Clinical Approach Solutions to Manage Opioid Use Disorder
Unveil the clinical approach to opioid use disorder and learn about evidence-based methods for effective treatment.
Overcoming Barriers in Managing Opioid Use Disorder: Strategies for Effective Care
A lot of people today have opioid use disorder (OUD), which is a serious health problem. It falls under the larger group of substance use disorders (SUD). Treating OUD can be difficult because everyone has their own set of problems, like pain or other health issues. Doctors and other healthcare professionals must make plans that are specific to each patient. They also need to stay up to date on laws, ethics, and ways to protect patient information. The Health Insurance Portability and Accountability Act (HIPAA) of 1996 covers all patients, but those getting treatment for drug or alcohol abuse have to follow more rules.
In this tutorial, we talk about how to get around problems with OUD administration. We look at stigma, team-based approaches, ways to talk to patients, treatment that puts the patient first, and legal issues. Health care workers can help patients get better by using these methods. Keywords like “opioid use disorder management,” “overcoming stigma in OUD,” and “patient-centered care for SUD” highlight important ideas to help people understand better and find what they’re looking for.
Learning Objectives
- Explain treatment planning methods that use patient-focused choices and proven ways to talk.
- Name the three kinds of stigma and how they affect people with mental health issues, SUD, and especially OUD.
- Talk about legal, ethical, and privacy concerns in caring for people with OUD.
Effective Treatment Planning with Patient-Centered Decisions
People with complex issues, like mental health problems, SUD, and pain, need special care. Each person shows up differently, so health systems are now focusing on care that puts the patient first.
Patient-centered care means building teams with doctors, patients, and families. They work together to plan, give, and check health care. This way ensures the patient’s needs are met, and their wishes, likes, and family situations are respected. It focuses on shared choices about treatments while seeing the patient as a whole person in their daily life (Dwamena et al., 2012; Bokhour et al., 2018).
Studies show key steps for a good patient-centered plan:
- Take a full patient history and a check-up, reviewing old and new treatments.
- Find all available drug and non-drug options.
- Check the patient’s current health, recent changes, and patterns.
- Look at risks for misusing or abusing opioids.
If starting opioids or if the patient is already on them, think about opioid stewardship. This means checking harms, benefits, risks, side effects, pain control, daily function, drug tests, stop plans, and ways to spot OUD. These programs, sometimes called analgesia stewardship, help manage opioids safely (Harle et al., 2019; Coffin et al., 2022). Guides exist to set them up (American Hospital Association, n.d.; Shrestha et al., 2023).
Integrative chiropractic care can play a big role here. It uses spinal adjustments and targeted exercises to get proper spinal alignment. This helps reduce pain without relying only on drugs, making it a good fit for OUD patients with pain. For example, adjustments fix spine issues that cause pain, and exercises strengthen muscles to keep alignment right.
A Nurse Practitioner (NP) adds full management and ergonomic advice. They look at work setups to prevent pain, such as how to sit or lift. NPs coordinate care by reviewing options such as therapy, meds, and lifestyle changes, ensuring everything works together.
Dr. Alexander Jimenez, DC, APRN, FNP-BC, with over 30 years in chiropractic and as a family nurse practitioner, observes that blending these methods cuts opioid use. At his El Paso clinic, he uses functional medicine to address root causes through nutrition and non-invasive treatments. He notes that poor posture from modern life worsens pain, leading to OUD risks. His teams help patients with self-massage and VR for recovery, reducing drug needs (Jimenez, n.d.a; Jimenez, n.d.b).
Evidence-Based Ways to Communicate
Good talking skills are key to building a patient-centered plan (Schaefer & Block, 2009). There are proven methods for starting conversations and getting patients involved.
One method is BATHE:
- Background: Ask, “How have things been since your last visit?”
- Affect: Ask, “How does this make you feel?”
- Trouble: Ask, “What bothers you most?”
- Handling: Ask, “How are you coping?”
- Empathy: Say, “That sounds hard.”
This uses open questions to let patients lead and feel supported (Stuart & Lieberman, 2018; Thomas et al., 2019).
Another is GREAT:
- Greetings/Goals: Start with hello and set aims.
- Rapport: Build trust.
- Evaluation/Expectation/Examination/Explanation: Check and explain.
- Ask/Answer/Acknowledge: Listen and respond.
- Tacit agreement/Thanks: Agree and thank.
This guide talks well (Brindley et al., 2014).
