Could individuals who are having headaches with neck pain need emergency treatment or need to get started with sustained physical therapy?
Headaches and Neck Pain
Headaches and neck pain are two very common symptoms. They often occur together and signal common health issues, including fatigue, sinus headaches, and migraines. The combination can also occur due to serious health issues such as a concussion or meningitis. Causes of headaches with neck pain range from various causes, such as not getting enough sleep, having the neck in an awkward position, or having a hangover, to life-threatening issues like fluid buildup in the brain. It is recommended that individuals see a healthcare provider as soon as possible to rule out any life-threatening issues. Discuss the symptoms of neck pain with headache, what can cause these symptoms, and discuss treatment and prevention.
Symptoms
Symptoms are similar to what they feel like when they occur alone. Headache can present as:
- A feeling of fullness in the head
- Head soreness
- Sharp head pain
- Throbbing head pain
- Pounding head pain
Neck pain can present as:
- Pain in the back of the neck
- Pain and/or aching of the upper back and/or shoulders
Associated Symptoms
Additional symptoms are common. Symptoms associated with headaches and neck pain include:
- Neck stiffness
- Trouble concentrating
- Exhaustion or sleepiness
- Aching throughout the body
- Nausea
- Dizziness
- Vertigo – feeling like the room is spinning.
- Photophobia – discomfort when looking at bright lights.
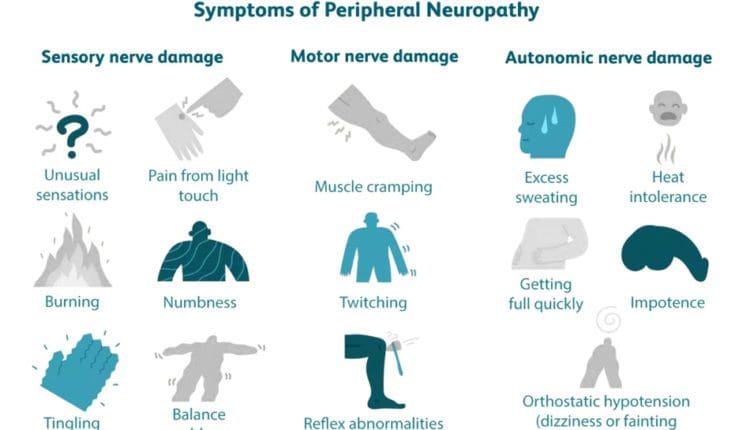
- A feeling of numbness or tingling down the arm
Generally, associated symptoms suggest a more severe cause and can help a healthcare provider make a diagnosis.
Emergency Help
New symptoms of headache or neck pain can indicate a serious condition. If you develop these symptoms together, get prompt medical attention.
Causes
There are a variety of medical conditions that can cause headaches and neck pain. Both of these conditions are caused by irritation of sensory nerve fibers. Sometimes, head or neck pain can spread to other areas because the sensory nerves of these structures are so close together. (Côté P. et al., 2019) Additionally, a medical condition like an infection can affect the other due to proximity. Causes of headaches with neck pain include:
Headaches
- Sinus headaches, tension headaches, and cervicogenic headaches are usually associated with head pain, but they can also involve neck pain. (Côté P. et al., 2019)
Migraine
- Migraines are commonly associated with headaches and often cause neck pain as well.
- In addition, they can cause nausea and body aches.
Fatigue
- Being tired commonly leads to temporary headaches and neck pain until thorough rest is achieved.
Alcohol Consumption and/or a Hangover
- For many, drinking can trigger a headache.
- This is a common migraine trigger, but it can also trigger headaches for those who don’t have migraines.
