ChiroMed: Traumatic Brain Injury & Posture

Traumatic Brain Injury & Posture: From Subtle Balance Changes to Abnormal Posturing — and How Integrative Chiropractic Care Can Help
Traumatic brain injuries (TBIs) can quietly change how you balance and stand, even months after a mild concussion. In the most serious cases, TBIs can trigger rigid reflex body positions called decorticate or decerebrate posturing, which are medical emergencies. These posture changes often stem from problems in how the brain uses sensory, visual, and vestibular (inner ear) signals. Neck and upper-back (cervical and upper thoracic) strain can exacerbate the problem by disrupting head-neck alignment and irritating nerves, which may worsen headaches and dizziness. An integrative plan that includes medical oversight, chiropractic adjustments, and sensory–motor therapies may help restore better alignment, reduce symptom drivers, and support safer balance over time (as part of a team approach). Mount Sinai Health System+3braininjurycanada.ca+3Brain Injury Association of America+3
Why TBIs Affect Posture
The brain’s balance triangle: vision, vestibular system, and body sense
Good balance depends on three main inputs working together: eyes (vision), the inner ear (vestibular system), and proprioception (your body’s internal sense of position). After a TBI, even a mild one, the brain may process these signals less efficiently. That can leave you feeling unsteady, dizzy, or “off,” especially during walking, turning the head, or in busy visual settings (like grocery aisles). Large groups of people with brain injuries report issues with balance, showing how common this problem can be. (Brain Injury Canada explains that balance integrates strength, vision, and inner-ear function and that balance problems are frequently reported after brain injury.) braininjurycanada.ca
Mild TBI: subtle but persistent postural-control changes
Research reviews show that after a concussion, people can have lingering deficits in postural control that routine tests sometimes miss. Nonlinear balance metrics and instrumented measures can detect differences even when symptoms appear to be improved. In other words, you might feel “almost fine,” but objective measures still pick up changes in sway, gait, or dynamic stability. PMC+1
Moderate to severe TBI: larger balance impairments
In moderate-to-severe TBI, studies document more obvious balance asymmetries and mobility limitations, which often require targeted, progressive rehab to improve safety and independence. OUP Academic
When Posture Becomes an Emergency: Abnormal Posturing
In rare but severe brain injuries, the body can assume reflex, rigid positions that signal deep brain dysfunction and require immediate medical care.
- Decorticate posturing: arms flexed toward the chest with clenched fists; legs extended and rigid. It’s a sign of serious brain damage affecting pathways in the cerebral cortex, thalamus, or upper midbrain. Call emergency services at once if you see this. (Cleveland Clinic; Mount Sinai.) Cleveland Clinic+1
- Decerebrate posturing: arms and legs extended, toes pointed down, head/neck arched backward, with rigid muscles—often linked to lower midbrain or pontine involvement. This also demands urgent care. (Cleveland Clinic; Mount Sinai.) Cleveland Clinic+1
Abnormal posturing is typically evaluated in conjunction with other signs using tools such as the Glasgow Coma Scale (GCS) during emergency assessments. NCBI
The Neck–Brain Link: How Cervical and Upper Thoracic Issues Can Worsen Symptoms
TBIs often occur with whiplash or neck strain, which can disturb joint motion, muscle tone, and head-on-neck position. In some patients, this can contribute to cervicogenic dizziness, headaches, and neck-related balance problems—especially when turning the head or maintaining upright posture. Clinical discussions from Dr. Jimenez’s team describe how cervical dysfunction and upper thoracic stiffness may aggravate dizziness and balance challenges after head/neck trauma. El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
- Dr. Jimenez, DC, APRN, FNP-BC, emphasizes that a careful examination of posture, cervical range of motion, and joint motion can reveal overlooked factors contributing to headaches and dizziness, and that progress often includes cervical stabilization and vestibular drills, alongside other care. El Paso, TX Doctor Of Chiropractic+1
What Symptoms Might You Notice?
