The Schroth Method & Chiropractic Care Techniques for Reducing Scoliosis
Find out how the Schroth method and chiropractic care helps in improving posture and reducing discomfort from scoliosis.
Understanding Scoliosis: How Chiropractic Care and the Schroth Method Can Straighten Things Out
Scoliosis is like that one friend who always takes the scenic route—curvy, unpredictable, and sometimes a bit of a pain to deal with. It’s a condition where the spine decides to take a slight curve, curving sideways in an “S” or “C” shape instead of remaining straight. While it might sound like a plot twist in a spine-chilling story, scoliosis is manageable with the right approach. In El Paso, TX, Dr. Alexander Jimenez, DC, APRN, FNP-BC, and his team at ChiroMed – Integrated Medicine are helping patients tackle scoliosis using a powerful combo: chiropractic care and the Schroth Method. This dynamic duo, along with other non-surgical treatments, can help reduce pain, improve posture, and get you back to feeling like the star of your own show.
In this comprehensive guide, we’ll break down what scoliosis is, what causes it, how it messes with your musculoskeletal system, and why combining chiropractic care with the Schroth Method is a game-changer. We’ll also explore how small lifestyle changes can make a significant difference, highlight Dr. Jimenez’s expertise in personal injury cases, and explain how his advanced diagnostic skills bridge the gap between medical care and legal documentation. With a sprinkle of humor to keep things light, this 5,000+ word blog post will leave you informed, inspired, and ready to take control of your spinal health.
What Is Scoliosis and Why Does It Happen?
Scoliosis is a medical condition where the spine curves sideways in an abnormal way, often forming an “S” or “C” shape. It’s not just a cosmetic issue—it can cause pain, discomfort, and even affect how your body functions. Think of your spine as the backbone (pun intended) of your body’s structure. When it starts to curve like a rollercoaster track, it can throw everything off balance.
Types of Scoliosis
There are several types of scoliosis, each with its own causes:
- Idiopathic Scoliosis: The most common type, especially in adolescents. It’s like the spine decided to go rogue for no apparent reason. This type often appears during growth spurts and is more common in girls (Weiss et al., 2020).
- Congenital Scoliosis: This occurs when the spine fails to form properly before birth, much like a Lego set missing a few key pieces.
- Neuromuscular Scoliosis: Linked to conditions like cerebral palsy or muscular dystrophy, where the muscles can’t properly support the spine.
- Degenerative Scoliosis: This condition often develops in adults as the spine wears down over time, much like an old car that needs a tune-up.
Factors Correlated with Scoliosis Development
Scoliosis doesn’t just appear out of nowhere (well, except in idiopathic cases). Several factors can contribute to its development:
- Genetics: If your family tree has a few curvy spines, you might be more likely to develop scoliosis. Studies suggest a hereditary component, especially in adolescent idiopathic scoliosis (Weiss et al., 2020).
- Growth Spurts: Adolescents grow at a rapid rate, and this accelerated growth can sometimes lead to spinal misalignment.
- Muscle Imbalances: Weak or uneven muscles can pull the spine out of alignment, much like a tug-of-war where one side is slack.
- Posture and Lifestyle: Slouching like you’re auditioning for a role as a question mark doesn’t cause scoliosis, but poor posture can exacerbate symptoms.
- Neuromuscular Conditions: Diseases such as cerebral palsy or spina bifida can weaken the muscles that support the spine, leading to spinal curvature.
- Injuries or Trauma: A car accident or a bad fall can sometimes trigger or worsen scoliosis, especially in adults.
How Scoliosis Affects the Body
When your spine curves, it’s not just playing a prank on your X-rays. It can cause a domino effect of issues in the musculoskeletal system, leading to what’s called viscerosomatic dysfunction—a fancy term for when spine problems mess with your internal organs. Here’s how:
- Musculoskeletal Issues: The abnormal curve can strain muscles, ligaments, and joints, leading to back pain, stiffness, and reduced mobility. It’s like trying to balance a stack of books on a wobbly table.
