The Throwing Motion and Its Impact on Performance
Can understanding the mechanics of the throwing motion help to understand why it may cause shoulder pain, the symptoms of a shoulder problem, the diagnosis, and the treatment options available?
Throwing a Ball and Shoulder Pain
The throwing motion is a complex shoulder movement that requires the mechanics of muscles, tendons, joints, ligaments, and bones. They all must move in a synchronized and stable pattern to move the shoulder joint. When these mechanics are interrupted or altered, inflammation can result in pain symptoms. (Wardell M., Creighton D., & Kovalcik C., 2022)
Throwing Motion
Distinct phases characterize the throwing motion:
- The wind up
- Cocking
- Acceleration
- Follow-through
- Deceleration
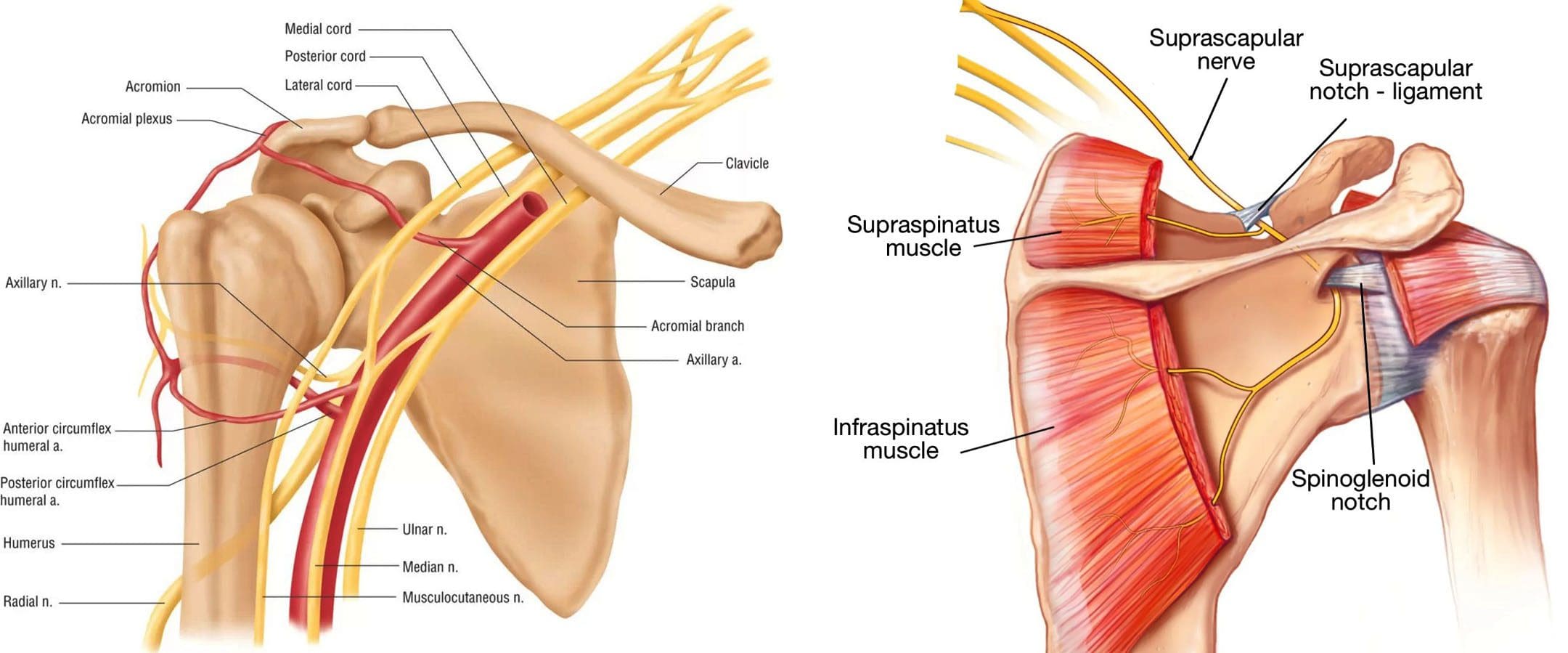
- The rotator cuff and shoulder muscles sequentially guide the movements for effective throwing mechanics. (Wardell M., Creighton D., & Kovalcik C., 2022)
- The labrum stabilizes the ball in the socket of the shoulder.
