Biology Strategies for Metabolic Health & Insulin Resistance
By Dr. Alex Jimenez, DC, FNP-APRN
Explore metabolic health with effective strategies to manage insulin resistance. Learn about the biology and solutions now.
Abstract
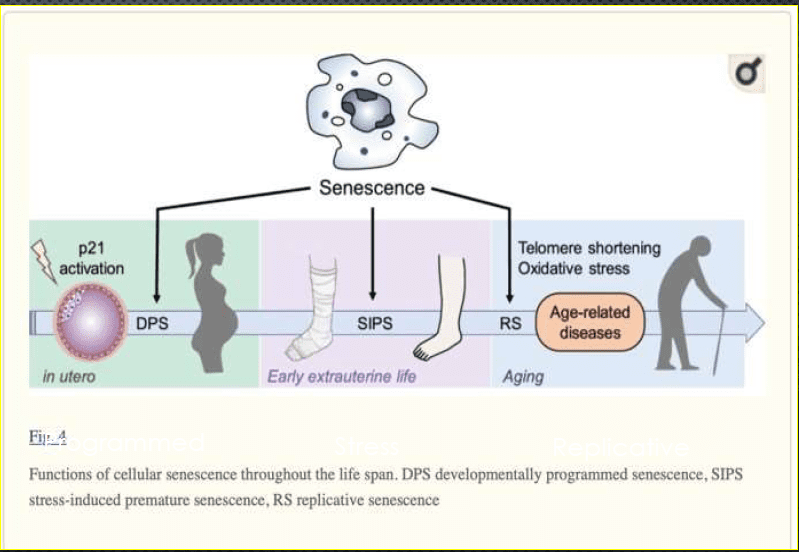
As a clinician bridging chiropractic functional medicine and advanced nursing practice, I have spent decades guiding patients through the complex terrain of metabolic health—where excess adiposity, insulin resistance, chronic stress, mitochondrial inefficiency, and circadian misalignment converge to drive weight gain, cardiometabolic disease, fatigue, and impaired cognitive sharpness. This educational post synthesizes contemporary evidence from leading research teams, including randomized controlled trials, prospective cohorts, mechanistic physiology, multi-omics (genomics, proteomics, metabolomics), and translational studies, to build an actionable, systems biology approach to metabolic resilience. I write in the first person to share how I assess, plan, and implement care, explaining the physiology underlying each recommendation and why specific tactics work.
We begin by clarifying the interconnected axes of metabolism: the stress-cortisol rhythm that shapes insulin signaling and thyroid conversion; the glucose-insulin axis that governs energy storage and endothelial function; the mitochondrial axis that determines whether fuel is burned cleanly or leaks into oxidative byproducts; the immune-inflammatory axis where cytokines (IL-6, TNF-α, NF-κB) impair receptor signaling; the circadian-sleep axis that coordinates hormonal timing and appetite; and the nutrient status axis, where deficits in magnesium, chromium, zinc, B vitamins, protein, vitamin D, and omega-3s hinder energetic throughput and repair. I also unpack adipose biology—white, beige, and brown fat phenotypes—and explain how thermogenic capacity affects metabolic flexibility and basal energy expenditure.
A focus of this post is practical, evidence-based guidance for individuals using and transitioning off GLP-1 receptor agonists. I describe the mechanisms behind appetite suppression, glycemic improvement, and gastric emptying, as well as the risks—especially lean mass loss when protein intake and resistance training are inadequate. I outline a GLP-1 exit strategy that I employ clinically: protein lock-in, strength training, structured meals, micronutrient sufficiency, sleep and stress stabilization, and hunger protocols that maintain satiety while minimizing reward-driven eating.
I provide a detailed clinical decision-tree rubric to evaluate metabolic health holistically: anthropometrics and body composition, glucose and insulin dynamics (fasting glucose, fasting insulin, HOMA-IR, fructosamine, postprandial checks), inflammatory markers (hs-CRP, ferritin), kidney and liver function, thyroid and sex hormones, micronutrients, gut and microbiome assessment, mitochondrial patterning, environmental exposures (arsenic and metals), medications (SSRIs, antipsychotics, steroids, beta-blockers), and behavioral skills. Throughout, I explain why “eat less, move more” is insufficient for many adults over 30–40 due to sarcopenia, hormonal shifts, sleep debt, stress load, and hidden deficiencies.
We explore healthy aging by addressing sarcopenia and bone loss in both men and women, nighttime circadian disruption, COVID-related cytokine and microbiome shifts, and oxidative stress markers (oxLDL, MPO, LDH) that reflect redox imbalance. I discuss clinical tactics to improve mitochondrial biogenesis (SIRT1/3, AMPK, PGC-1α), repair membranes before pushing electron transport, enhance adiponectin while reducing leptin resistance, and personalize protocols by HRV-guided training and recovery. Finally, I translate complex mechanisms into relatable plans anchored in daily life—protein-forward meals, post-meal walks, structured training, environment control, stress rituals, and accountability—so that patients can sustain weight loss, stabilize glucose, and regain cognitive clarity.
This is not medical advice; it is an educational resource grounded in modern evidence, intended to help you collaborate with your medical providers and co-create personalized plans that respect your biology, context, and goals.
Foundations of Systems Biology in Metabolic Health — Understanding the Interconnected Axes
In my clinical approach, I start with the premise that metabolic health behaves as a multi-node network rather than a single switch. The physiology that drives weight change, energy level, mood, and long-term disease risk emerges from the interplay of distinct yet synchronized axes. When a patient asks, “Why am I gaining weight despite dieting and exercising?” I look across the network to identify mismatches between biological and behavioral processes. The traditional “eat less, move more” mantra often falls short because it addresses energy intake and expenditure without calibrating the underlying system.
- The systems model uses the concept of physiological axes to guide assessment:
- The Stress–Cortisol Axis: Chronic stress elevates cortisol and can flatten the diurnal rhythm. This dysregulation reduces insulin sensitivity, suppresses T4→T3 conversion, increases visceral adiposity, and heightens food salience under reward-seeking states.
- The Glucose–Insulin Axis: Frequent hyperglycemia/hyperinsulinemia impairs receptor sensitivity; hyperinsulinemia becomes a driver of fat storage, endothelial strain, and neurocognitive changes.
- The Thyroid Axis: Inflammation and nutrient deficits (selenium, zinc, iron) reduce deiodinase function and T3 activity at the tissue level, lowering mitochondrial throughput and energy.
- The Sex Hormone Axis: Post-menopausal declines in estradiol and altered testosterone availability change adiposity distribution, muscle protein synthesis, and mitochondrial density.