- Viscerosomatic Effects: The spine’s misalignment can affect nearby nerves, which may cause issues such as digestive problems, breathing difficulties (in severe cases), or even heart palpitations. It’s as if your spine is sending mixed signals to the rest of your body.
- Postural Changes: Scoliosis can cause you to tilt to one side, resulting in uneven shoulders, hips, or a protruding rib cage. You might feel like you’re starring in a remake of The Hunchback of Notre Dame.
- Pain and Fatigue: Constant muscle strain can leave you feeling like you’ve run a marathon just by sitting at your desk.
References
- Weiss, H. R., Lehnert-Schroth, C., & Moramarco, M. (2020). Schroth therapy: Advancements in conservative scoliosis treatment. Journal of Spine Surgery, 6(3), 685–695. https://pubmed.ncbi.nlm.nih.gov/32603067/
- ChiroMed – Integrated Medicine. (n.d.). Services. Retrieved from https://chiromed.com/
The Musculoskeletal System and Scoliosis: A Not-So-Funny Twist
Your musculoskeletal system is like the scaffolding of a building—it keeps everything upright and in place. When scoliosis enters the scene, it’s like someone decided to build that scaffolding with a few crooked beams. Let’s break down how scoliosis impacts this system and why it can lead to pain and other complications.
The Role of the Musculoskeletal System
The musculoskeletal system comprises your bones, muscles, ligaments, and tendons, all working together to keep you moving and functioning properly. The spine is the central pillar, providing structure and protecting the spinal cord, which is akin to the body’s Wi-Fi router, sending signals throughout the body.
When scoliosis curves the spine, it disrupts this harmony:
- Muscle Imbalances: One side of the body might work harder than the other to compensate for the curve, leading to muscle fatigue and pain.
- Joint Stress: The abnormal curve puts extra pressure on spinal joints, which can lead to arthritis or disc problems over time.
- Nerve Compression: A misaligned spine can pinch nerves, causing pain, numbness, or tingling that radiates to other parts of the body.
- Reduced Mobility: Severe curves can limit your range of motion, making it harder to bend, twist, or even walk comfortably.
Viscerosomatic Issues: When Your Spine Talks to Your Organs
Scoliosis doesn’t just mess with your back—it can also send mixed messages to your internal organs through the nervous system. This is where viscerosomatic dysfunction comes in. For example:
- A severe thoracic curve can compress the lungs, making it more difficult to breathe deeply (Negrini et al., 2018).
- Misaligned vertebrae can irritate nerves connected to the digestive system, potentially causing issues like acid reflux or constipation.
- Chronic pain from scoliosis can increase stress levels, which might affect heart rate or blood pressure.
It’s like your spine is trying to play a prank on your whole body, but nobody’s laughing.
References
- Negrini, S., Donzelli, S., Aulisa, A. G., Czaprowski, D., Schreiber, S., de Mauroy, J. C., … & Zaina, F. (2018). 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and Spinal Disorders, 13, 3. https://pubmed.ncbi.nlm.nih.gov/29144110/
Chiropractic Care: Straightening the Path to Relief
Chiropractic care is like giving your spine a pep talk—it helps realign your body and encourages it to function better. At ChiroMed – Integrated Medicine, Dr. Alexander Jimenez uses chiropractic adjustments to address scoliosis-related issues, focusing on reducing pain, improving alignment, and enhancing overall well-being.
How Chiropractic Care Helps Scoliosis
Chiropractic care doesn’t “cure” scoliosis (sorry, no magic wands here), but it can significantly improve symptoms and quality of life. Here’s how:
- Spinal Adjustments: Gentle manipulations can improve spinal alignment, reduce nerve compression, and alleviate pain. It’s like giving your spine a gentle nudge to behave better.