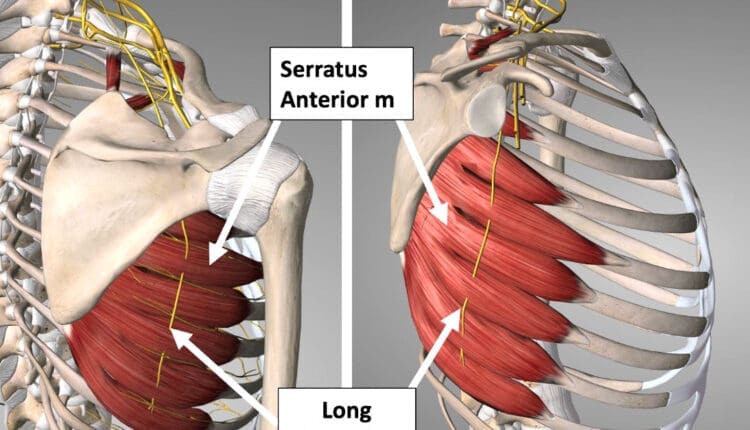
- The shoulder blade rotation coordinates with the arm to ensure mobility. (Itoigawa Y. et al., 2023)
The throwing motion generates high torque and acceleration forces acting on the shoulder joint and the surrounding muscles, ligaments, and tendons.
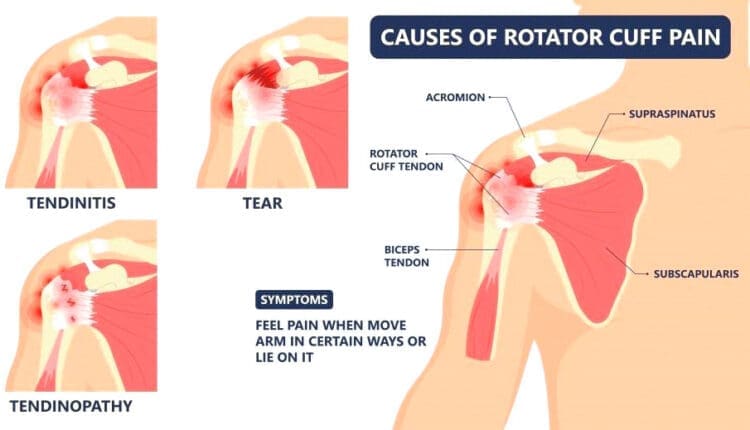
Causes of Pain
Pain when throwing can come from the:
- Shoulder blade
- Shoulder joint – cartilage and labrum
- Rotator cuff muscles and tendons
- Nerves that control the muscles’ function
The shoulder blade is attached to the upper back by ligaments, muscles, and tendons. The various muscles and tendons that control the movement of the shoulder blade impact movements. Abnormalities of any area can lead to shoulder dysfunction and pain when throwing. (Wardell M., Creighton D., & Kovalcik C., 2022) The most common is the tightness of the posterior shoulder capsule, causing a loss of normal internal rotation of the shoulder. If this is causing pain, individuals may notice that they can’t reach up as high on the side with the painful shoulder when reaching behind their back.
Symptoms
Whether an athlete or playing catch in the backyard, shoulder function abnormalities can cause significant pain. Some symptoms include.
Aching Pain
- Often deep in the shoulder or extending down the upper arm.
Dead Arm
- Lack of strength in the throwing motion.
Pain at Night
- Pain can awaken you from sleep.