Muscle Strain
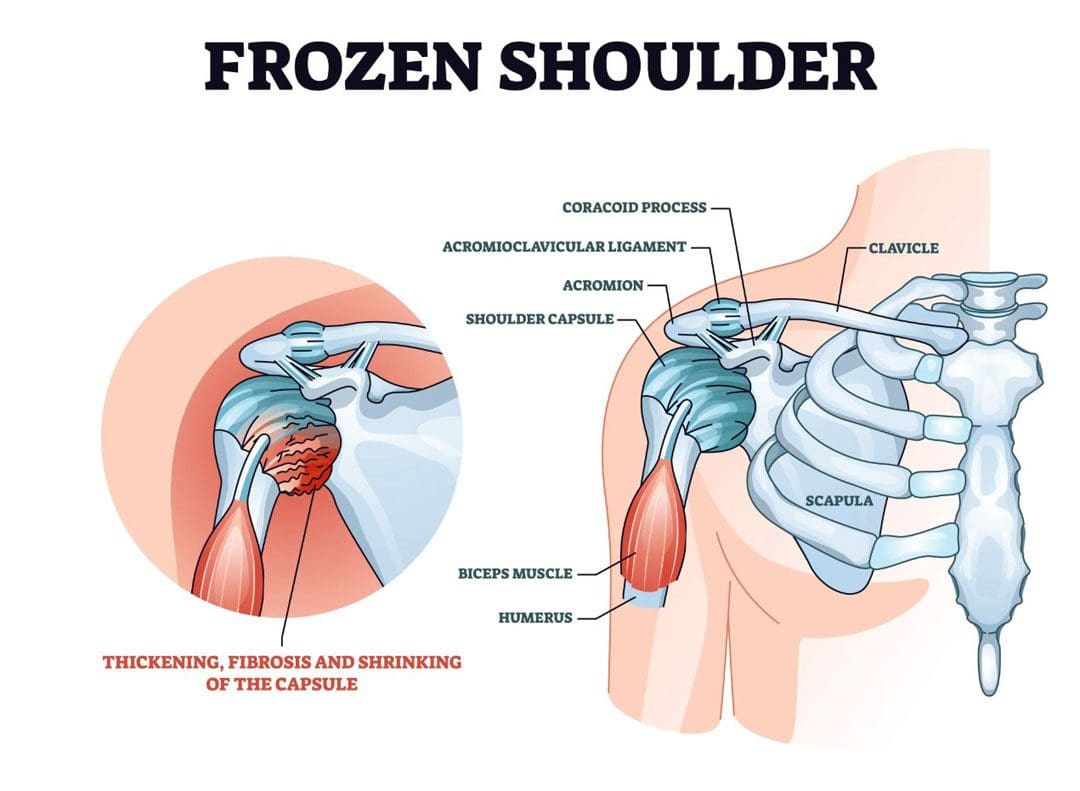
- Prolonged or recurrent positions that strain the neck muscles, like lifting or sitting at a desk, can cause aching or pain that involves both the head and neck. (Houle M. et al., 2021)
Injuries
- Trauma such as whiplash or falling can cause soreness in the head and neck.
- Bruises or other injuries may be present.
- Severe injuries can cause damage to the skull, brain, spine, spinal nerves, or spinal cord.
Concussion
- A concussion often causes trouble concentrating, persistent headaches, and neck pain.
- Usually, these symptoms improve within a few weeks after a mild concussion.
Meningitis
- Inflammation or infection of the lining around the brain and spinal cord causes pain or tenderness in the head, back, and neck.
- Neck stiffness and fever are commonly associated symptoms.
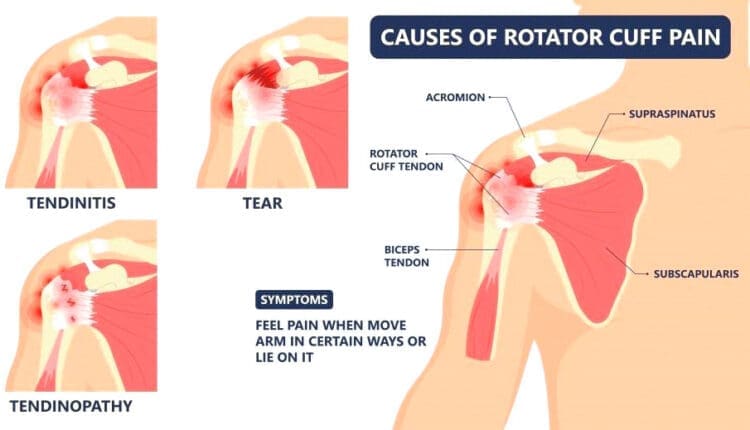
Pinched Nerve
- Arthritis is a common cause of pressure on spinal nerves.
- A pinched nerve in the upper spine can cause pain in the head and neck and tingling down the arm.
Herniated Disc
- Degenerative arthritis or trauma can cause a spinal disc to press on a nerve and possibly on the spinal cord.
- This may cause loss of sensation or weakness of the arm.