- Feeling wobbly, light-headed, or “tilted,” especially in visually busy places
- Headaches (often starting at the neck or base of the skull), neck pain, and eye strain
- Dizziness when turning the head, rolling in bed, or after long screen time
- Fatigue, brain fog, or irritability that worsens as the day goes on
- Slower walking, shorter steps, or veering off line
These align with common post-concussion complaints (headache, dizziness, fatigue) and with mobility/balance challenges described in the brain-injury literature. PMC+1
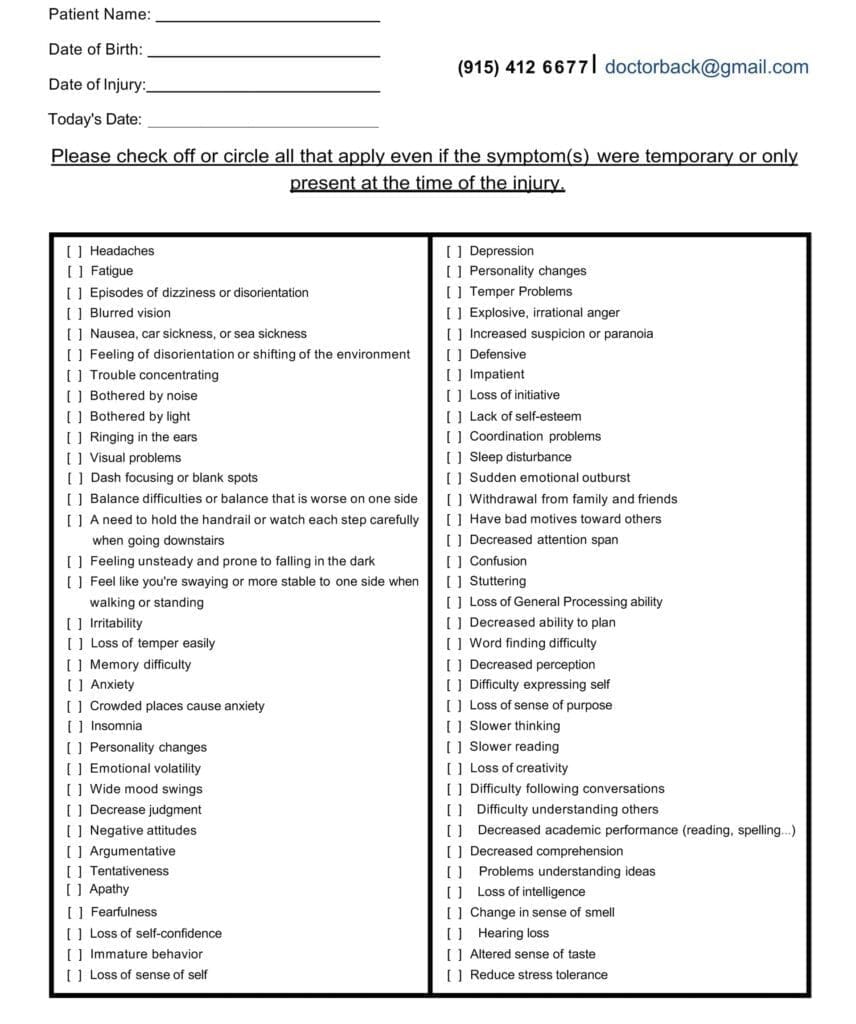
Symptom Questionnaire:
How Integrative Chiropractic Care Can Fit Into a TBI Recovery Plan
Important: Chiropractic care does not treat the brain injury itself and should not replace medical diagnosis or urgent care. It may, however, support symptom management and functional recovery when coordinated with your medical team (neurology, primary care, vestibular/physical therapy). Bergeron Clifford LLP
1) Restoring better spinal mechanics and alignment (especially upper neck)
Gentle, carefully selected spinal adjustments can reduce joint restrictions and muscle guarding in the cervical and upper thoracic regions. For some patients, improving head–neck alignment can reduce neck-related headaches and dizziness, which can indirectly improve balance and posture. Dr. Jimenez’s clinical materials and other chiropractic sources describe these goals and report symptom relief in select cases where the neck is a contributing factor. El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
2) Supporting neurophysiology and fluid dynamics (theoretical/adjunctive)
Some clinics note that adjustments may improve blood and cerebrospinal fluid (CSF) circulation, potentially aiding brain recovery by optimizing the environment around neural tissue. The evidence here is preliminary and should be framed as “may help” within a broader rehabilitation plan; still, it’s a common adjunctive rationale in clinical practice. Impact Medical Group+1
3) Sensory–motor rehabilitation to rebuild coordination
Integrative chiropractic and functional-neurology clinics often pair adjustments with targeted sensory and movement therapies: gaze stabilization, saccade/pursuit drills, balance progressions (wide base → narrow base → head turns), dual-task walking, and cervical proprioception exercises. These aim to retrain the brain (neuroplasticity) and calibrate vision–vestibular–proprioceptive inputs. HML Functional Care
4) Team-based care improves outcomes and safety
Medical guidance identifies red flags, rules out dangerous causes, and directs imaging or vestibular testing when needed. Rehabilitation professionals measure postural control, gait, and mobility using validated tools to demonstrate progress over time. Observational and review data indicate that balance changes occur after concussion, supporting the need for a structured assessment to guide rehabilitation. PMC+1
A Step-By-Step Care Pathway (What This Can Look Like)
- Medical evaluation first (especially if symptoms are new, severe, or worsening). Providers check for red flags and determine whether urgent care or imaging is necessary. Abnormal posturing = emergency. Mount Sinai Health System+1
- Baseline function check: vision, vestibular function, neck exam, simple balance tests. archives-pmr.org