Motivational interviewing is also useful. It’s a team-style talk to boost a patient’s desire to change. Build a bond, focus on the issue, spark a desire for change, and plan steps (Frost et al., 2018).
These methods emphasize listening, clear communication, and a structured approach to planning. For OUD patients with pain or mental issues, mix techniques for the best results.
Dr. Jimenez shares that in his practice, these talks help patients see non-drug options, such as chiropractic adjustments. He finds that empathy reduces stigma and fear, encouraging openness about OUD (Jimenez, n.d.a).
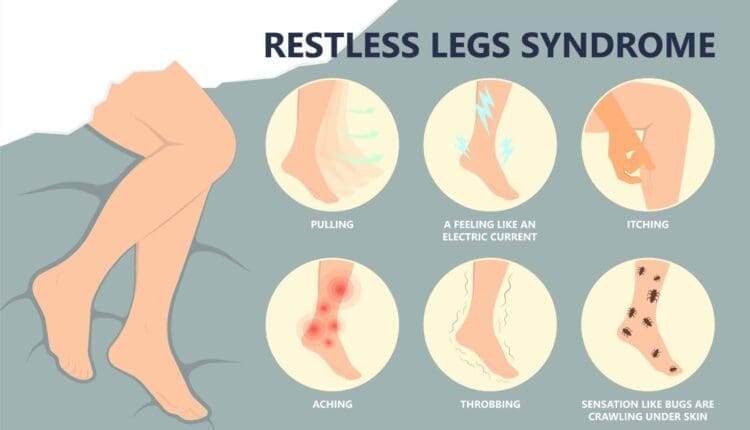
Understanding Stigma in Mental Health and Substance Use Disorders
Stigma blocks good talk for many with mental health or SUD. It’s attitudes, beliefs, actions, and systems that lead to unfair views and bad treatment (Cheetham et al., 2022).
Studies show stigmas like linking mental illness to violence (Perry, 2011). Media on shootings with mentally ill people strengthens this (McGinty et al., 2014; McGinty et al., 2016; Schomerus et al., 2022). For SUD, people think they’re more dangerous than those with schizophrenia or depression (Schomerus et al., 2011). Society blames people with SUDs more and avoids them (McGinty et al., 2015; Corrigan et al., 2012).
Views come from knowledge, contact with affected people, and the media. Public ideas are tied to norms on causes, blame, and danger. Race, ethnicity, and culture shape attitudes too (Giacco et al., 2014).
Health workers have biases. A survey of VA mental health providers showed awareness of race issues but avoidance of talks, using codes like “urban,” and thinking training stops racism (McMaster et al., 2021).
There are three stigma types:
- Structural Stigma: The ways Society and institutions keep prejudice. In health, it’s worse care, less access to behavioral health. Less funding for mental vs. physical issues (National Academies of Sciences, Engineering, and Medicine, 2016).
- Public Stigma: General or group attitudes, like police or church norms. Laws reinforce it, like broad mental illness rules implying all are unfit (Corrigan & Shapiro, 2010).
- Self-Stigma: When people internalize stigmas, it leads to low self-worth and shame. “Why try” affects independent living (Corrigan et al., 2009; Clement et al., 2015).
Dr. Jimenez observes that stigma makes OUD patients hide symptoms, delaying care. In his integrative work, he addresses this through education on holistic options, showing that recovery is possible without judgment (Jimenez, n.d.b).
Overcoming Stigma and Addressing Social Factors
To fight stigma, use education, behavior changes, and better care. Laws like the ADA and MHPAEA help ensure equal coverage and prevent discrimination (U.S. Congress, 2009; U.S. Congress, 2008; U.S. Department of Health and Human Services, n.d.; Busch & Barry, 2008; Haffajee et al., 2019).
These address social determinants of health (SDOH), such as coverage, access, quality, education, and stability (Centers for Disease Control and Prevention, n.d.).
Community programs help too:
- West Virginia’s Jobs and Hope: Training, jobs, education, transport, skills, record clearing for SUD people (Jobs and Hope, n.d.).
- Belden’s Pathway: Rehab for failed drug tests, leading to jobs (Belden, n.d.).
Education boosts provider confidence in OUD meds, reducing barriers (Adzrago et al., 2022; Hooker et al., 2023; Campbell et al., 2021).
Overcoming stigma is key to success in mental health and SUD.
Interprofessional Team Work
Teams improve outcomes for patients with chronic pain and mental health or SUD (Joypaul et al., 2019; Gauthier et al., 2019).
Teams include doctors, nurses, NPs, pharmacists, PAs, social workers, PTs, therapists, SUD experts, and case managers.
