Functional Wellness Benefits Unpacked to Improve Autoimmune Conditions
Uncover the impact of autoimmune conditions using functional wellness on health and well-being with effective strategies.
Understanding Autoimmune Conditions: How Functional Wellness Can Transform Your Health
It can be hard to live with an autoimmune disease, but new research shows that functional wellness approaches can help you manage your symptoms and improve your quality of life. This complete guide covers how the immune system works, what happens when it doesn’t work properly, and how non-surgical treatments like chiropractic care and acupuncture, along with holistic approaches, can help you get your health and energy back.
Understanding Your Immune System: Your Body’s Defense Network
The immune system serves as your body’s primary defense mechanism, constantly working to protect you from harmful invaders such as bacteria, viruses, fungi, and parasites (Better Health Victoria, 1999; Medical News Today, 2025). This complex network consists of specialized cells, organs, proteins, and tissues that work together to keep you healthy and functioning optimally.
The Components of Your Immune System
Your immune system includes several key components that work together seamlessly. White blood cells, also called leukocytes, are key players in immune defense (Better Health Victoria, 1999). These cells move through blood and tissue throughout your body, constantly searching for foreign invaders. When they detect threats, they launch an immune attack to protect your health.
The bone marrow produces red blood cells that carry oxygen, white blood cells that fight infection, and platelets that help blood clot (Better Health Victoria, 1999). The thymus filters and monitors blood content while producing specialized white blood cells called T-lymphocytes (Better Health Victoria, 1999). The lymphatic system, a network of delicate tubes throughout the body, manages fluid levels, responds to bacteria, removes cancer cells, and absorbs fats from the intestine (Better Health Victoria, 1999).
How the Immune System Works
The immune system operates through two subsystems: the innate and adaptive immune systems (NCBI, 2023). The innate immune system provides general defense against harmful germs and substances using immune cells such as natural killer cells and phagocytes. The adaptive immune system creates specific responses to particular invaders, helping the body remember and recognize previous threats.
B lymphocytes produce antibodies and help alert T lymphocytes (Medical News Today, 2025). These antibodies are special proteins that lock onto specific antigens, marking them for destruction. T lymphocytes destroy compromised cells in the body and help alert other leukocytes (Medical News Today, 2025). Helper T cells coordinate the immune response by communicating with other cells, while killer T cells attack infected cells directly.
When functioning properly, the immune system can distinguish healthy tissue from unwanted substances (Medical News Today, 2025). If it detects an undesirable substance, it mounts an immune response—a complex attack to protect the body from invaders. This remarkable system enables your body to defend itself while maintaining normal function.
The Critical Role of Inflammation in Health and Disease
Inflammation represents the body’s natural response to injury, infection, or harmful stimuli. While acute inflammation serves as a protective mechanism, chronic inflammation can contribute to numerous health problems, including autoimmune conditions (Frontiers in Immunology, 2023).
Understanding the Inflammatory Process
When your body experiences external adverse stimuli, it triggers innate immunity and inflammation, followed by adaptive immunity (Frontiers in Immunology, 2023). This process involves the release of inflammatory mediators, including cytokines and inflammasomes, which play important roles in mediating immune responses through innate cells such as macrophages and adaptive cells such as T and B cells (Frontiers in Immunology, 2023).
Pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 promote inflammation, while anti-inflammatory cytokines work to resolve it. The balance between these opposing forces determines whether inflammation helps or harms the body. In autoimmune diseases, this balance becomes disrupted, leading to persistent inflammation that damages healthy tissues.
Inflammation and Immune System Dysfunction
The relationship between inflammation and the immune system is bidirectional and complex. IL-1β, a key inflammatory cytokine, affects both innate and adaptive immunity (Frontiers in Immunology, 2023; PMC, 2023). As an inflammatory driver, IL-1β can lead to innate immune abnormalities, resulting in autoinflammation. It can also increase T and B cell proliferation, potentially leading to autoimmune diseases when this process becomes excessive (Frontiers in Immunology, 2023).
Long-term stimulation of innate inflammation contributes to abnormal activation and infiltration of T and B cells, disrupting immune tolerance and leading to autoantibody production (PMC, 2023). This results in autoimmunity that aggravates tissue damage and inflammation. The microenvironment balance of pro-inflammatory and anti-inflammatory cytokines is closely associated with autoimmune diseases, particularly rheumatoid arthritis, inflammatory bowel disease, and systemic lupus erythematosus (Frontiers in Immunology, 2023).