Subarachnoid Hemorrhage
- This is a serious condition caused by bleeding of a blood vessel in the brain.
- Irritation and inflammation can cause severe head and neck pain, possibly with seizures and loss of consciousness.
Hydrocephalus
- Fluid can accumulate around the brain, causing pain-inducing pressure.
- Causes include obstruction of cerebrospinal fluid flow due to brain tumors, brain infections, or congenital malformations. (Langner S. et al., 2017)
Increased Intracranial Pressure
- Pressure on the brain and the brain’s blood vessels can cause pain.
- Causes of pressure within the skull include hydrocephalus, head trauma, brain tumors, or swelling from a stroke.
- Severe cases can cause lethargy or loss of consciousness.
Brain or Spine cancer
- Cancer of the brain or within the spine can cause pain affecting the head and neck, often with other symptoms, like loss of vision.
Treatment
Talk to a healthcare provider about the following treatments. Treating headaches with neck pain includes methods that address symptoms and methods that treat the underlying cause. The medications used for headaches with neck pain often reduce both symptoms, but this depends on the cause. Treatments that can relieve both headaches and neck pain when they occur together include:
- Getting proper sleep to alleviate fatigue.
- Rest and rehabilitation after a concussion or another injury.
- Physical therapy to keep muscles flexible and relaxed.
- Non-surgical decompression and traction to decompress the spine.
- Pain medication to relieve pain after minor trauma.
- Migraine medication or sinus headache treatment (Petersen S. M., Jull G. A., & Learman K. E. 2019)
- Fluids for meningitis treatment and antibiotics for bacterial meningitis.
- Surgical procedures for a tumor or subarachnoid hemorrhage.
- A surgical procedure to relieve hydrocephalus.
Headache Treatment
You can do a few things to relieve your headaches, and although they won’t directly take away your neck pain, your headache relief might also decrease your neck pain. These include:
- Avoiding loud noises
- Cranial massage
- Applying gentle cranial pressure
- Avoiding bright lights as much as possible
- Using specialized migraine sunglasses
Neck Pain Treatment
Some treatments that can specifically treat neck pain include:
- Exercise, stretching, and physical therapy (Côté P. et al., 2019)
- Ice or heat
- Muscle relaxants
- Anti-inflammatory injections
Injury Medical Chiropractic and Functional Medicine Clinic
It can be difficult to know whether a serious problem is causing headaches and neck pain. The more dangerous conditions don’t necessarily cause more severe pain. This is why getting medical attention is crucial if you have these symptoms together. If you frequently have both headaches and neck pain, it can have a substantial impact on your quality of life. There are ways to manage the symptoms, including preventative measures such as physical therapy, exercises, and avoiding triggers. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems.
Tension Headaches
References
Côté, P., Yu, H., Shearer, H. M., Randhawa, K., Wong, J. J., Mior, S., Ameis, A., Carroll, L. J., Nordin, M., Varatharajan, S., Sutton, D., Southerst, D., Jacobs, C., Stupar, M., Taylor-Vaisey, A., Gross, D. P., Brison, R. J., Paulden, M., Ammendolia, C., Cassidy, J. D., … Lacerte, M. (2019). Non-pharmacological management of persistent headaches associated with neck pain: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. European journal of pain (London, England), 23(6), 1051–1070. https://doi.org/10.1002/ejp.1374
Houle, M., Lessard, A., Marineau-Bélanger, É., Lardon, A., Marchand, A. A., Descarreaux, M., & Abboud, J. (2021). Factors associated with headache and neck pain among telecommuters – a five days follow-up. BMC Public Health, 21(1), 1086. https://doi.org/10.1186/s12889-021-11144-6
Langner, S., Fleck, S., Baldauf, J., Mensel, B., Kühn, J. P., & Kirsch, M. (2017). Diagnosis and Differential Diagnosis of Hydrocephalus in Adults. Diagnostik und Differenzialdiagnostik des Hydrozephalus beim Erwachsenen. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin, 189(8), 728–739. https://doi.org/10.1055/s-0043-108550
Petersen, S. M., Jull, G. A., & Learman, K. E. (2019). Self-reported sinus headaches are associated with neck pain and cervical musculoskeletal dysfunction: a preliminary observational case-control study. The Journal of manual & manipulative therapy, 27(4), 245–252. https://doi.org/10.1080/10669817.2019.1572987