- The Circadian–Sleep Axis: Misalignment and sleep debt elevate appetite (ghrelin), dampen satiety (leptin), lower insulin sensitivity, and alter gut microbiome composition.
- The Immune–Inflammatory Axis: Cytokines (IL-6, TNF-α) and NF-κB activation blunt insulin receptor signaling (IRS-1/2), reduce GLUT4 translocation, and increase barrier permeability and systemic inflammation.
- The Mitochondrial Axis: Membrane integrity, electron transport chain efficiency, and mitochondrial biogenesis (regulated by SIRT1/3, AMPK, and PGC-1α) determine the balance between clean fuel utilization and ROS generation.
- The Nutrient Status Axis: Deficits in magnesium, chromium, zinc, B vitamins (especially B1), protein, vitamin D, and omega-3s impair enzymatic activity and signaling fidelity.
- The Microbiome–Gut Axis: Dysbiosis alters short-chain fatty acid production, incretin signaling, immune tone, and appetitive drive.
When someone transitions off GLP-1 receptor agonists, these axes must be protected proactively. Appetite signals rebound, stress rises, and if lean mass was lost during pharmacologic therapy, resting metabolic rate (RMR) drops—creating a physiologic pull toward rapid regain. The solution is multisystem: preserve lean mass, design meal structure, stabilize sleep and stress, and correct micronutrient deficits.
Why this works: tuning all axes simultaneously restores metabolic flexibility, enabling the body to use glucose and fat efficiently, maintain satiety signaling, and reduce inflammatory brake patterns on insulin receptors. This is the essence of systems biology care—interweaving physiology and life context to create durable outcomes.
Why “Eat Less, Move More” Fails After 30–40 — Physiological Shifts That Demand Precision
In the first decades of life, caloric restriction paired with activity improvements often yields noticeable results. But beyond age 30–40, physiology moves. Even without sharp changes in lifestyle, many adults notice weight creeping upward, energy thinning, and training that “doesn’t work as it used to.” Here’s why:
- Sarcopenia begins subtly: Without consistent resistance training and adequate protein, lean mass declines. Muscle is the largest glucose sink and a critical determinant of RMR. Lose muscle, and the caloric burn drops—making maintenance tougher even with similar intake.
- Hormonal transitions change the map: Declines in estradiol and shifts in testosterone affect adipose distribution, lipolysis, and muscle protein synthesis. These changes favor visceral fat, which is metabolically active and inflammatory.
- Sleep debt and circadian drift impair insulin sensitivity, elevate ghrelin levels to increase appetite, reduce leptin levels to reduce satiety, and destabilize energy rhythms. Night shift work or frequent late nights compounds these effects.
- Chronic stress flattens the cortisol curve: A high sympathetic tone raises food salience, increases cravings, lowers thyroid conversion, and distorts recovery. Many patients run high-intensity workouts while under-sleeping—fueling an overtrained, under-recovered physiology.
- Micronutrient deficits accumulate: Gradual shortfalls in magnesium, B1, zinc, chromium, vitamin D, and omega-3s impair receptor signaling and mitochondrial enzymes, diminishing response to diet and training.
Thus, a simple caloric deficit without systems support can produce paradoxical outcomes: weight plateaus, regain, fatigue, hair shedding, and mood volatility. The answer is not moral effort but precise physiology—protect muscle, align sleep, reduce stress, correct deficits, and modulate insulin dynamics while tailoring activity to recovery.
GLP-1 Physiology, Lean Mass Risk, and Exit Strategy — Designing Durable Outcomes

GLP-1 receptor agonists (e.g., semaglutide) reduce appetite, delay gastric emptying, and improve glycemic control—excellent tools within a comprehensive plan. Yet, risks arise when therapy occurs in isolation:
- Lean mass loss: Appetite suppression often reduces total intake and protein intake specifically. Without deliberate protein dosing (1.2–1.6 g/kg/day) and resistance training (2–4 sessions/week), patients lose lean mass, lowering RMR and increasing the likelihood of rebound.
- Stress and hunger rebound: Discontinuation can reactivate “food noise” and amplify cravings. Cortisol rises, insulin sensitivity dips, and satiety cues weaken—especially if sleep debt and high-intensity training persist.
- Nutrient gaps: Reduced intake can produce deficits (protein and micronutrients), leading to fatigue, hair thinning, poor recovery, and reduced detoxification capacity.
- GI adaptation: Changes in gastric emptying alter meal timing and tolerance. Reintroducing normal structure post-therapy requires gradual transitions, fiber, and gut support.
My GLP-1 exit strategy starts before therapy: protect lean mass, calibrate protein intake, build a stress-regulation plan, optimize sleep, and establish structured meals with fiber-rich foods. Post-therapy, we maintain protein targets, prioritize full-body strength (legs/posterior chain), fix meal timing, and use volumetric satiety foods (soups, salads, broths) to reduce hedonic overdrive. Monitoring lipase/amylase helps catch pancreatic stress early.
Why this works: lean mass preservation stabilizes RMR and glucose disposal; structured meals and micronutrient sufficiency restore satiety and energy; stress and sleep harmonization rebuild autonomic balance; and post-therapy hunger protocols prevent reward-driven relapse.
Clinical Decision-Tree Rubric for Comprehensive Weight Management — Precision Assessment
To aim interventions precisely, I use an integrated decision-tree. This rubric identifies dominant drivers and ensures coherence rather than scattershot fixes.
- History and Context
- Personal timeline: pregnancy, menopause/andropause, concussion or head trauma, sleep changes, night-shift work.
- Social determinants: family food culture (pizza nights, celebrations), childcare stressors, work demands, commute time, screen exposure.
- Coping patterns: smoking, alcohol, binge tendencies, reward-seeking behaviors, prior disordered eating. Not a moral judgment—physiology under stress seeks accessible dopamine.
- Traumatic stress: hypervigilance and emotional eating link; we consider counseling.
- Anthropometrics and Body Composition
- DEXA or bioimpedance for body fat percentage and lean mass; trends matter more than snapshots.
- Waist circumference, visceral adiposity indicators, and strength scores (functional capacity markers).
- Metabolic Labs
- Fasting glucose: incremental increases (e.g., 95→99 mg/dL) matter clinically; cohort data show that steps upward correlate with long-term diabetes risk.
- Fasting insulin, HOMA-IR, 1–2 hr postprandial glucose/insulin, fructosamine (short-term glycemic exposure).
- Lipids: triglycerides, HDL, LDL particle number/size, ApoB; Lp(a) if indicated.
- Inflammation: hs-CRP, ferritin patterns, homocysteine (methylation and vascular risk).
- Kidney: eGFR trends; early decline signals metabolic strain.