What Are Autoimmune Conditions?
Autoimmune conditions occur when your immune system mistakenly attacks your own healthy cells and tissues, viewing them as foreign invaders (Healthdirect, 2025; Carey, n.d.). This immune system dysregulation can lead to a wide range of symptoms and health complications affecting various organs and systems throughout the body.
The Scope of Autoimmune Diseases
More than 80 autoimmune diseases have been identified, affecting an estimated 50 million people in the United States (Rupa Health, 2025; Performance Health and Wellness, 2025). An additional 8 million people have autoantibodies, indicating an increased risk of developing autoimmune conditions (Rupa Health, 2025).
Women are disproportionately impacted by autoimmune conditions, with estimates suggesting that approximately 75% of those affected are female (Carey, n.d.). This gender disparity highlights the complex interplay between hormones, genetics, and immune function in autoimmune disease development.
Common Types of Autoimmune Disorders
- Rheumatoid arthritis ranks among the most prevalent autoimmune disorders affecting women, characterized by joint inflammation (Carey, n.d.). This condition leads to joint pain and stiffness, along with fatigue and general malaise. The inflammatory process can damage cartilage and bone, potentially causing permanent joint deformity if left untreated.
- Lupus is a multifaceted autoimmune condition that can affect organs such as the skin, kidneys, and heart (Carey, n.d.). Women with lupus often experience flare-ups triggered by stress, sun exposure, or infections. The disease can cause a characteristic butterfly-shaped rash across the face, along with fatigue, fever, joint pain, and organ damage (Mayo Clinic, 2022).
- Multiple sclerosis (MS) predominantly affects women, leading to neurological symptoms as the immune system attacks the protective covering of nerves (Carey, n.d.). Women with MS may experience fatigue, weakness, and cognitive changes. The disease progresses differently in each person, with some experiencing relapsing-remitting patterns while others face progressive decline.
- Hashimoto’s thyroiditis affects the thyroid gland, leading to hypothyroidism (Carey, n.d.). Symptoms include fatigue, weight gain, depression, and cold sensitivity (Medical News Today, 2023). This autoimmune condition can significantly impact energy levels, metabolism, and overall quality of life.
Other common autoimmune conditions include Crohn’s disease, ulcerative colitis, celiac disease, psoriasis, and type 1 diabetes. Each condition presents unique challenges, but they share common underlying mechanisms of immune dysfunction and inflammation.
Causes and Risk Factors
The exact cause of autoimmune conditions remains largely unknown, though research points to a combination of genetic, environmental, and hormonal factors (Carey, n.d.). For women, hormonal fluctuations throughout life—during menstruation, pregnancy, and menopause—can influence the onset and exacerbation of symptoms.
Environmental factors such as stress, diet, chemical exposure, and infections may trigger or worsen autoimmune conditions (Carey, n.d.). The gut microbiome also plays a crucial role, with dysbiosis linked to numerous autoimmune diseases (Oxford Academic, 2024; Frontiers in Microbiomes, 2025). Understanding these contributing factors empowers individuals to take proactive steps in managing their health through lifestyle choices and therapies that promote balance and wellness.
Symptoms and Effects of Autoimmune Conditions on the Body
Autoimmune conditions can cause a wide range of symptoms that vary significantly between individuals and conditions. The effects can be mild or severe, intermittent or constant, and can profoundly affect quality of life.
Common Systemic Symptoms
Fatigue stands as one of the most common and debilitating symptoms across autoimmune conditions (Healthdirect, 2025; Global Autoimmune Institute, 2025). This overwhelming tiredness doesn’t improve with rest and can interfere with daily activities, work, and relationships. The chronic nature of autoimmune-related fatigue stems from the ongoing inflammatory process and the energy demands placed on the immune system.
Fever and low-grade elevations in body temperature frequently accompany autoimmune conditions, reflecting the body’s inflammatory state (Healthdirect, 2025; Global Autoimmune Institute, 2025). These temperature fluctuations can occur during disease flares or persist chronically, contributing to overall malaise.
Many people with autoimmune diseases experience swollen glands, indicating immune system activation (Healthdirect, 2025; Global Autoimmune Institute, 2025). Lymph nodes may become enlarged and tender as they work to filter inflammatory substances and immune cells.
Musculoskeletal Manifestations
Joint pain, stiffness, and swelling are common features of many autoimmune conditions, particularly rheumatoid arthritis and lupus (Healthdirect, 2025; Medical News Today, 2023). Morning stiffness lasting more than 30 minutes is characteristic of inflammatory arthritis and distinguishes it from osteoarthritis. The inflammatory process can damage joints over time, leading to deformity and disability if left unmanaged.
