond 12 weeks: Persistent symptoms
- Titrate therapies; address mood/sleep/autoimmune or endocrine drivers; consider collaborative pain programs. (Curran et al., 2024). PMC
Where Local Chiropractic or Functional Neurology Clinics Fit
Community clinics frequently educate patients about post-concussion care and offer combined chiropractic + vestibular/oculomotor programs under medical supervision. These clinics emphasize neck care, balance/eye-movement drills, and staged activity. (Denver Chiropractic; Calibration Chiropractic + Functional Health; HML Functional Care). Denver Integrated Spine Center+2calibrationmansfield.com+2
Clinical observation (aligned with Dr. Jimenez’s posts): Patients often report that a combined neck + vestibular/ocular approach reduces headache frequency, steadies vision, and improves stamina for work or driving. (DrAlexJimenez.com). El Paso, TX Doctor Of Chiropractic
Safety Reminders
- If you develop a worsening headache, repeated vomiting, seizure, weakness, confusion, or unequal pupils, seek emergency care immediately. (Mayo Clinic, n.d.). Mayo Clinic
- Spinal manipulation is not used in unstable injuries. Care should follow a full exam, with imaging or referrals when indicated.
Take-Home Messages
- Hidden symptoms are common after TBI. They span thinking, mood, senses, sleep, and balance. (BrainLine, 2017; Mayo Clinic, n.d.). BrainLine+1
- A thorough history and targeted questions are the most powerful diagnostic tools.
- Use a ladder of tests, from PCSS/RPQ, VOMS, BESS, and MoCA to SOT, advanced MRI (DTI/SWI), EEG/qEEG, and GFAP/UCH-L1 biomarkers, based on complexity. (Mucha et al., 2014; ACNS, 2020; JAMA, 2024; Patil et al., 2025). PMC+3PMC+3acns.org+3
- An integrative team—chiropractor + NP—covers structure, neurology, and overall health, improving safety and continuity of care. (Figueiredo et al., 2024; Curran et al., 2024). MDPI+1
References
BrainLine. (2017, December 1). Symptoms of traumatic brain injury (TBI). BrainLine
BrainLine. (2017, June 21). TBI 101: Physical symptoms. BrainLine
Curran, M. C., et al. (2024). Chronic pain after traumatic brain injury: A collaborative care intervention (TBI Care). PMC
Eyres, S., Carey, A., Gilworth, G., Neumann, V., & Tennant, A. (2005). Construct validity and reliability of the Rivermead Post-Concussion Symptoms Questionnaire (RPQ). PubMed
Figueiredo, R., Castro, C., & Fernandes, J. B. (2024). Nursing interventions to prevent secondary injury in critically ill patients with traumatic brain injury: A scoping review. Journal of Clinical Medicine, 13(8), 2396. MDPI
Haneef, Z., Levin, H., & Masel, B. (2013). Electroencephalography and quantitative EEG in mild traumatic brain injury. PMC
Hanscom Air Force Base Public Affairs. (2017, March 17). TBI recognition critical to treating invisible wounds. Hanscom Air Force Base
Health.mil. (2022, February 4). Air Force Invisible Wounds Initiative helps build a supportive culture. Military Health System
Hsu, C. C. T., et al. (2023). The current state of susceptibility-weighted imaging and its clinical applications in TBI. PubMed
Ilkhani, S., et al. (2024). Beyond surviving: A scoping review of collaborative care models to inform the future of post-discharge trauma care. PMC
Intermountain Health. (2024). Post-Concussion Symptom Scale (PCSS). Intermountain Healthcare
Irimia, A., et al. (2015). Functional neuroimaging of traumatic brain injury: Advances and clinical utility. PMC
JAMA Network Open. (2024). Papa, L., et al. Diagnostic performance of GFAP, UCH-L1, and MAP-2 for TBI evaluation. JAMA Network
Jantzen, K. J., et al. (2004). A prospective fMRI study of mild traumatic brain injury. PMC
Mayo Clinic. (n.d.). Traumatic brain injury—Symptoms & causes. Mayo Clinic
Mayo Clinic. (n.d.). Traumatic brain injury—Diagnosis & treatment. Mayo Clinic
Mucha, A., et al. (2014). Brief Vestibular/Ocular Motor Screening (VOMS). PMC
NW Health Sciences University. (2022). Chiropractic and traumatic brain injuries: Bringing value for TBI and concussion patients. Northwestern Health Sciences University
Patil, S., et al. (2025). Clinical utility of diffusion tensor imaging in sport-related concussion. PMC
Paolini, F., et al. (2025). Diffusion tensor imaging as a neurologic predictor in TBI. MDPI
Richter, S., et al. (2024). Predicting recovery in mild TBI with DTI and biomarkers. The Lancet
Shirley Ryan AbilityLab. (2013). Sensory Organization Test (SOT). Shirley Ryan AbilityLab
Sports Concussion Assessment Tool—SCAT5. (2017). Official SCAT5 form (BJSM). British Journal of Sports Medicine
Tenney, J. R., et al. (2020). American Clinical Neurophysiology Society. Use of quantitative EEG for mTBI—Practice guideline. acns.org
UHC Policy Note. (2024). Computerized dynamic posturography—Medical policy summary. UHC Provider
Zeldovich, M., et al. (2023). Factorial validity of the RPQ across languages (CENTER-TBI). SpringerOpen
Additional clinic/education sources referenced in context
- Denver Chiropractic. Mild traumatic brain injury—Can a chiropractor help?. Denver Integrated Spine Center
- Calibration Chiropractic + Functional Health. How integrative chiropractic care can help with TBIs. calibrationmansfield.com
- HML Functional Care. How chiropractic neurology supports brain healing. HML Functional Care
- Pinnacle Health Chiropractic. Six ways chiropractic care supports healing after TBI. pinnaclehealthchiro.com
- Apex Chiropractic. Benefits of chiropractic care following a TBI. Apex Chiropractic
Dr. Alexander Jimenez (clinical perspective & education)
- DrAlexJimenez.com. The importance of concussion tests for brain injury evaluation. El Paso, TX Doctor Of Chiropractic
- DrAlexJimenez.com. Blood markers could detect concussion. El Paso, TX Doctor Of Chiropractic
- Dr. Alexander Jimenez—LinkedIn profile. Professional background (DC + APRN, FNP-BC). LinkedIn
Industry update (biomarkers)
- bioMérieux. (2024, May 28). FDA 510(k) clearance of VIDAS® TBI (GFAP, UCH-L1) assay. bioMérieux Website