- Thyroid: TSH, free T4, free T3, reverse T3; antibodies if indicated.
- Sex hormones: estradiol, progesterone, testosterone, SHBG; DHEA-S as context.
- Nutrients: magnesium, zinc, chromium, B1 (thiamine), B12, folate, vitamin D, and omega-3 index.
- Liver: ALT/AST, GGT for steatosis patterns.
- Cortisol and Circadian Evaluation
- Salivary cortisol curve for flattening vs hypercortisolemia.
- Sleep architecture: duration, latency, awakenings; OSA screening when snoring or daytime sleepiness is present.
- Shift work: time meals/light exposure to reduce mismatch.
- Gut and Microbiome
- Symptoms: bloating, stool variability, and reflux.
- Consider stool testing for dysbiosis, calprotectin, and short-chain fatty acid production.
- Fiber intake and butyrate support via diet.
- Mitochondrial and Energy Utilization
- Subjective energy, post-exertional fatigue, and lactate patterns.
- Training tolerance and recovery markers: resting HR, HRV proxies for autonomic balance.
- Redox patterns and oxidative stress.
- Environmental Burden
- Potential exposures (arsenic, metals), endocrine disruptors, water/air quality, and occupational risks.
- Medications Review
- SSRIs (sertraline), antipsychotics, steroids, beta-blockers, antihistamines, contraceptives—evaluate metabolic impacts, consider alternatives with prescribers.
- Behavioral and Skills Assessment
- Cooking routines, meal planning, shopping, and food environment.
- Stress management, literacy, and social support.
- Exercise preferences, barriers, opportunities.
Why this works: the rubric illuminates root causes—insulin dynamics, inflammation, endocrine shifts, nutrient deficits, sleep/stress patterns, gut integrity, environmental exposures—so interventions become targeted, layered, and sustainable.
Stress, Cortisol, and Appetite (“Food Noise”) — How Autonomic Patterns Drive Eating Behavior
Patients pushing intense workouts on short sleep and high stress often report ravenous evening hunger and frustration. The physiology is straightforward:
- Cortisol elevation and curve flattening: Early high stress followed by persistent evening activation dampens diurnal oscillation. Over time, HPA axis resilience declines and the body maintains a “wired and tired” state—high sympathetic drive, low parasympathetic tone.
- Insulin sensitivity falls: Cortisol antagonizes insulin receptors; glucose remains elevated post-meal; insulin secretion rises to compensate, increasing adiposity risk.
- T4→T3 conversion drops: Stress reduces deiodinase activity, lowering tissue T3 levels; energy throughput declines, fat loss stalls.
- Enteric inflammation and permeability: Stress elevates gut cytokines and loosens tight junctions, increasing translocation and food sensitivity patterns; cravings intensify as the brain seeks quick dopamine relief.
- Reward pathway shifts: In low-reward states, food becomes accessible to dopamine. Ultra-processed, highly palatable foods hijack reward systems, increasing “food noise.”
Post-GLP-1, these effects can magnify: appetite returns, stress rises, and cravings escalate. My strategy depowers physiology triggers first—normalize sleep, enforce structured meals, prioritize protein and fiber, replete magnesium and other cofactors—and only then escalate exercise intensity with periodization.
Why this works: restoring autonomic balance reestablishes hormonal timing and appetite regulation; micronutrient sufficiency improves receptor fidelity; structured meals stabilize glycemia, reducing reward-driven seeking.
Glucose and Insulin Regulation — Central Levers for Weight, Longevity, and Vascular Health
Glucose and insulin dynamics sit at the heart of metabolic health. Cohort data show stepwise increases in fasting glucose predict long-term diabetes risk. Layering fasting insulin, HOMA-IR, and fructosamine sharpens risk estimation. Beyond numbers, mechanisms matter:
- Hyperinsulinemia drives fat storage, reduces insulin receptor density, and alters adipocyte biology.
- Postprandial spikes increase endothelial stress and cognitive fluctuations, reflecting microvascular strain and oxidative stress.
- Chronic exposure suppresses lipolysis, increases visceral fat, and distorts energy flux.
Clinical tactics:
- Protein-forward meals: Protein attenuates glycemic response and promotes muscle protein synthesis, supporting lean mass preservation.
- Carbohydrate quality: Choose fiber-rich, minimally processed carbs; pair with protein and healthy fats to slow absorption and reduce spikes.
- Meal timing: Consistent windows aligned to circadian cues reduce variability; avoid late-night eating to protect insulin sensitivity.
- Movement micro-bursts: 10–15 minutes of light walking after meals lowers postprandial glucose excursions.
Why this works: blunting spikes reduces oxidative stress and endothelial activation; protein preserves GLUT4 capacity in muscle; regular movement improves insulin signaling and glucose disposal.
Lean Mass Preservation — The Anchor of Long-Term Weight Maintenance and Metabolic Flexibility
I tell patients: you cannot see lean mass on a bathroom scale, but it is your metabolic bank account. Lose it, and the body wastes energy. GLP-1 therapy accelerates lean mass loss when protein is inadequate and strength training is absent.
- Protein targets:
- Aim for 1.2–1.6 g/kg/day for adults seeking fat loss while maintaining lean mass, or for those gaining lean mass. Higher ranges can be considered for older adults or those in aggressive training, tailored to kidney health.
- Distribute evenly across meals (roughly 25–40 g per meal, with leucine-rich sources) to maximize muscle protein synthesis.
- Resistance training:
- 2–4 weekly sessions focusing on compound lifts or bodyweight progressions (squats, deadlifts, presses, rows).
- Progressive overload and periodization tailored to recovery; track strength scores and energy to avoid overreaching.
- Mitochondrial support:
- Build aerobic base and strength to enhance mitochondrial biogenesis and substrate use.
- Avoid “biohack-only” approaches that focus solely on NAD+ without addressing membrane repair; combine nutrition, sleep, and progressive exercise for durable mitochondrial restoration.
Why this works: muscle increases basal energy consumption, stabilizes glucose, and raises RMR; training signals drive GLUT4 translocation and mTOR activation; adequate protein supports repair and enzymatic function.
Magnesium and Micronutrients — The Hidden Cofactors of Insulin Signaling and Energy Metabolism

In patients with metabolic disease, magnesium deficiency is common and consequential. It is essential for ATP-dependent enzymes, insulin receptor phosphorylation, and sleep quality. The literature consistently links magnesium insufficiency to impaired glucose regulation, hypertension, and adiposity.
- Magnesium supports enzymatic fidelity and reduces inflammatory tone; it often corrects subtle sleep fragmentation that undermines recovery and appetite regulation.