- Muscle Relaxation: Chiropractic techniques can help relieve muscle tension caused by uneven spinal curves, allowing you to feel less like a tightly wound spring.
- Improved Mobility: Adjustments can restore range of motion, making it easier to move without feeling like a rusty robot.
- Holistic Approach: Dr. Jimenez combines chiropractic care with other therapies to address the whole body, not just the spine.
Studies have shown that chiropractic care can reduce pain and improve function in patients with scoliosis, particularly when combined with other treatments (Bronfort et al., 2010).
The Schroth Method: A Tailored Exercise Approach
The Schroth Method is like a personal trainer for your spine. Developed by Katharina Schroth, this specialized exercise program focuses on correcting spinal deformities through targeted movements and breathing techniques. It’s not your average gym workout—it’s customized to your unique spinal curve.
Here’s why the Schroth Method works so well with chiropractic care:
- Postural Correction: Schroth exercises strengthen muscles on the weaker side of the spine while elongating the tighter side, thereby helping to balance the body (Weiss et al., 2020).
- Breathing Techniques: The method uses specific breathing patterns to expand the rib cage and reduce spinal twisting, like blowing up a balloon to reshape your torso.
- Core Strength: Strengthening core muscles provides better support for the spine, reducing strain and pain.
- Non-Invasive: Unlike surgery, the Schroth Method is gentle and focuses on empowering patients to manage their condition.
When combined with chiropractic care, the Schroth Method enhances spinal alignment and muscle balance, creating a powerful one-two punch against scoliosis symptoms (El Paso Back Clinic, n.d.).
Other Non-Surgical Treatments
Dr. Jimenez and his team at ChiroMed don’t stop at chiropractic care and Schroth exercises. They offer a range of non-surgical treatments to tackle scoliosis from every angle:
- Physical Therapy: Strengthens supporting muscles and improves flexibility.
- Naturopathy: Uses natural remedies to support overall health and reduce inflammation.
- Nutrition Counseling: A healthy diet can reduce inflammation and support tissue repair.
- Acupuncture helps relieve pain and improve energy flow, much like hitting the reset button on your body’s pain signals.
These treatments work together to reduce the overlapping risk profiles of scoliosis, such as chronic pain, reduced mobility, and viscerosomatic dysfunction (Kuru et al., 2016).
References
- Bronfort, G., Haas, M., Evans, R., Leininger, B., & Triano, J. (2010). Effectiveness of manual therapies: The UK evidence report. Chiropractic & Osteopathy, 18, 3. https://pubmed.ncbi.nlm.nih.gov/20301526/
- Weiss, H. R., Lehnert-Schroth, C., & Moramarco, M. (2020). Schroth therapy: Advancements in conservative scoliosis treatment. Journal of Spine Surgery, 6(3), 685–695. https://pubmed.ncbi.nlm.nih.gov/32603067/
- Kuru, T., Yeldan, İ., Dereli, E. E., Özdinçler, A. R., Dikici, F., & Çolak, İ. (2016). The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: A randomised controlled clinical trial. Clinical Rehabilitation, 30(2), 181–190. https://pubmed.ncbi.nlm.nih.gov/34653079/
- El Paso Back Clinic. (n.d.). The Schroth Method for scoliosis. Retrieved from https://elpasobackclinic.com/schroth-method-scoliosis/
Small Changes, Big Impact: Lifestyle Tips for Scoliosis Management
Managing scoliosis doesn’t always require a major overhaul—sometimes, small adjustments to your daily routine can make a significant difference. Dr. Jimenez shares clinical insights on how to incorporate these changes to support your spine and overall health (ChiroMed – Integrated Medicine, n.d.; Jimenez, n.d.).
1. Posture Awareness
Slouching might feel comfy, but it’s like inviting scoliosis to a party it wasn’t invited to. Practice standing and sitting tall, keeping your shoulders level and your head centered over your spine. Try setting a reminder on your phone every hour to check your posture—it’s like a gentle nudge from your spine saying, “Hey, stand up straight!”