Muscle aches, pain, and weakness are frequently associated with autoimmune diseases (Global Autoimmune Institute, 2025). This myalgia can be widespread or localized, and its intensity can fluctuate. Some conditions, such as polymyositis and dermatomyositis, specifically target muscle tissue, leading to progressive weakness.
Bone pain and inflammation may occur in conditions like ankylosing spondylitis, which primarily affects the spine and sacroiliac joints (Global Autoimmune Institute, 2025). Over time, this can lead to fusion of vertebrae and reduced spinal mobility.
Neurological Symptoms
Brain fog and cognitive difficulties represent common complaints among people with autoimmune diseases (Global Autoimmune Institute, 2025). This mental cloudiness affects concentration, memory, and mental clarity, significantly impacting work performance and daily functioning. The neuroinflammation associated with autoimmune conditions contributes to these cognitive symptoms. Numbness and tingling in the arms and legs, particularly in multiple sclerosis, result from nerve damage (Tri-State Arthritis, 2025; Global Autoimmune Institute, 2025). These sensory disturbances can range from mild tingling to complete numbness, affecting mobility and safety.
Headaches and migraines occur more frequently in many autoimmune conditions (Global Autoimmune Institute, 2025). The inflammatory processes and vascular changes associated with these diseases can trigger severe headaches that resist conventional pain management. Dizziness, balance difficulties, and vision changes affect some patients with autoimmune conditions, particularly those with MS or lupus (Global Autoimmune Institute, 2025; Mayo Clinic, 2022). These symptoms can increase fall risk and limit independence.
Digestive Manifestations
Abdominal pain, bloating, and digestive issues commonly affect people with autoimmune conditions, especially those involving the gastrointestinal tract, like Crohn’s disease and ulcerative colitis (Global Autoimmune Institute, 2025). Symptoms may include diarrhea, constipation, blood in stool, nausea, and vomiting. Food sensitivities and intolerances frequently develop in autoimmune conditions (Global Autoimmune Institute, 2025). Gut inflammation and increased intestinal permeability can trigger reactions to foods previously well tolerated, necessitating dietary modifications.
Malabsorption and nutrient deficiencies can result from chronic gut inflammation (Global Autoimmune Institute, 2025). This can lead to anemia, vitamin deficiencies, and unintended weight loss, further complicating health management.
Skin and Other Symptoms
Rashes and skin lesions are characteristic of many autoimmune conditions (Global Autoimmune Institute, 2025; Mayo Clinic, 2022). Lupus causes the characteristic butterfly rash across the cheeks and nose, while psoriasis produces scaly, inflamed patches. These visible symptoms can significantly impact self-esteem and quality of life.
Temperature sensitivity, whether to heat or cold, affects many autoimmune patients (Global Autoimmune Institute, 2025). Raynaud’s phenomenon, common in lupus and scleroderma, causes fingers and toes to change color and become painful in response to cold or stress.
Shortness of breath and chest pain may indicate autoimmune involvement of the lungs or heart (Global Autoimmune Institute, 2025; Mayo Clinic, 2022). These serious symptoms require immediate medical attention to prevent complications.
The wide-ranging effects of autoimmune conditions underscore the need for comprehensive, holistic management approaches that address multiple body systems and symptoms simultaneously.
The Functional Wellness Approach to Autoimmune Management
Traditional medical management of autoimmune diseases typically relies on immunosuppressants, corticosteroids, or biologic medications (Performance Health and Wellness, 2025). While these interventions can help manage flare-ups, they don’t address the underlying cause of the immune system’s overactivity. Functional wellness offers a different paradigm—one that seeks to identify and address root causes rather than simply suppressing symptoms.
The Functional Medicine Philosophy
Functional medicine approaches autoimmune conditions by investigating why the immune system is misfiring (Performance Health and Wellness, 2025). This comprehensive approach integrates nutrition and lifestyle medicine, advanced lab testing, gut microbiome analysis, personalized supplementation, and environmental toxin evaluation (Performance Health and Wellness, 2025).
The goal extends beyond symptom relief to achieving long-term immune regulation and remission (Performance Health and Wellness, 2025). Functional medicine doesn’t view the body as broken but as imbalanced, aiming to restore balance at the source through personalized interventions based on individual health profiles, genetics, lifestyle, lab data, environment, stress history, and microbiome status (Performance Health and Wellness, 2025; Integrative Medicine AZ, 2022).