- Chromium enhances insulin receptor complex function and glucose handling.
- Zinc supports insulin storage and receptor function and is integral to thyroid conversion and immune balance.
- B1 (thiamine) is critical for carbohydrate metabolism; deficiency impairs pyruvate dehydrogenase, leading to increased lactate and fatigue.
- Vitamin D and omega-3 fatty acids modulate immune tone and insulin sensitivity.
- Protein—while a macronutrient—is functionally essential for lean mass, enzymes, transport proteins, and hormones.
Why this works: correcting micronutrient deficits restores intracellular signaling fidelity, improves mitochondrial enzymes, and stabilizes hormonal rhythms—enabling dietary and training strategies to produce their intended results.
Environmental Toxicants and Metabolic Burden — Metals, Endocrine Disruptors, and Hidden Roadblocks
Environmental exposures can derail metabolic regulation. In stubborn cases where behavior is strong but results lag, I screen for burden:
- Arsenic exposure is associated with insulin dysregulation and increased diabetes risk in some populations; water sources and occupational factors matter.
- Other metals can impair thyroid enzymes and mitochondrial function.
- Air and water quality elevate oxidative burden; filtration and remediation may be necessary.
Why this works: uncovering and addressing environmental load reduces inflammatory tone, protects endocrine axes, and restores mitochondrial throughput—unlocking progress when standard strategies stall.
Circadian Biology, Night Shift, and Meal Timing — Aligning Daily Rhythms to Metabolic Needs
We are circadian organisms. Night shift work disrupts hormonal timing, increases appetite, reduces insulin sensitivity, and alters microbiome composition. Perfect alignment may be impossible, but optimization within constraints matters:
- Anchored meals: Fix meal timing relative to sleep windows even on night shift; consistency reduces circadian mismatch.
- Light management: Bright light during the active phase; dim light before sleep; minimize blue light exposure in the pre-sleep window.
- Sleep hygiene: Dark, cool environments, pre-sleep routines, and noise reduction.
- Post-shift nutrition: Avoid large, high-carb meals immediately before sleep; favor protein and fiber earlier in the active period.
Why this works: stable timing helps synchronize peripheral clocks (pancreas, liver, adipose), improving insulin secretion rhythms, appetite cues, and energy regulation.
COVID-19, Cytokines, and Metabolic Shifts — Immune Perturbations and Recovery Strategies
Since COVID emerged, I have seen clinically significant shifts in metabolic tone among patients with previously stable health. Mechanisms likely include cytokine dysregulation, microbiome perturbations, and immune recalibration:
- Cytokine elevation increases insulin resistance and appetite dysregulation; hyperinflammatory states distort autonomic balance.
- Microbiome changes disrupt incretin signaling and short-chain fatty acid production, increasing gut permeability.
- Post-viral fatigue reduces exercise capacity; graded activity with careful recovery is required.
Clinical strategy: stabilize with sleep normalization, micronutrient sufficiency, low-inflammatory diets, gentle movement, and gut support. Build intensity gradually, guided by HRV, to avoid relapse.
Why this works: restoring immune balance reduces NF-κB activity, improves insulin signaling, and rebuilds training tolerance.
Medication-Induced Weight Gain — Understanding Drug Metabolic Signatures and Mitigation
Medications can influence weight and metabolic dynamics:
- SSRIs (e.g., sertraline): Some patients gain weight despite reduced intake; consider alternatives or mitigation strategies when appropriate.
- Antipsychotics, steroids, beta-blockers: Known metabolic impacts; evaluate necessity and dosing.
- Antihistamines: Sedation and appetite changes can drive intake.
- Contraceptives and hormone therapies: Affect fluid, fat distribution, and mood.
Why this works: collaborating with prescribers to choose metabolically friendlier options and implementing compensatory lifestyle tactics (protein-first meals, resistance training, sleep optimization) reduces downstream weight gain.
From Biohacking to Coherent Strategy — Building a Plan That Outlasts Trends
Patients arrive confused by disparate tactics: cold plunges, sauna, red light, NAD, fasting—stacked without sequence or rationale. While these tools have merit, the lack of a coherent plan leads to burnout. My framework anchors fundamentals first:
- Sleep and circadian alignment.
- Protein and micronutrient sufficiency.
- Progressive resistance and aerobic conditioning.
- Structured meal timing and glycemic management.
- Environmental hygiene.
Why this works: fundamentals build resilience. Once sleep, protein, and training consistency are established, add targeted supports (green tea extract, resveratrol, alpha-lipoic acid) based on labs and recovery metrics. Without foundations, advanced tactics yield inconsistent or transient results.
Building a Lifestyle That Keeps Weight Off — Habit Architecture and Environment Control

Nobody regrets maintaining results; frustration arises when weight rebounds. Maintenance requires embedding behaviors into daily routines:
- Habit architecture: Morning protein meals; scheduled training; pre-sleep wind-down; post-meal walks.
- Environment control: Pantry organization, meal prepping, grocery defaults, fast-food alternatives.
- Social support: family agreement on food culture, peer accountability, and community.
- Skill-building: Quick protein options, fiber-rich sides, batch cooking, travel strategies.
Relatable example: A parent wakes at 6 a.m., does 15 minutes of resistance band work, eats a 30 g protein breakfast, takes a 10–15 minute walk after lunch, and keeps dinner early with vegetables and lean protein. Over months, this steady structure beats sporadic boot camps.
Why this works: consistency beats intensity. Behavioral scaffolding reduces friction, prevents drift, and sustains physiologic alignment.
Post-Menopause and Andropause — The Inflammatory Shift and Metabolic Implications
After estradiol declines, cellular tone moves from anti-inflammatory to pro-inflammatory. Men may experience declining testosterone and changes in body composition. Both contexts elevate visceral adiposity risk and complicate weight loss.
Clinical adjustments:
- Higher protein intake to preserve lean mass.
- Resistance training emphasis to counter sarcopenia; full-body compound lifting with progressive overload.
- Omega-3 and polyphenol-rich diets reduce inflammatory tone and support endothelial function.
- Sleep support and stress regulation protect the cortisol rhythm.
- Careful evaluation of thyroid conversion and micronutrient status (selenium, zinc, iron).
Why this works: restoring anti-inflammatory balance and anabolic signaling rebuilds metabolic flexibility; muscle becomes a reliable glucose sink and supports bone via mechanical loading.
Reading the Data — Clinically Relevant Metrics and Thresholds for Decision-Making
Numbers guide interventions:
- Fasting glucose: incrementals (e.g., 95–99 mg/dL) are not benign when paired with elevated fasting insulin or fructosamine.