- Cervical and upper thoracic care: gentle mobilization/adjustments (as appropriate), soft-tissue work, and home exercises to restore motion and reduce headache/neck-related dizziness. El Paso, TX Doctor Of Chiropractic
- Sensory–motor retraining: vestibular and oculomotor drills, graded balance tasks, gait training; progress in small, safe steps. HML Functional Care
- Lifestyle and pacing: sleep, graded activity, hydration, and symptom-paced screens/exercise—often supported by nurse-practitioner-led coaching in integrative settings. (Dr. Jimenez’s practice materials emphasize whole-person plans and steady progression.) El Paso, TX Doctor Of Chiropractic
How TBIs Can Lead to Spinal Misalignments and Symptom Flares
- Impact mechanics (falls, crashes, sports) can strain facet joints, discs, and deep neck muscles.
- The body may then adopt protective postures (chin jutting, shoulder guarding), which can irritate cervical nerves and muscle trigger points.
- These patterns may worsen headaches and dizziness by disturbing cervical proprioception and upper-neck mobility—especially around C0–C2, a frequent source of cervicogenic symptoms after whiplash/TBI. Clinical articles on cervicogenic dizziness echo these links and suggest appropriate manual care and stabilization when indicated (after medical clearance). El Paso, TX Doctor Of Chiropractic+1
When Symptoms Become “Rigid Posturing”
Remember: decorticate or decerebrate posturing means severe brain dysfunction. The person is typically unconscious and in a coma; both patterns require 911/emergency care now. (Do not attempt chiropractic or rehab; call for medical help immediately.) Cleveland Clinic+1
Tests and Tools for TBI & Postural Problems (From Simplest to Most Advanced)
Note: Your exact pathway depends on symptoms and safety. Start with medical evaluation and add tests as needed.
Bedside & Screening (simplest)
- History and neuro exam (headache, dizziness, nausea, vision changes, sleep, mood, neck pain; cranial nerves; coordination).
- Glasgow Coma Scale (GCS) in acute settings to rate eye, verbal, and motor responses. NCBI
- Symptom scales (e.g., post-concussion symptom checklists). Mayo Clinic
- Basic balance screens (Romberg, tandem stance, timed up-and-go), and observation of gait and turns.
- Cervical exam: range of motion, segmental motion, palpation, and joint position error tests for proprioception when appropriate. (Dr. Jimenez highlights posture and cervical mechanics in clinical content.) El Paso, TX Doctor Of Chiropractic
Clinic-level functional tests
- BESS (Balance Error Scoring System) and instrumented postural sway for more sensitive detection of balance deficits after concussion. PMC
- Community Balance & Mobility Scale (CB&M) for higher-level balance and mobility challenges (validated in brain injury populations). PMC
- Vestibular/Oculomotor screening (e.g., smooth pursuit, saccades, vestibulo-ocular reflex/gaze stabilization, visual motion sensitivity).
- Cervical/vestibular differentiation tests (to help sort inner-ear vs. neck-driven dizziness).
Specialized vestibular & ocular testing
- Videonystagmography (VNG), calorics, rotary chair, and dynamic visual acuity tests to quantify vestibular deficits.
- Eye-tracking or computerized oculomotor measures for pursuit/saccades.