Each helps uniquely:
- Pharmacists watch meds, spot interactions.
- Case managers link specialists, find resources, and support families (Sortedahl et al., 2018).
- Teams set goals, max non-opioid treatments (Liossi et al., 2019).
Integrative chiropractic care includes adjustments and exercises for alignment, easing pain naturally.
NPs give full care, ergonomic tips to avoid pain triggers, and coordinate options.
Dr. Jimenez’s clinic shows this. As a DC and FNP-BC, he leads teams with therapists, nutritionists, and coaches. He observes interprofessional work cuts opioid use by addressing the roots with functional medicine, VR, and nutrition. For OUD, he blends chiropractic care for pain, NP coordination for plans, and stigma-fighting through team support (Jimenez, n.d.a; Jimenez, n.d.b).
The Power of Chiropractic Care in Injury Rehabilitation-Video
Legal and Ethical Issues in SUD Care
Providers must know laws and ethics for mental/SUD patients, like discrimination, aid, and privacy (Center for Substance Abuse Treatment, 2000).
Key Federal laws:
- Americans with Disabilities Act (ADA) of 1990.
- Rehabilitation Act of 1973.
- Workforce Investment Act of 1998.
- Drug-Free Workplace Act of 1988.
ADA and Rehabilitation ban discrimination in government and in business services like hotels, shops, and hospitals. Protect those with impairments limiting life activities (U.S. Department of Health and Human Services, n.d.).
Provisions:
- Protect “qualified” people who meet the requirements.
- Reasonable accommodations for jobs.
- No hire/retain if there is a direct threat.
- No denial of benefits, access, or jobs in funded places.
For SUD: Alcohol users are protected if qualified, no threat. Ex-drug users in rehab are the same. Current illegal drug users are protected for health/rehab, not others. Programs can deny if used during.
Workforce Act centralizes job programs; no refusal to SUD people (U.S. Congress, 1998).
Drug-Free Act requires drug-free policies for federal funds/contracts: statements, awareness, actions on violations (U.S. Code, n.d.).
States have their own laws; check the local laws.
Public Aid laws:
- Contract with America Act (1996): No SSI/DI if SUD key factor (U.S. Congress, 1996).
- Adoption Act (1997): 15-month foster reunification limit (U.S. Congress, 1997).
- Personal Responsibility Act (1996): Work after 2 years of aid, drug screens (U.S. Department of Health and Human Services, 1996).
These push work, sobriety.
Dr. Jimenez notes that legal awareness helps his practice by ensuring holistic plans comply and by reducing OUD risks through a non-drug focus (Jimenez, n.d.a).
Keeping Patient Info Private
Privacy is vital. Laws include:
- HIPAA (1996): Protects PHI, sets use/disclosure rules (U.S. Department of Health and Human Services, n.d.).
- 42 CFR Part 2: Extra for SUD records. No disclosure of name or status without consent. Fines for breaks. Applies to federal-aided programs (Substance Abuse and Mental Health Services Administration, n.d.).
Consent needs: program name, receiver, patient name, purpose, info type, revoke note, expire date, signature, and date.
This fights discrimination fears, encouraging treatment (Center for Substance Abuse Treatment, 2000).
Wrapping Up
As we deal with the ongoing problems of opioid use disorder (OUD), it’s clear that the best way to handle them is through a multi-faceted approach that puts the health of the patient first instead of quick fixes. Healthcare providers are essential to changing lives. They do this by supporting patient-centered decision-making and evidence-based communication, and by breaking down the three types of stigma—structural, public, and self—that make it harder for people to get better. Legal and ethical frameworks, such as HIPAA and 42 CFR Part 2 privacy protections, make sure that people who need help can get it without worrying about being treated unfairly. Interprofessional teams also help make sure that everyone receives the care they need.
Chiropractic care, which focuses on spinal adjustments and specific exercises to help with proper alignment, is a non-invasive way to ease pain and cut down on the need for opioids. Nurse Practitioners (NPs) improve this by offering comprehensive care, ergonomic advice to avoid injury, and the coordination of various treatment options, including therapy and lifestyle changes. Dr. Alexander Jimenez, DC, APRN, FNP-BC, stresses in his clinical practice that these integrative methods not only help with physical symptoms but also give patients the tools they need to make educated decisions and follow personalized plans. This leads to long-term recovery and less use of opioids (Jimenez, n.d.a; Jimenez, n.d.b).