Diagnosis
Finding a healthcare provider familiar with sports injuries can be helpful. They can best determine if a structural abnormality needs to be addressed. (American Academy of Orthopaedic Surgeons, 2021)
Treatment
Most can improve with nonsurgical treatments. The earliest phase of treatment is resting the joint and reducing inflammation. Treatments can include:
- Ice
- Anti-inflammatory medications
- Cortisone injection
Once the inflammation has subsided, the source of the discomfort can be addressed.
Physical Therapy
Therapy can include:
- A structured shoulder stretching and strengthening program will help.
- The physical therapist will focus on scapular mobility when managing shoulder joint problems.
Exercises may include: (American Academy of Orthopaedic Surgeons, 2024)
- Stretching to improve internal rotation or any other lost motion can help allow a more normal throwing motion.
- Strength exercises are often aimed at the rotator cuff, as these muscles initiate proper shoulder movements and stabilize the shoulder joint.
- Maintaining flexibility and strength of the periscapular muscles (muscles that attach to the scapula bone) is important to ensure that the scapular movements are coordinated with the throwing motion.
Suppose improvements are not made within three months of therapy, or individuals can’t return to competitive sports within six months. In that case, the individual may need to return to their healthcare provider or see an orthopedic specialist who may recommend surgery. (American Academy of Orthopaedic Surgeons, 2024)
Injury Medical Chiropractic and Functional Medicine Clinic
As a Family Practice Nurse Practitioner, Dr. Jimenez combines advanced medical expertise with chiropractic care to address various conditions.
- Wellness & Nutrition: Personalized plans to optimize health and prevent disease.
- Chronic Pain Management: Non-invasive solutions for fibromyalgia, sciatica, and low back pain.
- Personal Injury & Auto Accident Care: Tailored rehabilitation for whiplash, soft tissue injuries, and more.
- Sports Injuries & Orthopedic Care: Treatment for sprains, strains, and complex injuries.
- Functional Medicine: Root-cause analysis for chronic disorders, incorporating nutrition, lifestyle, and environmental factors.
- Neuromusculoskeletal Health: Care for neck pain, migraines, herniated discs, and scoliosis.
Our clinic integrates Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine to create customized care plans that promote natural healing, mobility, and long-term wellness. By focusing on flexibility, agility, and strength, we empower patients to thrive, regardless of age or health challenges.
At El Paso’s Chiropractic Rehabilitation Clinic & Integrated Medicine Center, we passionately focus on treating patients after frustrating injuries and chronic pain syndromes. We focus on improving your ability through flexibility, mobility, and agility programs tailored for all age groups and disabilities. We use in-person and virtual health coaching and comprehensive care plans to ensure every patient’s personalized care and wellness outcomes.
Lumbar Spine Injuries in Sports: Chiropractic Healing
References
Wardell, M., Creighton, D., & Kovalcik, C. (2022). Glenohumeral Instability and Arm Pain in Overhead Throwing Athletes: A Correlational Study. International journal of sports physical therapy, 17(7), 1351–1357. https://doi.org/10.26603/001c.39800
Itoigawa, Y., Koga, A., Morikawa, D., Kubota, A., Uehara, H., Maruyama, Y., Takazawa, Y., & Ishijima, M. (2023). Posterior shoulder stiffness was associated with shoulder pain during throwing in college baseball players: assessment of shear wave elastography. European journal of orthopaedic surgery & traumatology: orthopedie traumatologie, 33(4), 1237–1244. https://doi.org/10.1007/s00590-022-03286-z
American Academy of Orthopaedic Surgeons. (2021). Shoulder Injuries in the Throwing Athlete. https://orthoinfo.aaos.org/en/diseases–conditions/shoulder-injuries-in-the-throwing-athlete/
American Academy of Orthopaedic Surgeons. (2024). Shoulder Impingement/Rotator Cuff Tendinitis. https://orthoinfo.aaos.org/en/diseases–conditions/shoulder-impingementrotator-cuff-tendinitis