Key Focus Areas in Functional Wellness
- Gut Health Restoration: The gut plays a central role in immune system regulation, with 70-80% of immune cells residing in gut-associated lymphoid tissue (Frontiers in Microbiomes, 2025; PMC, 2019). Gut dysbiosis—an imbalance in the gut microbiome—is consistently associated with autoimmune conditions, including rheumatoid arthritis, multiple sclerosis, and type 1 diabetes (Frontiers in Microbiomes, 2025; Oxford Academic, 2024).
- Functional medicine practitioners use the “4R” approach to restore gut health: Remove inflammatory foods and hidden infections; Replace digestive enzymes and stomach acid; Reinoculate with probiotics and prebiotics; and Repair the intestinal lining with nutrients like L-glutamine, zinc, and collagen (Performance Health and Wellness, 2025). Studies have found that correcting gut permeability reduces symptoms in autoimmune patients, including those with Crohn’s disease and Hashimoto’s thyroiditis (Performance Health and Wellness, 2025).
- Inflammation Reduction: Chronic inflammation serves as the engine of autoimmune disease (Performance Health and Wellness, 2025). Anti-inflammatory strategies include removing reactive foods like gluten, dairy, and refined sugar; balancing omega-3 to omega-6 fatty acid ratios; supporting detoxification pathways; addressing sleep and stress; and adding targeted anti-inflammatory nutrients like turmeric, omega-3s, quercetin, and resveratrol (Performance Health and Wellness, 2025).
- Clinical trials demonstrate that anti-inflammatory diets can significantly reduce disease activity in patients with rheumatoid arthritis and lupus (Performance Health and Wellness, 2025; PMC, 2024). The Mediterranean diet, characterized by high consumption of fruits, vegetables, whole grains, legumes, fatty fish, nuts, olive oil, and phytochemicals, has shown particular promise in modulating immune responses (PMC, 2024).
- Personalized Nutrition: Functional medicine recognizes that individual responses to foods vary significantly. Customized nutrition plans eliminate potential inflammatory foods while increasing intake of anti-inflammatory foods rich in omega-3 fatty acids, antioxidants, and phytonutrients (Flourish Counseling MD, 2025). Functional stool testing and food sensitivity analysis help guide this process for each patient (Performance Health and Wellness, 2025).
- Stress Management: Chronic stress exacerbates autoimmune conditions by increasing inflammation and disrupting immune function (Flourish Counseling MD, 2025; MGI Clinic, 2025). Stress management techniques like mindfulness meditation, yoga, and biofeedback help reduce stress and its impact on the body (Flourish Counseling MD, 2025).
- Lifestyle Modifications: Simple changes in daily routines can profoundly affect the management of autoimmune diseases (Flourish Counseling, MD, 2025). This includes optimizing sleep patterns, engaging in regular physical activity, and adopting habits that promote overall well-being (Flourish Counseling MD, 2025).
Chiropractic Care: Aligning Your Body for Optimal Health
Chiropractic care offers a supportive role in managing autoimmune conditions by promoting nervous system balance and reducing inflammation (Chiro CT, 2025). While not a cure, these treatments may alleviate pain, fatigue, and joint stiffness, improving overall quality of life (Chiro CT, 2025; Atlas Chiropractic, 2024).
How Chiropractic Care Supports Autoimmune Management
- Improves Nervous System Function: Chiropractic care primarily focuses on optimizing the nervous system, which is closely connected to the immune system (Atlas Chiropractic, 2024). Proper spinal alignment can enhance nerve function, improving communication between the immune system and the rest of the body, thereby supporting more balanced immune responses (Atlas Chiropractic, 2024; Anchor to Health, 2023). By manipulating the spine, chiropractors can improve communication between the central nervous system and the immune system (Anchor to Health, 2023). This enhanced communication may lead to improved healing, reduced symptoms, and reduced pain throughout the day.
- Reduces Inflammation: Autoimmune conditions often involve chronic inflammation, which can lead to pain and tissue damage (Atlas Chiropractic, 2024). Chiropractic adjustments and therapies can help reduce inflammation by promoting better circulation and facilitating the body’s natural healing processes (Atlas Chiropractic, 2024). This provides relief from discomfort and may reduce the severity of autoimmune flare-ups.