- Computerized posturography/force-plate is utilized for objective sway and strategy analysis, while center-of-mass measures aid in characterizing dynamic postural control following a concussion. IJSPT
Neurocognitive assessment
- Standardized tests of attention, processing speed, memory, and executive function are used in concussion management (clinic-dependent).
Imaging & electrophysiology (advanced)
- CT (acute bleed/fracture) and MRI (structural injury).
- Diffusion Tensor Imaging (DTI) (white-matter pathways) and functional MRI in research/selected clinical contexts.
- EEG if seizures or atypical episodes are suspected. (Mount Sinai lists EEG among tests for abnormal posturing workups; emergency pathways decide timing.) Mount Sinai Health System+1
- PET/SPECT in select specialty centers; blood biomarkers (e.g., GFAP, UCH-L1) may be used in emergency algorithms.
Evidence Snapshots: What Research and Clinical Sources Say
- Postural control can remain impaired after concussion; sophisticated metrics can reveal deficits not obvious on quick screens. PMC
- Dynamic postural control, as measured by center-of-mass, is a useful outcome within one year post-concussion. IJSPT
- Balance limitations after TBI are common and affect independence; better sitting balance early in rehab predicts better self-care after discharge. Brain Injury Association of America
- Cervicogenic dizziness and neck-related headache can follow whiplash/head trauma; carefully managed manual therapy and cervical stabilization may reduce symptom drivers. (Clinical sources, including Dr. Jimenez’s site.) El Paso, TX Doctor Of Chiropractic+1
- Chiropractic care should be adjunctive—not a replacement for medical treatment—and may help selected patients as part of a team plan, especially when cervical dysfunction contributes to symptoms. Bergeron Clifford LLP
- Some clinics suggest that adjustments may help with blood and cerebrospinal fluid flow; however, this idea remains a theory and should be clearly explained to patients and used as part of a medically supervised plan. Impact Medical Group+1
A Practical, Integrated Plan (Example)
Built around safety, simplicity, and steady progress—and coordinated with your medical team.
- Protect & screen: See a clinician first. Urgent signs (worsening severe headache, repeated vomiting, loss of consciousness, new weakness/vision loss, abnormal posturing) need emergency care. Mount Sinai Health System+1
- Calm the neck: Gentle manual therapy and mobility work for the cervical/upper thoracic regions to reduce joint restriction and muscle guarding. Add home drills (chin nods, scapular setting, breathing) and progress slowly. El Paso, TX Doctor Of Chiropractic
- Recalibrate balance systems: Start with a wide-base stance, eyes open → eyes closed; then narrow base; then add head turns and dual-task steps. Integrate gaze stabilization (VOR) and visual motion tolerance exercises as symptoms allow. HML Functional Care
- Train real-life tasks: Gentle walking on level ground → turns → uneven terrain; keep sessions short and frequent. Measure progress with CB&M or instrumented sway when available. PMC
- Whole-person support: Sleep regularity, hydration, anti-inflammatory nutrition, and pacing (breaks between screens/reading). Clinics like Dr. Jimenez’s emphasize collaborative care—chiropractic care, nurse practitioner oversight, and vestibular/physical therapy—ensuring each domain is covered. El Paso, TX Doctor Of Chiropractic
When to Call Right Away (Red Flags)
- Abnormal posturing (decorticate/decerebrate), severe confusion, or unresponsiveness
- Worsening severe headache, repeated vomiting, seizures, new weakness/numbness, or vision loss
- Neck pain with fever, sudden stiff neck, or neurological deficits
These signs need emergency evaluation—not clinic-based care. Mount Sinai Health System+1
How Dr. Alexander Jimenez’s Team Applies This Locally (El Paso)
Dr. Jimenez, DC, APRN, FNP-BC, highlights a dual-scope approach: identifying cervical drivers of headache/dizziness, rebuilding posture with gentle adjustments and stabilization, and combining this with vestibular drills, balance progressions, and lifestyle support. His clinical articles emphasize the importance of careful posture and cervical motion exams, stepwise progress, and collaborative plans with medical and rehabilitation partners. El Paso, TX Doctor Of Chiropractic+1
The Bottom Line
- Mild TBI can leave behind subtle balance problems; severe TBI can cause abnormal posturing—an emergency. PMC+2Cleveland Clinic+2