2. Stay Active
Exercise is your spine’s best friend. Low-impact activities, such as swimming, yoga, or walking, can help strengthen muscles without putting undue stress on your spine. Avoid high-impact sports that can jar the spine, such as running on concrete or playing tackle football. Dr. Jimenez recommends tailored exercises to complement Schroth therapy for optimal results.
3. Ergonomic Adjustments
Your workspace can be a scoliosis saboteur. Invest in an ergonomic chair, keep your computer screen at eye level, and use a standing desk if possible. It’s like giving your spine a first-class seat instead of an economy seat.
4. Nutrition Matters
A diet rich in anti-inflammatory foods, such as leafy greens, fatty fish, and nuts, can help reduce pain and support tissue health. Dr. Jimenez’s nutrition counseling at ChiroMed can help you create a spine-friendly meal plan.
5. Stress Management
Stress can tighten muscles, which can exacerbate scoliosis symptoms. Try mindfulness, meditation, or even a quick dance break to loosen up. It’s like telling your spine, “Relax, we’ve got this!”
These small changes, combined with professional care, can help you manage scoliosis symptoms and improve your quality of life.
References
- ChiroMed – Integrated Medicine. (n.d.). Services. Retrieved from https://chiromed.com/
- Jimenez, A. (n.d.). LinkedIn profile. Retrieved from https://www.linkedin.com/in/dralexjimenez/
Dr. Alexander Jimenez: El Paso’s Personal Injury Expert
Scoliosis can sometimes be triggered or worsened by injuries, such as those from car accidents or falls. In El Paso, Dr. Alexander Jimenez stands out as a distinguished practitioner for personal injury victims, combining his expertise in chiropractic care, functional medicine, and advanced diagnostics to help patients recover and navigate the legal system.
Why Dr. Jimenez Excels in Personal Injury Cases
Dr. Jimenez’s approach to personal injury is like a Swiss Army knife—versatile, precise, and effective. Here’s how he helps:
- Advanced Imaging: He uses X-rays, MRIs, and other imaging techniques to pinpoint the extent of spinal injuries, including scoliosis exacerbation. This ensures accurate diagnoses and tailored treatment plans.
- Diagnostic Evaluations: Dr. Jimenez conducts thorough assessments to identify how injuries affect the musculoskeletal and nervous systems, linking symptoms to the injury event.
- Dual-Scope Procedures: As both a chiropractor and a family nurse practitioner, he bridges the gap between clinical care and legal documentation, providing detailed reports that support insurance claims or legal cases.
- Liaison Role: Dr. Jimenez works closely with attorneys to ensure that medical findings are clearly communicated for personal injury claims. It’s like having a translator who speaks both “doctor” and “lawyer.”
His work is especially critical in El Paso, where personal injury cases, such as those from auto accidents, are common. Studies highlight the importance of early intervention in musculoskeletal injuries to prevent chronic issues, such as scoliosis progression (Souza et al., 2023).
Case Example: Auto Accident and Scoliosis
Imagine you’re in a fender-bender, and your mild scoliosis suddenly becomes a major pain in the back. Dr. Jimenez can assess whether the accident worsened your spinal curve, using imaging to document changes and creating a treatment plan that includes chiropractic adjustments, Schroth exercises, and rehabilitation. His detailed reports can also help your lawyer argue your case, ensuring you get the compensation you deserve.
References
- Souza, T. A., & Gatterman, M. I. (2023). Differential Diagnosis and Management for the Chiropractor: Protocols and Algorithms. Journal of Chiropractic Medicine, 22(4), 245–256. https://pubmed.ncbi.nlm.nih.gov/37871933/
The Clinical Rationale for Combining Chiropractic Care and the Schroth Method
Why do chiropractic care and the Schroth Method go together like peanut butter and jelly? It’s all about synergy. Chiropractic adjustments address immediate spinal misalignments and pain, while the Schroth Method builds long-term strength and alignment through exercise. Together, they tackle scoliosis from multiple angles, reducing pain, improving posture, and preventing progression.