- Improves Mobility and Joint Function: Joint stiffness and pain are common in individuals with autoimmune conditions, leading to decreased mobility and quality of life (Atlas Chiropractic, 2024). Chiropractic care can improve joint function and increase range of motion through gentle manipulations and targeted exercises, helping patients maintain flexibility and independence (Atlas Chiropractic, 2024; Anchor to Health, 2023).
Chiropractic manipulations often improve the range of motion throughout many joints of the body (Anchor to Health, 2023). As a result, patients who receive these treatments regularly can usually move more fluidly than before. Because many autoimmune disorders directly or indirectly cause movement dysfunction, this represents a huge benefit.
- Reduces Stress: The impact of stress on autoimmune conditions cannot be overstated; it can exacerbate symptoms and trigger flare-ups (Atlas Chiropractic, 2024). Chiropractic treatments, including spinal adjustments and massage therapy, can have a calming effect on the nervous system, reducing stress levels and potentially mitigating the impact of stress on autoimmune conditions (Atlas Chiropractic, 2024).
- Improves Sleep Quality: Sleep disturbances are common among individuals with autoimmune conditions, often due to pain or discomfort (Atlas Chiropractic, 2024). By addressing spinal misalignments and reducing pain and tension in the body, chiropractic care can help improve sleep quality, which is crucial for the body’s healing processes and overall health (Atlas Chiropractic, 2024).
- Enhances Overall Quality of Life: By addressing various symptoms associated with autoimmune conditions, such as pain, inflammation, and stress, chiropractic care can significantly improve patients’ quality of life (Atlas Chiropractic, 2024). This allows them to engage more fully in daily activities and enjoy a greater sense of well-being.
Chiropractic BioPhysics® for Autoimmune Conditions
Chiropractic BioPhysics® (CBP) represents an evidence-based corrective care technique particularly helpful for people living with autoimmune disorders (IdealSpine, 2023). CBP focuses on restoring alignment to the spine using mirror-image® adjustments and spinal traction, designed to realign the spine to reduce pain and inflammation caused by autoimmune diseases (IdealSpine, 2023). Studies show that CBP is effective at reducing inflammation and easing muscle tension, which are often associated with autoimmune diseases (IdealSpine, 2023). In addition to relieving physical discomfort, CBP has been found to reduce psychological stress related to chronic illness, further helping people cope better with their condition and improving overall quality of life (IdealSpine, 2023).
CBP addresses the entire neuromusculoskeletal system, treating three systems simultaneously: the nervous, muscular, and skeletal systems (IdealSpine, 2023). By treating these three major body systems, CBP can significantly reduce inflammation, pain, and other symptoms associated with autoimmune disorders.
Dr. Alexander Jimenez’s Integrative Approach to Autoimmune Care
Dr. Alexander Jimenez, DC, APRN, FNP-BC, brings a unique dual perspective to the management of autoimmune diseases at his El Paso practice. As both a licensed chiropractor and board-certified Family Practice Nurse Practitioner, Dr. Jimenez offers comprehensive treatment protocols that bridge physical medicine, functional medicine, and advanced diagnostics (A4M, 2016; Dr. Alex Jimenez, 2025).
Dr. Jimenez’s Credentials and Philosophy
With over 25 years of expertise, Dr. Jimenez has been consistently voted El Paso’s top chiropractor from 2015 through 2024 (LinkedIn, 2024; Dr. Alex Jimenez, 2025). His dual licensure as both a chiropractor and nurse practitioner provides unique insights into the etiologies, pathogenesis, and treatment of complex clinical conditions (A4M, 2016).
As an IFMCP (Institute for Functional Medicine Certified Practitioner) and CFMP, Dr. Jimenez evaluates health comprehensively, addressing physical, nutritional, and emotional factors (Dr. Alex Jimenez, 2025). His practice stands out for integrating the biomechanical focus of chiropractic care with a nurse practitioner’s diagnostic and therapeutic scope (A4M, 2016).
The Injury Medical & Chiropractic Clinic Approach
Dr. Jimenez’s Injury Medical & Chiropractic Clinic serves as El Paso’s largest mobility, flexibility, and agility center (A4M, 2016). The clinic’s multidisciplinary team includes chiropractors, nurse practitioners, registered nurses, nutritionists, and physical performance trainers who collaborate to deliver personalized care (A4M, 2016).
As a chiropractor, Dr. Jimenez specializes in restoring musculoskeletal function, particularly after trauma, neck, back, and spine injuries, and soft-tissue injuries (A4M, 2016). His chiropractic interventions emphasize non-invasive techniques such as spinal decompression, manual adjustments, and functional rehabilitation to alleviate pain and enhance mobility (A4M, 2016).