- These changes stem from how the brain integrates vision, vestibular input, and body sense, and they can be worsened by neck/upper-back dysfunction. braininjurycanada.ca+1
- Integrative care—encompassing medical oversight, targeted chiropractic adjustments for cervical mechanics, and sensory–motor rehabilitation—offers a practical path to safer posture and stability. HML Functional Care+1
References
Brain Injury Association of America. (n.d.). [Factors associated with sitting and standing balance]. https://biausa.org/ Brain Injury Association of America
Brain Injury Association of America. (n.d.). [Sitting balance in rehabilitation is a good predictor of the amount of assistance that will be required]. https://biausa.org/ Brain Injury Association of America
Brain Injury Canada. (n.d.). [Balance]. https://braininjurycanada.ca/ braininjurycanada.ca
Brain Injury Canada. (n.d.). [Mobility]. https://braininjurycanada.ca/ braininjurycanada.ca
Cleveland Clinic. (2023, May 9). [Decerebrate posturing: What it is, causes, & treatment]. https://my.clevelandclinic.org/ Cleveland Clinic
Cleveland Clinic. (2023, May 9). [Decorticate posturing: What it is, causes, & treatment]. https://my.clevelandclinic.org/ Cleveland Clinic
Inness, E. L., et al. (2011). [Measuring balance and mobility after traumatic brain injury: Validation of the Community Balance and Mobility Scale (CB&M)]. Journal of Neurosurgery, 114(6). https://pmc.ncbi.nlm.nih.gov/ PMC
Mount Sinai Health Library. (2025, Apr 16). [Decerebrate posture]. https://www.mountsinai.org/ Mount Sinai Health System
Mount Sinai Health Library. (2025, Apr 16). [Decorticate posture]. https://www.mountsinai.org/ Mount Sinai Health System
Patejak, S., et al. (2021). [A systematic review of center of mass as a measure of dynamic postural control following concussion]. International Journal of Sports Physical Therapy. https://ijspt.scholasticahq.com/ IJSPT
Permenter, C. M., et al. (2023). [Postconcussive syndrome]. StatPearls. https://www.ncbi.nlm.nih.gov/books/ NCBI
Sosnoff, J. J., et al. (2011). [Previous mild traumatic brain injury and postural-control dynamics]. Journal of Athletic Training. https://pmc.ncbi.nlm.nih.gov/ PMC
Buckley, T. A., et al. (2016). [Postural control deficits identify lingering post-concussion neurological deficits]. Journal of Athletic Training. https://pmc.ncbi.nlm.nih.gov/ PMC
Jain, S., et al. (2023). [Glasgow Coma Scale]. StatPearls. https://www.ncbi.nlm.nih.gov/books/ NCBI
Flint Rehab. (2021). [Posturing after brain injury: Types and recovery outlook]. https://www.flintrehab.com/ Flint Rehab
HML Functional Care. (2025, Jul 22). [How chiropractic neurology supports brain healing]. https://hmlfunctionalcare.com/ HML Functional Care
Impact Medical Group. (2024, Jun 26). [Can chiropractic care help with mild traumatic brain injuries?] https://www.impactmedicalgroup.com/ Impact Medical Group
Northwest Florida Physicians Group. (2025). [Using chiropractic care to treat traumatic brain injuries]. https://northwestfloridaphysiciansgroup.com/ Northwest Florida Physicians Group
Pinnacle Health Chiropractic. (2025). [Six ways chiropractic care supports healing after TBI]. https://www.pinnaclehealthchiro.com/ pinnaclehealthchiro.com
ThinkVida. (2025). [Treating concussions with chiropractic care]. https://thinkvida.com/ Vida Integrated Health
Jimenez, A. (n.d.). [Finding hidden TBI symptoms: Signs you might miss]. dralexjimenez.com. https://dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Jimenez, A. (n.d.). [Neck pain and feeling dizzy: Cervicogenic/cervical vertigo]. dralexjimenez.com. https://dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Jimenez, A. (n.d.). [Cervicogenic dizziness from whiplash]. dralexjimenez.com. https://dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Jimenez, A. (2025). [Traumatic brain injury: Understanding the long-term effects]. dralexjimenez.com. https://dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Post Disclaimer
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "ChiroMed: Traumatic Brain Injury & Posture" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and facilitate clinical collaboration with specialists across disciplines. Each specialist is governed by their professional scope of practice and licensure jurisdiction. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRN: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card