- Insulin: fasting and postprandial values contextualize glucose; high fasting insulin with normal glucose suggests early resistance.
- Triglycerides and HDL: high TG/low HDL patterns point to insulin resistance and poor lipid handling.
- eGFR: early declines signal metabolic stress; protect kidney microvasculature with glycemic stability and improved endothelial function.
- hs-CRP: persistent elevation reflects inflammatory burden and associates with vascular risk.
Why this works: Integrating metabolic, inflammatory, and functional markers yields a more accurate picture of disease trajectory—informing a more precise strategy and monitoring plan.
Lean Mass, Strength Scores, and Everyday Load — Integrating Movement into Daily Life
Strength scores quantify functional capacity—grip strength, squat depth, push capacity, and carry distance. I show patients how everyday tasks (pushing a lawn mower, carrying groceries, climbing stairs) can match or exceed gym exertion when leveraged intentionally.
- Increase step counts and embed micro-movements (stairs, walking errands).
- Use walking meetings and family walks to bond and move at the same time.
- Track simple performance markers to reinforce progress: more push-ups, longer carries, and a steadier heart rate during submaximal effort.
Why this works: integrating movement reduces the psychological barrier to exercise and smooths energy use across the day—shifting energy balance sustainably.
Functional Medicine’s Influence Beyond The Joints- Video
Transitioning Off GLP-1s — A Stepwise, Protective Plan
The GLP-1 exit period is vulnerable. My plan includes:
- Protein lock-in: Anchored at 1.2–1.6 g/kg/day before titrating down.
- Resistance training: 2–4 sessions/week, with leg and posterior chain emphasis to activate large muscle groups.
- Meal structure: Fixed times, balanced macros, and fiber-dense vegetables; avoid grazing.
- Stress modulation: Breathwork (box breathing or 4-7-8), mindfulness, and time in nature to reduce sympathetic drive.
- Sleep stabilization: 7–9 hours, consistent schedule, morning sunlight exposure.
- Micronutrients: Magnesium, chromium, zinc, B1, vitamin D, individualized to labs and clinical context.
- Cortisol mapping: Identify flattening; avoid high-intensity stacking under sleep debt; schedule recovery days.
- Hunger protocols: Volumetric foods; protein-first strategy; minimize ultra-processed reward foods; use soups and salads as satiety bridges.
- Support and tracking: Weekly check-ins, appetite journal, strength and energy metrics, lipase monitoring if indicated.
Why this works: lean mass protection stabilizes energy use; structured meals reduce variability and cravings; micronutrient sufficiency ensures enzymatic integrity; stress and sleep optimization restore autonomic balance; hunger protocols prevent reward-driven overeating.
Protein in Practice — Flexible, Real-Life Strategies for Satiety and Muscle
Not everyone wants meat thrice daily. I built flexible options:
- Greek yogurt bowls with seeds and berries (high-protein, probiotic support).
- Cottage cheese with tomatoes, olive oil, and herbs (protein and healthy fats).
- Plant protein blends (pea/rice) calibrated to leucine thresholds to trigger mTOR.
- Egg-based meals; tofu stir-fries; rotating fish/seafood for omega-3s.
- Legume soups and stews with lean proteins for satiety and fiber synergy.
Why this works: varied textures and cultural preferences improve adherence; protein-first structures glycemic response and support muscle protein synthesis while fitting diverse tastes.
Metaflammation, Adipose Biology, and Insulin Receptor Dynamics — Breaking the Feedback Loop
Adipose tissue is not inert; it is hormonally active:
- Inflammatory adipokines (TNF-α, IL-6) increase with visceral fat, impair insulin receptor signaling, promote serine phosphorylation of IRS-1/2, and reduce GLUT4 translocation.
- Leptin resistance blunts satiety and increases inflammatory tone.
- Adiponectin declines, reducing insulin sensitivity and endothelial protection.
Chronic hyperinsulinemia downregulates receptor density and function. Fat oxidation declines, glycolytic bias increases, and lactate rises—amplifying fatigue and limiting training tolerance.
We reverse this by:
- Reducing inflammatory load via anti-inflammatory nutrition (omega-3s, polyphenols).
- Improving mitochondrial function (aerobic base, resistance training, sleep).
- Aligning meal timing to reduce hyperinsulinemia and postprandial spikes.
Why this works: reducing cytokine activation improves receptor fidelity; mitochondrial improvements enhance oxidative capacity; meal timing stabilizes endocrine rhythms.
Detoxification Capacity and Oxidative Stress — Nutrient-Driven Repair for Hormonal and Metabolic Homeostasis
Liver function and phase I/II detox pathways affect metabolic stability. Insufficient glycine, sulfur-containing amino acids, B vitamins, and magnesium impair detoxification and increase oxidative stress, disrupting insulin receptor signaling and mitochondrial enzyme function.
Diet and lifestyle focus:
- Cruciferous vegetables, allium family (onions/garlic), protein sufficiency, and colorful polyphenols.
- Reduce alcohol excess; prioritize sleep; avoid unnecessary exposures.
Why this works: detoxification capacity lowers oxidative stress and inflammatory signaling, restoring receptor sensitivity and improving energy metabolism.
Metabolic Coaching — Translating Physiology into Daily Rituals
Willpower alone fails against physiology in a mismatch. We structure behaviors:
- Fixed breakfast: 30–40 g protein.
- Planned resistance training on set days; aerobic based on alternate days.
- 10–15 minute post-meal walks.
- Pre-commitments: grocery list defaults, meal prep routines.
- Stress rituals: 5-minute diaphragmatic breathing, brief journaling, sunlight breaks.
- If–then plans: “If late meeting → protein shake and nuts; if craving → volumetric soup first.”
Why this works: rituals create predictability; reducing friction increases adherence; physiology receives consistent energy and recovery cues.
Dopamine, Reward, and Non-Stigmatizing Strategies — Rewiring for Resilience
Some patients have lower basal dopamine tone or histories of compulsive behaviors. I approach this compassionately:
- Provide alternate dopamine sources: movement, sunlight, social connection, creative pursuits.
- Reduce exposure to ultra-processed foods that hijack reward pathways.
- Use consistent meal timing and protein-first strategies to blunt reward-driven hunger.
- Refer to counseling when trauma or compulsive patterns are present.
Why this works: reestablishing healthy reward circuits reduces reliance on food for dopamine; structured meals prevent crashes that trigger hedonic seeking.
Preventing Relapse After Goal Weight — Anchoring Maintenance to Physiology
Relapse is predictable if the plan ends at the goal. We pre-empt by:
- Scheduling maintenance training.
- Maintaining protein targets.
- Keeping meal timing constant.