Recent developments in OUD treatment as of 2025 indicate a transition towards more individualized and accessible alternatives. For example:
- FDA-approved drugs like methadone, buprenorphine, and naltrexone are still the mainstays of treatment for OUD. They help reduce cravings and withdrawal symptoms while also assisting people to stay stable over the long term.
- Precision medicine goes beyond one-size-fits-all approaches by tailoring treatments to each person’s genetic, psychological, and social factors. This should lead to better results.
- New Guideline: The World Health Organization’s 2025 updates emphasize the importance of psychosocial support alongside drug treatments. They also focus on preventing overdoses in the community and making care more widely available.
- Declining Trends: The number of deaths involving opioids dropped for the first time in 2023 since 2018, which is a good sign that ongoing efforts in policy, education, and treatment are having an effect.
We can create a future where OUD is not a life sentence but a condition that can be managed by combining these new ideas with reducing stigma and working together to care for people. Healthcare professionals, communities, and policymakers must continue to push for fair access to care so that everyone gets the compassionate, evidence-based help they need. In the end, overcoming the obstacles to managing OUD isn’t just about treatment; it’s also about restoring hope, respect, and a better quality of life.
References
- Adzrago, D., Paola, A. D., Zhu, J., et al. (2022). Association between prescribers’ perceptions of the utilization of medication for opioid use disorder and opioid dependence treatability. Healthcare, 10(9), 1733. https://doi.org/10.3390/healthcare10091733
- American Hospital Association. (n.d.). Stem the tide: Opioid stewardship measurement implementation guide. https://www.aha.org/opioids/stem-tide-addressing-opioid-epidemic-taking-action
- Belden. (n.d.). Belden’s Pathway to Employment. https://www.belden.com/about/pathways-to-employment
- Bokhour, B. G., Fix, G. M., et al. (2018). How can healthcare organizations implement patient-centered care? Examining a large-scale cultural transformation. BMC Health Services Research, 18(1), 168. https://doi.org/10.1186/s12913-018-2993-5
- Brandeis Opioid Resource Connector. (2021). Addressing the Opioid Crisis through Social Determinants of Health: What Are Communities Doing? https://opioid-resource-connector.org/sites/default/files/2021-02/Issue%20Brief%20-%20Final.pdf
- Brindley, P. G., Smith, K. E., Cardinal, P., & LeBlanc, F. (2014). Improving medical communication with patients and families: Skills for a complex (and multilingual) clinical world. Canadian Respiratory Journal, 21(2), 89-91. https://doi.org/10.1155/2014/789456
- Busch, S. H., & Barry, C. L. (2008). New evidence on the effects of state mental health mandates. Inquiry, 45(3), 308-322. https://doi.org/10.5034/inquiryjrnl_45.03.308
- Campbell, C. I., Saxon, A. J., Boudreau, D. M., et al. (2021). Primary Care Opioid Use Disorders treatment (PROUD) trial protocol: A pragmatic, cluster-randomized implementation trial in primary care for opioid use disorder treatment. Addiction Science & Clinical Practice, 16(1), 9. https://doi.org/10.1186/s13722-021-00221-1
- Centers for Disease Control and Prevention. (n.d.). Social Determinants of Health at CDC. https://www.cdc.gov/socialdeterminants/index.htm
- Center for Substance Abuse Treatment. (2000). Integrating Substance Abuse Treatment and Vocational Services. (Treatment Improvement Protocol (TIP) Series, No. 38.) Chapter 7—Legal Issues. https://www.ncbi.nlm.nih.gov/books/NBK64294/
- Center for Substance Abuse Treatment. (2000). Substance Abuse Treatment for Persons with Child Abuse and Neglect Issues. (Treatment Improvement Protocol (TIP) Series, No. 36.) Appendix B –Protecting Clients’ Privacy. https://www.ncbi.nlm.nih.gov/books/NBK64900/
- Cheetham, A., Picco, L., Barnett, A., et al. (2022). The impact of stigma on people with opioid use disorder, opioid treatment, and policy. Substance Abuse and Rehabilitation, 13, 1-12. https://doi.org/10.2147/SAR.S304256