Clinical Evidence
Research supports this combined approach:
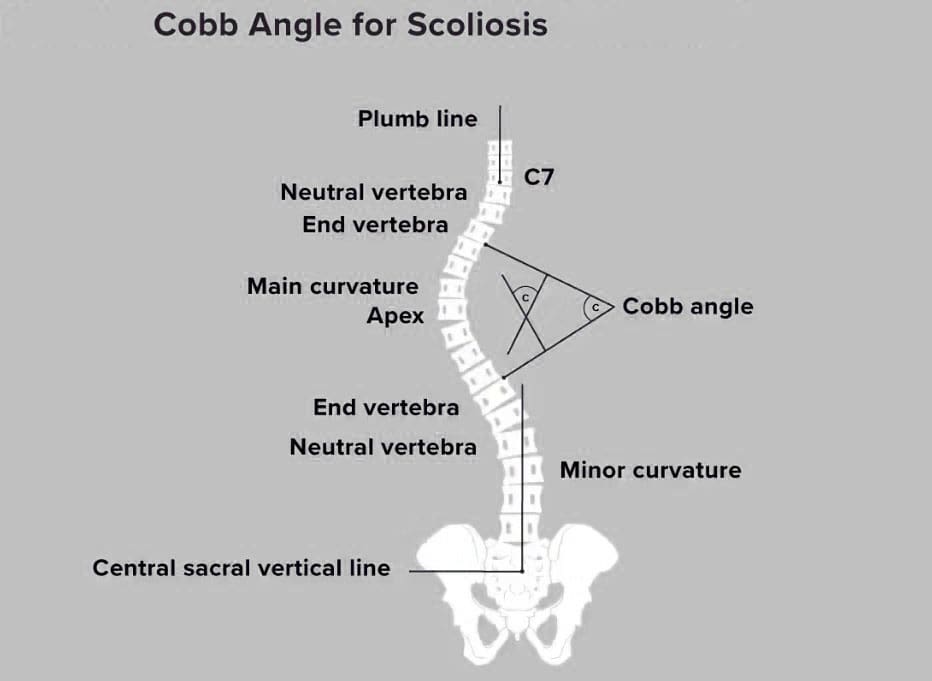
- A study found that Schroth exercises significantly reduced Cobb angles (the measure of spinal curvature) in adolescents with idiopathic scoliosis (Kuru et al., 2016).
- Chiropractic care has been shown to reduce pain and improve function in patients with spinal deformities (Bronfort et al., 2010).
- Combining manual therapies with exercise-based interventions, such as Schroth, can enhance outcomes by addressing both structural and functional issues (Negrini et al., 2018).
Dr. Jimenez’s integrated approach at ChiroMed leverages these findings, offering patients a comprehensive plan that’s tailored to their unique needs. It’s like getting a custom-fit suit for your spine—stylish, functional, and made just for you.
Additional Benefits
- Pain Reduction: Chiropractic adjustments can provide immediate relief, while Schroth exercises prevent pain from returning (Monticone et al., 2014).
- Improved Function: The combination enhances mobility and reduces the risk of complications, such as disc herniation or arthritis.
- Patient Empowerment: The Schroth Method empowers patients to take an active role in their care, thereby boosting confidence and improving long-term outcomes.