- Monitoring stress and sleep.
- Refreshing micronutrients regularly.
- Sustaining community and accountability.
Why this works: the maintenance phase is a programmed state that protects lean mass, stabilizes hormones, and preserves glycemic control—preventing the slide that leads to regain.
Case-Based Scenarios — Translating Science into Real Lives
Composite examples illustrate the approach:
- Early-morning boot camper: Wakes at 4 a.m., trains hard, sleeps 6 hours, craves chips at night. We reduce intensity, move workouts later, increase protein, add magnesium, and anchor sleep. Food noise decreases; weight loss resumes.
- Post-GLP-1 transitioner: Stops medication; appetite surges; hair thinning from low protein. We lock protein at 1.4 g/kg/day, emphasize resistance training, structure meals, and supplement zinc and B vitamins. Lean mass stabilizes; maintenance holds.
- Night-shift nurse: Eats during circadian “night,” struggles with weight. We anchor meals to sleep, fix protein at the start of the active period, use light management, and post-meal walks. Insulin sensitivity improves; weight trends downward.
- Post-menopause professional: Belly fat and fatigue. We stabilize sleep, build resistance training, elevate omega-3s and magnesium, and monitor thyroid conversion and insulin. Visceral fat decreases; energy increases.
Why these work: personalized sequencing respects life context, physiological readiness, and recovery capacity—turning complex science into practical routines.
Practical Food and Movement Tactics — High-Impact, Low-Friction Strategies
- Pair carbohydrates with protein and fiber to blunt glycemic spikes.
- Build lunches around lean proteins plus large salads or vegetable soups.
- Add 10–15 minute walks after meals to lower postprandial glucose.
- Keep protein-forward snacks available (eggs, yogurt, shakes).
- Stack habits: combine family time with evening walks, use walking phone calls at work.
- Default dinners: fish or chicken, vegetables, and healthy fats.
Why this works: low-friction habits implemented daily outperform intermittent intensity; small steps compound into meaningful physiologic change.
Metaflammation and Integrated Clinical Strategies — Linking Inflammation to Metabolic Rigidity
I use the term metaflammation to describe persistent, low-grade inflammation driven by excess adiposity, stress, poor sleep, and environmental exposures. In adipose tissue, macrophage infiltration and cytokine signaling (IL-6, TNF-α) blunt IRS-1/2 and GLUT4 function—creating insulin resistance and metabolic rigidity. Endothelial dysfunction increases vascular risk; mitochondrial overload raises ROS, peroxidizes lipids (oxLDL), and fuels NF-κB.
Clinical markers:
- LDL particle size and number, oxLDL, MPO, and hs-CRP.
- LDH as a proxy for glycolytic bias and lactate.
- Ferritin/iron disparities reflecting hepcidin-mediated inflammation.
Interventions:
- Anti-inflammatory nutrition (Mediterranean-like patterns).
- Resistance training increases GLUT4 and improves insulin sensitivity; aerobic base enhances endothelial function.
- Sleep and stress regulation normalize cortisol curves, reducing inflammatory signaling.
Why this works: reducing inflammatory signaling restores receptor fidelity and mitochondrial efficiency—recovering metabolic flexibility and lowering disease risk.
Brown and Beige Fat Thermogenesis — Unlocking UCP1 to Raise Basal Expenditure
Adipose types differ:
- White adipose tissue (WAT) stores energy.
- Brown adipose tissue (BAT) contains abundant mitochondria and UCP1, enabling thermogenesis.
- Beige adipocytes (within WAT) can be induced to express UCP1 and become thermogenic in response to specific cues.
Many with obesity fail to recruit beige-to-brown transformation due to chronic inflammation, sympathetic dysregulation, low thyroid tissue activity, and inactivity. Enhancing thermogenesis increases basal energy expenditure, improves metabolic flexibility, and supports fat loss.
Strategies:
- Gentle, safe cold exposure (with clinician guidance).
- Resistance training and interval exercise to upregulate myokines.
- Optimizing thyroid status to improve mitochondrial biogenesis.
- Nutritional support for mitochondrial cofactors (iron, copper, coenzyme Q10, carnitine as indicated).
Why this works: thermogenesis increases energy expenditure independent of conscious effort, complements dietary changes, and improves glucose handling through enhanced mitochondrial oxidation.
Oxidative Stress and Redox Balance — Simple Assessments, Precision Interventions
Oxidative stress reflects an imbalance between ROS generation and antioxidant defenses. In insulin resistance, mitochondrial overload increases ROS, which damages lipids (oxLDL), proteins, and DNA, and fuels NF-κB.
Markers:
- Oxidized LDL, MPO, and hs-CRP.
- Elevated LDH suggesting glycolytic bias and lactate overflow.
Interventions should restore redox balance rather than over-supplement blindly:
- Dietary polyphenols (berries, olives, green tea).
- Adequate magnesium and B vitamins to support mitochondrial enzymes.
- Sequenced mitochondrial support (repair membranes first, then consider NAD+ strategies).
Why this works: targeted interventions lower the oxidative burden without prematurely pushing electron transport, reducing inflammatory signaling and restoring efficient energy production.
Thyroid and Testosterone Axes — Tissue-Level Metabolism and Mitochondrial Function
Normal TSH/T4 does not guarantee adequate tissue T3. Inflammatory cytokines and nutrient deficiencies reduce deiodinase activity, lowering intracellular T3 levels in muscle, adipose tissue, liver, and kidney. Clinically, this presents as fatigue, cold intolerance, poor recovery, and weight gain.
Similarly, low or suboptimal testosterone impairs lean mass accretion, reduces basal metabolic rate, decreases mitochondrial density, and limits lipolysis. Both axes influence IRS-1/2 signaling and GLUT4 trafficking.
Rationale for correction:
- Restoring physiologic T3 and testosterone levels improves mitochondrial biogenesis, oxidative capacity, and glucose disposal.
- Use evidence-based guidelines, monitor hematocrit and lipids, and integrate lifestyle supports (sleep, stress, resistance training).
Why this works: correcting endocrine insufficiencies removes systemic brakes on metabolic signaling, enabling the body to respond to nutrition and training.
Systems Biology Protocols — Sequencing Interventions for Maximum Impact
Sequencing matters. I structure protocols to prevent overload and maximize adaptation:
- Stabilize circadian rhythms: a consistent sleep-wake schedule and morning sunlight.
- Improve diet quality: fiber-rich, minimally processed foods; adequate protein and polyphenols.
- Initiate movement: resistance training first, then build aerobic base; add intervals only when readiness metrics (sleep, HRV) support.
- Repair membranes: targeted phospholipids for mitochondrial integrity.