- Clement, S., Schauman, O., Graham, T., et al. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45(1), 11-27. https://doi.org/10.1017/S0033291714000129
- Coffin, P. O., Martinez, R. S., Wylie, B., et al. (2022). Primary care management of long-term opioid therapy. Annals of Medicine, 54(1), 2451-2469. https://doi.org/10.1080/07853890.2022.2118597
- Corrigan, P. W., Larson, J. E., & Rüsch, N. (2009). Self-stigma and the “why try” effect: Impact on life goals and evidence-based practices. World Psychiatry, 8(2), 75-81. https://doi.org/10.1002/j.2051-5545.2009.tb00218.x
- Corrigan, P. W., Morris, S. B., Michaels, P. J., Rafacz, J. D., & Rüsch, N. (2012). Challenging the public stigma of mental illness: A meta-analysis of outcome studies. Psychiatric Services, 63(10), 963-973. https://doi.org/10.1176/appi.ps.201100529
- Corrigan, P. W., & Shapiro, J. R. (2010). Measuring the impact of programs that challenge the public stigma of mental illness. Clinical Psychology Review, 30(8), 907-922. https://doi.org/10.1016/j.cpr.2010.06.004
- Dwamena, F., Holmes-Rovner, M., Gaulden, C., et al. (2012). Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews, 2012(12), CD003267. https://doi.org/10.1002/14651858.CD003267.pub2
- Frost, H., Campbell, P., Maxwell, M., et al. (2018). Effectiveness of Motivational Interviewing on adult behavior change in health and social care settings: A systematic review of reviews. PLoS One, 13(10), e0204890. https://doi.org/10.1371/journal.pone.0204890
- Gauthier, K., Dulong, C., & Argáez, C. (2019). Multidisciplinary treatment programs for patients with chronic non-malignant pain: A review of clinical effectiveness, cost-effectiveness, and guidelines – an update. Canadian Agency for Drugs and Technologies in Health. https://www.ncbi.nlm.nih.gov/books/NBK545496/
- Giacco, D., Matanov, A., & Priebe, S. (2014). Providing mental healthcare to immigrants: Current challenges and new strategies. Current Opinion in Psychiatry, 27(4), 282-288. https://doi.org/10.1097/YCO.0000000000000070
- Haffajee, R. L., Mello, M. M., Zhang, F., et al. (2019). Association of federal mental health parity legislation with health care use and spending among high utilizers of services. Medical Care, 57(4), 245-255. https://doi.org/10.1097/MLR.0000000000001076
- Harle, C. A., DiIulio, J., Downs, S. M., et al. (2019). Decision-Centered design of patient information visualizations to support chronic pain care. Applied Clinical Informatics, 10(4), 719-728. https://doi.org/10.1055/s-0039-1696668
- Hooker, S. A., Crain, A. L., LaFrance, A. B., et al. (2023). A randomized controlled trial of an intervention to reduce stigma toward people with opioid use disorder among primary care clinicians. Addiction Science & Clinical Practice, 18(1), 10. https://doi.org/10.1186/s13722-023-00366-1
- Jimenez, A. (n.d.a). Dr. Alex Jimenez, DC, Injury Specialist. https://dralexjimenez.com/
- Jimenez, A. (n.d.b). Dr. Alexander Jimene,z DC, APRN, FNP-BC, IFMCP, CFMP, ATN ♛. LinkedIn. https://www.linkedin.com/in/dralexjimenez/
- Jobs and Hope. (n.d.). https://jobsandhope.wv.gov/
- Joypaul, S., Kelly, F., McMillan, S. S., et al. (2019). Multi-disciplinary interventions for chronic pain involving education: A systematic review. PLoS One, 14(10), e0223306. https://doi.org/10.1371/journal.pone.0223306
- Liossi, C., Johnstone, L., Lilley, S., et al. (2019). Effectiveness of interdisciplinary interventions in paediatric chronic pain management: A systematic review and subset meta-analysis. British Journal of Anaesthesia, 123(2), e359-e371. https://doi.org/10.1016/j.bja.2019.01.024
- McGinty, E. E., Goldman, H. H., Pescosolido, B., et al. (2015). Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Social Science & Medicine, 126, 73-85. https://doi.org/10.1016/j.socscimed.2014.12.010
- McGinty, E. E., Kennedy-Hendricks, A., Choksy, S., et al. (2016). Trends in news media coverage of mental illness in the United States: 1995-2014. Health Affairs, 35(6), 1121-1129. https://doi.org/10.1377/hlthaff.2016.0011
- McGinty, E. E., Webster, D. W., Jarlenski, M., et al. (2014). News media framing of serious mental illness and gun violence in the United States, 1997-2012. American Journal of Public Health, 104(3), 406-413. https://doi.org/10.2105/AJPH.2013.301557