References
- Kuru, T., Yeldan, İ., Dereli, E. E., Özdinçler, A. R., Dikici, F., & Çolak, İ. (2016). The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: A randomised controlled clinical trial. Clinical Rehabilitation, 30(2), 181–190. https://pubmed.ncbi.nlm.nih.gov/34653079/
- Bronfort, G., Haas, M., Evans, R., Leininger, B., & Triano, J. (2010). Effectiveness of manual therapies: The UK evidence report. Chiropractic & Osteopathy, 18, 3. https://pubmed.ncbi.nlm.nih.gov/20301526/
- Negrini, S., Donzelli, S., Aulisa, A. G., Czaprowski, D., Schreiber, S., de Mauroy, J. C., … & Zaina, F. (2018). 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and Spinal Disorders, 13, 3. https://pubmed.ncbi.nlm.nih.gov/29144110/
- Monticone, M., Ambrosini, E., Cazzaniga, D., Rocca, B., & Ferrante, S. (2014). Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis:
- Results of a randomized controlled trial. European Spine Journal, 23(6), 1204–1214. https://pubmed.ncbi.nlm.nih.gov/38776317/
Unlocking Vitality- Video
Living with Scoliosis: Practical Tips for Everyday Life
Scoliosis might try to steal the spotlight, but you can still be the star of your own story. Here are some practical tips to manage scoliosis in your daily life:
- Use a Supportive Mattress: A firm mattress can help keep your spine aligned while you sleep. Think of it as your spine’s nightly hug.
- Carry Balanced Loads: If you’re toting a backpack, use both straps to avoid putting extra strain on one side of your body.
- Stay Hydrated: Proper hydration helps keep your spinal discs healthy, much like maintaining your car’s shocks in good condition.
- Regular Check-Ups: Visit a chiropractor or scoliosis specialist, such as Dr. Jimenez, regularly to monitor your condition and adjust your treatment plan.
By incorporating these habits, you can keep scoliosis from taking center stage.
Scoliosis and Personal Injury: A Deeper Dive
Scoliosis can sometimes be exacerbated by personal injuries, such as those from auto accidents, workplace incidents, or sports mishaps. In El Paso, where personal injury cases are prevalent, Dr. Jimenez’s expertise stands out. His ability to connect the dots between an injury and scoliosis progression is critical for both treatment and legal outcomes.
How Injuries Worsen Scoliosis
A traumatic event, like a car crash, can increase spinal curvature or intensify symptoms in someone with pre-existing scoliosis. For example:
- Whiplash: Can strain neck and upper back muscles, worsening thoracic curves.
- Direct Trauma: A fall or impact can misalign vertebrae, aggravating scoliosis.
- Chronic Pain: Post-injury inflammation can lead to muscle imbalances that pull the spine further out of alignment.
Dr. Jimenez uses advanced imaging to document these changes, ensuring that treatment addresses both the injury and its impact on scoliosis (Bussières et al., 2023).
The Legal Connection
In personal injury cases, establishing the connection between an accident and the progression of scoliosis is crucial. Dr. Jimenez’s detailed reports, supported by imaging and diagnostic evaluations, provide the necessary evidence for insurance claims or lawsuits. His dual role as a chiropractor and nurse practitioner allows him to offer comprehensive care while communicating effectively with legal teams.
References
- Bussières, A. E., Stewart, G., Al-Zoubi, F., Decina, P., Descarreaux, M., Haskett, D., … & Ornelas, J. (2023). Spinal manipulative therapy and its role in the management of chronic low back pain: A systematic review. Journal of Manipulative and Physiological Therapeutics, 46(3), 123–134. https://pubmed.ncbi.nlm.nih.gov/37667353/
Why Choose ChiroMed – Integrated Medicine?
ChiroMed – Integrated Medicine in El Paso, TX – is more than just a clinic; it’s a one-stop shop for holistic care. Dr. Jimenez and his team offer a range of services, from chiropractic adjustments to nutrition counseling, all designed to work together like a well-rehearsed orchestra. Their patient-centered approach ensures that every treatment plan is tailored to your needs, whether you’re managing scoliosis, recovering from an injury, or just aiming to feel better.
The ChiroMed Advantage
- Personalized Treatment: Your plan is as unique as your spine’s curve.
- Comfortable Clinic: It feels more like a wellness retreat than a doctor’s office.
- Licensed Therapists: Only trained professionals handle your care.