- Support redox: magnesium, green vegetables, hydration; monitor morning urine pH trends with clinical oversight.
- Activate sirtuin/AMPK pathways: green tea extract, resveratrol, alpha-lipoic acid under clinician guidance.
- Personalize via labs: adjust thyroid, iron, vitamin D, and insulin markers.
- Evaluate medications: minimize metabolic side effects; mitigate with lifestyle and monitoring when pharmacologic changes are not possible.
Why this works: orderly sequencing respects cellular priorities—repair first, then upgrade signaling—producing stable, sustainable improvements.
Sleep, Stress, HRV, and Cortisol — Restoring Autonomic Balance for Metabolic Recovery
Stress physiology shapes insulin sensitivity and thyroid conversion. Autonomic balance and HPA axis function are foundational:
- Evaluate resting heart rate and HRV to gauge stress and recovery.
- Aim for 7–9 hours of restorative sleep; fragmented sleep is associated with metabolic dysregulation.
- Implement daily parasympathetic practices (meditation, diaphragmatic breathing, biofeedback).
- Align meal and alcohol timing with circadian rhythms; avoid late, heavy meals.
Why this works: parasympathetic dominance improves glucose control and recovery; sleep normalizes hormonal rhythms and reduces nocturnal cytokine surges.
Sarcopenia and Bone Loss — Muscle and Skeletal Health Across the Lifespan
Sarcopenia diminishes glucose disposal capacity and functional independence. Bone loss is increasingly observed in men and women, exacerbated by medications (PPIs, statins), low testosterone, stress, undernutrition, and low mechanical loading. Interventions include:
- DEXA scans when indicated.
- Protein sufficiency, vitamin D, calcium, and magnesium attention.
- Resistance and impact training to stimulate bone remodeling.
- Address malabsorption and endocrine issues.
Why this works: muscle and bone are linked through mechanical signals; building muscle preserves function, reduces fracture risk, and improves insulin sensitivity.
Iron–Ferritin Disparities and Hepcidin — Interpreting Inflammation’s Signature
Chronic inflammation modulates iron trafficking via hepcidin. Disparities (high iron/low ferritin or vice versa) reflect altered storage and mobilization. Iron is essential for deiodinase function and mitochondrial respiration; dysregulation of iron metabolism drives fatigue and cold intolerance.
Interventions:
- Treat root inflammatory drivers first.
- Assess for occult blood loss, malabsorption, or excessive supplementation.
- Replete iron only when indicated and safe; monitor to avoid oxidative stress.
Why this works: correcting iron handling improves thyroid conversion and oxygen transport, restoring energy and thermogenesis.
LDH, Glycolytic Bias, and the Warburg Lens — Metabolic Shifts in Health and Disease
Elevated LDH indicates glycolytic bias, which in oncology correlates with the Warburg effect. In non-cancer metabolic dysregulation, elevated LDH levels can reflect reduced mitochondrial oxidative capacity, overtraining, tissue injury, or inflammation.
Interventions:
- Aerobic base building and resistance training.
- Nutrient sufficiency (B vitamins, magnesium).
- Reducing inflammatory stress; improving sleep.
Why this works: restoring oxidative capacity reduces lactate overflow, improving endurance and recovery.
Urine pH, Renal Redox, and Practical Alkalinization — Tracking Trends with Clinical Oversight
Morning urine pH provides a low-cost window into systemic acid load and potential trends in oxidative stress. Persistently low values below 6.5 in diabetics can correlate with oxidative burden and microvascular stress.
Practical steps:
- Track morning pH with reliable strips; review patterns with your clinician.
- Increase dietary alkalinity via greens and mineral-rich foods.
- Focus on magnesium sufficiency and hydration.
- Medical strategies (e.g., sodium bicarbonate) are reserved for advanced disease under nephrology oversight.
Why this works: improved redox poise protects microvasculature and reduces renal stress; dietary shifts are foundational and safe when supervised.
Perfusion, Oxygen Delivery, and Microvascular Integrity — Lessons from Diabetes
Microvascular complications in diabetes (retinopathy, nephropathy, neuropathy) reveal the importance of oxygen delivery and endothelial health. Improving endothelial function via aerobic exercise, omega-3s, nitric oxide pathways, and glycemic variability reduction preserves capillary networks.
Why this works: mitochondrial integrity and thyroid sufficiency (tissue T3) enhance oxygen utilization; carnitine may assist fatty acid transport when indicated, but priority remains hormonal and mitochondrial repair.
Lifestyle Extremes — Overnutrition, Starvation, Alcohol, and Overtraining Risks
Extremes aggravate metaflammation:
- Severe caloric restriction leads to bone loss, menstrual disruption, thyroid suppression, and lean mass loss; it is counterproductive long-term.
- Overnutrition and ultra-processed foods elevate insulin and cytokines, overwhelm mitochondria, and promote fat storage.
- Alcohol patterns disrupt sleep and cortisol rhythms; dose matters even with “clean” spirits.
- Overtraining without adequate recovery increases cortisol, injury risk, and paradoxically worsens metabolic markers. HRV-guided training helps titrate load safely.
Why this works: avoiding extremes preserves hormonal balance, mitochondrial function, and reduces inflammatory burden—creating a hospitable environment for sustainable change.
Practical Protocol Highlights — Stepwise, Adaptable, Personalized
Nutrition:
- Whole-food patterns with high fiber and polyphenols.
- Protein balance is typically 1.2–1.6 g/kg/day in active individuals; adjust based on kidney function and goals.
- Distribute carbohydrates around training when insulin sensitivity allows; otherwise, lower glycemic load and adapt gradually.
Movement:
- Resistance training 2–3 days/week minimum, full-body compound lifts adjusted for joint health.
- Aerobic base 150–300 minutes/week, moderate intensity, progressing carefully.
- Interval work 1–2 days/week, only when sleep and HRV support readiness.
Recovery:
- Sleep 7–9 hours, consistent timing.
- Stress regulation daily (10–20 minutes).
- HRV monitoring to titrate training load and detect overreaching.
Lab-Guided Adjustments:
- If oxLDL and MPO are high, intensify anti-inflammatory diet, consider omega-3s, increase aerobic base, assess for sleep apnea when appropriate.
- For thyroid, address selenium, iron, iodine; adjust medications per guidelines.
- For testosterone, evaluate causes (sleep apnea, obesity, medications); prioritize lifestyle, then pharmacology when indicated and monitored.
Environmental:
- Screen for toxic metals when history suggests exposure; consider chelation/binding only under medical supervision.
- Improve indoor air quality and address occupation-specific risks.