- McMaster, K. J., Peeples, A. D., Schaffner, R. M., et al. (2021). Mental healthcare provider perceptions of race and racial disparity in the care of Black and White clients. Journal of Behavioral Health Services & Research, 48(4), 501-516. https://doi.org/10.1007/s11414-021-00753-3
- National Academies of Sciences, Engineering, and Medicine. (2016). Ending discrimination against people with mental and substance use disorders: The evidence for stigma change. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK384923/
- Perry, B. L. (2011). The labeling paradox: Stigma, the sick role, and social networks in mental illness. Journal of Health and Social Behavior, 52(4), 460-477. https://doi.org/10.1177/0022146511408913
- Schaefer, K. G., & Block, S. D. (2009). Physician communication with families in the ICU: Evidence-based strategies for improvement. Current Opinion in Critical Care, 15(6), 569-577. https://doi.org/10.1097/ACQ.0b013e328332af31
- Schomerus, G., Lucht, M., Holzinger, A., et al. (2011). The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol and Alcoholism, 46(2), 105-112. https://doi.org/10.1093/alcalc/agq089
- Schomerus, G., Schindler, S., Sander, C., et al. (2022). Changes in mental illness stigma over 30 years – Improvement, persistence, or deterioration? European Psychiatry, 65(1), e78. https://doi.org/10.1192/j.eurpsy.2022.2334
- Shrestha, S., Khatiwada, A. P., Sapkota, B., et al. (2023). What is “Opioid Stewardship”? An overview of current definitions and a proposal for a universally acceptable definition. Journal of Pain Research, 16, 383-394. https://doi.org/10.2147/JPR.S389785
- Sortedahl, C., Krsnak, J., Crook, M. M., et al. (2018). Case managers on the front lines of opioid epidemic response: Advocacy, education, and empowerment for users of medical and nonmedical opioids. Professional Case Management, 23(5), 256-263. https://doi.org/10.1097/NCM.0000000000000294
- Stuart, M. R., & Lieberman, J. A. (2018). The fifteen-minute hour: Efficient and effective patient-centered consultation skills (6th ed.). CRC Press. https://www.routledge.com/The-Fifteen-Minute-Hour-Efficient-and-Effective-Patient-Centered-Consultation-Skills/Stuart-Lieberman/p/book/9781138497719
- Substance Abuse and Mental Health Services Administration. (n.d.). Substance Abuse Confidentiality Regulations. https://www.samhsa.gov/about-us/who-we-are/laws-regulations/confidentiality-regulations-faqs
- Thomas, C., Cramer, H., Jackson, S., et al. (2019). Acceptability of the BATHE technique amongst GPs and frequently attending patients in primary care: A nested qualitative study. BMC Family Practice, 20(1), 121. https://doi.org/10.1186/s12875-019-1011-1
- U.S. Code. (n.d.). 41 USC Ch. 81: Drug-Free Workplace. https://uscode.house.gov/view.xhtml?path=/prelim@title41/subtitle4/chapter81&edition=prelim
- U.S. Congress. (1996). Public Law 104-121 – Contract with America Advancement Act of 1996. https://www.govinfo.gov/app/details/PLAW-104publ121
- U.S. Congress. (1997). H.R.867 – Adoption and Safe Families Act of 1997. https://www.congress.gov/bill/105th-congress/house-bill/867
- U.S. Congress. (1998). Public Law 105-220 – Workforce Investment Act of 1998. https://www.govinfo.gov/content/pkg/PLAW-105publ220/pdf/PLAW-105publ220.pdf
- U.S. Congress. (2008). S.3406 – ADA Amendments Act of 2008. https://www.congress.gov/bill/110th-congress/senate-bill/3406
- U.S. Congress. (2009). H.R.3590 – Patient Protection and Affordable Care Act. https://www.congress.gov/bill/111th-congress/house-bill/3590/text
- U.S. Department of Health and Human Services. (1996). The Personal Responsibility and Work Opportunity Reconciliation Act of 1996. https://aspe.hhs.gov/reports/personal-responsibility-work-opportunity-reconciliation-act-1996
- U.S. Department of Health and Human Services. (n.d.). The Mental Health Parity and Addiction Equity Act. https://www.hhs.gov/guidance/document/mental-health-parity-and-addiction-equity-act
- U.S. Department of Health and Human Services. (n.d.). Your rights under Section 504 of the Rehabilitation Act. https://www.hhs.gov/sites/default/files/ocr/civilrights/resources/factsheets/504.pdf
- U.S. Department of Health and Human Services. (n.d.). HIPAA. https://www.hhs.gov/hipaa/index.html