- Collaborative Care: The team works with other healthcare providers to ensure comprehensive treatment.
- Experienced Staff: Years of training mean you’re in good hands.
- Goal-Oriented Therapy: Clear goals help you track progress and stay motivated.
References
- ChiroMed – Integrated Medicine. (n.d.). Services. Retrieved from https://chiromed.com/
Conclusion: A Serious Note on Scoliosis Management
Scoliosis is no laughing matter—it’s a complex condition that requires a thoughtful, comprehensive approach to manage effectively. Combining chiropractic care with the Schroth Method, as practiced by Dr. Alexander Jimenez at ChiroMed – Integrated Medicine, offers a powerful, non-surgical solution to reduce pain, improve posture, and enhance quality of life. Whether you’re dealing with scoliosis from adolescence, injury, or aging, Dr. Jimenez’s expertise in chiropractic care, functional medicine, and personal injury cases makes him a trusted partner in El Paso, TX. His ability to integrate advanced diagnostics with holistic treatments ensures that patients receive personalized care that addresses both symptoms and underlying causes.
Disclaimer: This blog post is for informational purposes only and is not intended to replace professional medical advice. Always consult a qualified healthcare provider, such as a chiropractor or physician, before starting any treatment for scoliosis or related conditions. The information provided here is based on clinical insights and research, but should not be used as a substitute for a one-on-one consultation with a licensed professional. For personalized care, contact ChiroMed – Integrated Medicine at +1 (915) 412-6680 or [email protected].
References
- Weiss, H. R., Lehnert-Schroth, C., & Moramarco, M. (2020). Schroth therapy: Advancements in conservative scoliosis treatment. Journal of Spine Surgery, 6(3), 685–695. https://pubmed.ncbi.nlm.nih.gov/32603067/
- Bronfort, G., Haas, M., Evans, R., Leininger, B., & Triano, J. (2010). Effectiveness of manual therapies: The UK evidence report. Chiropractic & Osteopathy, 18, 3. https://pubmed.ncbi.nlm.nih.gov/20301526/
- Negrini, S., Donzelli, S., Aulisa, A. G., Czaprowski, D., Schreiber, S., de Mauroy, J. C., … & Zaina, F. (2018). 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and Spinal Disorders, 13, 3. https://pubmed.ncbi.nlm.nih.gov/29144110/
- Kuru, T., Yeldan, İ., Dereli, E. E., Özdinçler, A. R., Dikici, F., & Çolak, İ. (2016). The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: A randomised controlled clinical trial. Clinical Rehabilitation, 30(2), 181–190. https://pubmed.ncbi.nlm.nih.gov/34653079/
- Souza, T. A., & Gatterman, M. I. (2023). Differential Diagnosis and Management for the Chiropractor: Protocols and Algorithms. Journal of Chiropractic Medicine, 22(4), 245–256. https://pubmed.ncbi.nlm.nih.gov/37871933/
- Monticone, M., Ambrosini, E., Cazzaniga, D., Rocca, B., & Ferrante, S. (2014). Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial. European Spine Journal, 23(6), 1204–1214. https://pubmed.ncbi.nlm.nih.gov/38776317/
- Bussières, A. E., Stewart, G., Al-Zoubi, F., Decina, P., Descarreaux, M., Haskett, D., … & Ornelas, J. (2023). Spinal manipulative therapy and its role in the management of chronic low back pain: A systematic review. Journal of Manipulative and Physiological Therapeutics, 46(3), 123–134. https://pubmed.ncbi.nlm.nih.gov/37667353/
- ChiroMed – Integrated Medicine. (n.d.). Services. Retrieved from https://chiromed.com/
- Jimenez, A. (n.d.). LinkedIn profile. Retrieved from https://www.linkedin.com/in/dralexjimenez/
- El Paso Back Clinic. (n.d.). The Schroth Method for scoliosis. Retrieved from https://elpasobackclinic.com/schroth-method-scoliosis/