Why this works: personalized dosing matches physiology and life context; stepwise escalation maintains safety and coherence.
Clinician’s Perspective — Iterative Care and Patient Empowerment
Care is a living process. Biomarkers guide us, but the lived experience—energy, mood, pain, sleep quality, performance, recovery—matters equally. Education empowers patients to understand the rationale behind interventions and carry them out consistently. We iterate based on feedback and labs, building momentum and resilience over time.
Why this works: optimally dosing interventions depends on real-time data from the body and life; patient understanding drives adherence and shared decision-making.
Summary
Metabolic health is a networked physiology that requires synchronized tuning across stress-cortisol rhythms, glucose-insulin dynamics, thyroid conversion, sex hormone transitions, immune-inflammatory signaling, mitochondrial capacity, circadian alignment, micronutrient sufficiency, gut integrity, and environmental hygiene. Metaflammation—low-grade, persistent inflammation—impairs IRS-1/2 and GLUT4 signaling, decreasing insulin sensitivity and pushing cells toward glycolysis and lactate overload. Adipose biology matters: inflamed, hypertrophic adipocytes produce IL-6 and TNF-α, reduce adiponectin, and fuel visceral fat accumulation, elevating cardiometabolic risk.
I use a systems biology decision-tree to personalize care: anthropometrics and body composition, fasting and postprandial glucose-insulin measures (HOMA-IR, fructosamine), lipid particle analysis (LDL-P, oxLDL, ApoB), inflammatory markers (hs-CRP, ferritin patterns), kidney and liver trends, thyroid and sex hormones, micronutrients (magnesium, B1, zinc, chromium, vitamin D, omega-3s), and gut health. Sleep architecture, HRV, and cortisol curves guide recovery and training dose; environmental exposures (arsenic, metals) and medications are explored for metabolic signatures.
For GLP-1 use and transitions, we mitigate risks by locking protein at 1.2–1.6 g/kg/day, emphasizing resistance training, structuring meals and fiber intake, stabilizing sleep and stress, and using hunger protocols that reduce ultra-processed reward-seeking. We monitor lipase/amylase for pancreatic stress and replete micronutrients to restore enzymatic fidelity. Thermogenic strategies (inducing beige/brown fat via UCP1) increase basal expenditure; mitochondrial improvement (repair membranes, then activate SIRT1/3–AMPK–PGC-1α) restores oxidative capacity. We reduce NF-κB activity and improve endothelial function through anti-inflammatory nutrition, sleep, and exercise.
Practical tactics include protein-first meals, post-meal walks, pantry control, travel strategies, and habit stacking. Maintenance plans prevent relapse by embedding routines—such as scheduled training, consistent meal timing, stress rituals, and community accountability. This approach is not a single “diet” but an iterative, personalized framework grounded in modern, evidence-based methods. By harmonizing physiology and life context, patients regain energy, cognitive sharpness, weight stability, and long-term cardiovascular and metabolic resilience.
Conclusion
Lasting metabolic health cannot be reduced to calorie arithmetic or isolated hacks. It is the outcome of coherent, systems biology care that restores signaling fidelity, mitochondrial function, hormonal orchestration, and circadian timing, while protecting muscle and microvasculature. By correcting micronutrient deficits, aligning sleep and stress, structuring meals to minimize glycemic volatility, and periodizing resistance and aerobic training, we re-enable insulin receptors and optimize fuel use. Thoughtful protocols for GLP-1 transitions—anchored in lean mass preservation and appetite regulation—ensure durable results. A compassionate, iterative partnership with patients, guided by data and practicality, transforms frustration into metabolic resilience and healthy aging.
Key Insights
- Lean mass preservation is the anchor of maintenance; protect it with adequate protein and progressive resistance training.
- Cortisol, insulin, thyroid conversion, and inflammatory signaling form an interconnected web; treat them together rather than piecemeal.
- Magnesium and key micronutrients are frequently deficient; repletion restores enzyme function, insulin signaling, sleep, and energy.
- Circadian alignment and quality sleep are essential; night shift requires tailored timing of meals, light exposure, and training.
- GLP-1 therapies must be embedded in whole-person plans; design the exit before the start to prevent rebound.
- Environmental exposures, medications, and microbiome shifts can stall progress; screen and address methodically.
- Consistency beats intensity; habit architecture and environment control sustain outcomes and prevent relapse.
References
- Hotamisligil GS. Inflammation, metaflammation, and immunometabolic disorders. Nature Reviews Immunology.
- Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. J Clin Invest.
- Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev.
- Petersen KF, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev.
- Ridker PM. hs-CRP in cardiovascular risk assessment. N Engl J Med.
- Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med.
- Pedersen BK. Muscles and myokines: endocrine functions of skeletal muscle. Nat Rev Endocrinol.
- Warburg O. On the origin of cancer cells. Science.
- Arnlov J et al. Low testosterone and cardiovascular risk. Circulation.
- Van Cauter E, Spiegel K. Sleep and metabolic regulation. Lancet.
- Chouchani ET, et al. Mitochondrial dysfunction in metabolic disease: mechanisms and therapeutics.
- Cantó C, Auwerx J. Targeting sirtuin-AMPK-PGC-1α axis to improve metabolism.
- Rosen ED, Spiegelman BM. Adipocyte biology and energy balance.
- Bass J, Lazar MA. Circadian rhythms and metabolic regulation.
- Turnbaugh PJ, et al. Microbiome in obesity and metabolic syndrome.
- Lean MEJ, et al. GLP-1 therapy and clinical monitoring.
- Esposito K, et al. Mediterranean diet and inflammation.
- Vlasova AN, et al. Maternal microbiome and infant immunity.
Keywords
Metaflammation; Insulin resistance; NF-κB; IL-6; TNF-α; Adiponectin; Leptin resistance; Brown fat; Beige fat; UCP1; GLUT4; IRS-1; IRS-2; Oxidative stress; OxLDL; MPO; hs-CRP; LDH; Warburg effect; Sarcopenia; Osteoporosis; Thyroid conversion; Testosterone; HRV; Cortisol; Sleep; Circadian rhythm; Systems biology; Functional medicine; Mitochondrial biogenesis; SIRT1; AMPK; PGC-1α; GLP-1 receptor agonists; Fructosamine; HOMA-IR; ApoB; eGFR; Magnesium; B1 (thiamine); Chromium; Zinc; Omega-3; Protein-first; Post-meal walking; Habit architecture; Environmental toxicants; Arsenic; Microbiome; Gut dysbiosis; Evidence-based weight management.
Disclaimers
This educational content is for informational purposes only and should not be used as medical advice.
All individuals must obtain recommendations for their personal situations from their own medical providers.