As a board-certified nurse practitioner, Dr. Jimenez employs evidence-based medicine to address systemic and metabolic dysfunctions (A4M, 2016). His expertise extends to managing chronic degenerative disorders, hormonal imbalances, weight management, and pain syndromes. This dual perspective allows him to identify underlying disease causes—from biomechanical misalignments to physiological imbalances—and design treatment regimens that address both symptoms and root causes (A4M, 2016).
Clinical Correlations: Integrative Medicine in Practice
Dr. Jimenez’s clinical observations demonstrate the power of combining chiropractic care with integrative medicine for patients with autoimmune conditions. His approach recognizes that autoimmune conditions often stem from multiple contributing factors requiring multifaceted solutions.
The synergy of chiropractic and functional medicine roles enables Dr. Jimenez to offer a holistic approach, particularly effective for complex conditions such as chronic pain, fibromyalgia, and inflammatory disorders (A4M, 2016). His integrative protocols combine functional medicine assessments, lifestyle interventions, and advanced diagnostics to achieve homeostasis and physiological balance (A4M, 2016).
Dr. Jimenez emphasizes addressing the root causes of injury and illness rather than merely treating symptoms. By identifying biomechanical dysfunctions, nutritional deficiencies, inflammatory triggers, and lifestyle factors, he helps patients achieve lasting improvements in health (A4M, 2016; Dr. Alex Jimenez, 2025).
Enhancing Health Through Targeted Interventions
Dr. Jimenez’s clinical correlation extends to understanding how different therapeutic modalities work synergistically. He integrates targeted exercise programs designed to strengthen vulnerable areas, improve mobility, and prevent long-term problems (A4M, 2016). These exercise prescriptions are tailored to each patient’s specific condition, fitness level, and functional goals.
Massage therapy forms another key component of Dr. Jimenez’s integrative approach. He recognizes that therapeutic massage can reduce muscle tension, improve circulation, reduce inflammation, and promote relaxation—all of which are crucial for managing autoimmune-related pain and stiffness (A4M, 2016).
Acupuncture represents yet another tool in Dr. Jimenez’s comprehensive treatment arsenal. By incorporating this ancient healing practice, he helps patients modulate immune function, reduce inflammation, and alleviate pain through mechanisms distinct from but complementary to chiropractic adjustments (A4M, 2016).
Patient-Centered Care and Education
Dr. Jimenez’s commitment to patient education sets his practice apart. His comprehensive website, dralexjimenez.com, offers evidence-based information on health conditions, treatment options, and wellness strategies (A4M, 2016). By fostering health literacy, Dr. Jimenez enables patients to make informed decisions and take charge of their well-being.
The practice accepts major insurances, including Aetna, Blue Cross Blue Shield, Cigna, and First Health, making integrative care accessible to a broad patient base (A4M, 2016). Patients can visit in person at 11860 Vista Del Sol, Suite 128, El Paso, TX 79936, or engage through telehealth consultations (A4M, 2016).
Dr. Jimenez’s functional medicine series educates patients on holistic health principles, covering topics such as spinal health and metabolic optimization (A4M, 2016). This educational focus empowers patients to become active participants in their healing journey rather than passive recipients of care.
Through his dual expertise and integrative philosophy, Dr. Jimenez demonstrates how combining chiropractic care, functional medicine, targeted exercise, massage therapy, and acupuncture can address the complex needs of patients with autoimmune conditions, promoting natural healing and preventing long-term complications.
Acupuncture: Ancient Wisdom for Modern Autoimmune Challenges
Acupuncture, a traditional Chinese medicine practice with over 2,000 years of history, has gained recognition for its potential benefits in managing autoimmune disorders (Carey, n.d.; PubMed, 2025). This ancient healing modality offers a unique approach to restoring balance and supporting immune health.
The Mechanisms Behind Acupuncture’s Effectiveness
The fundamental principle of acupuncture centers on Qi (pronounced “chee”), the vital life force that flows through the body along specific pathways known as meridians (Carey, n.d.). When this flow becomes disrupted, it can lead to imbalances and health issues. By inserting thin needles into strategic points along these meridians, acupuncture aims to restore Qi balance, promoting overall health and wellness.
Research supports acupuncture’s efficacy in modulating the immune system, particularly relevant for those dealing with autoimmune disorders (Carey, n.d.; PubMed, 2025). Acupuncture can activate the vagal-adrenal axis, resulting in decreased systemic inflammation (QJM, 2024; PubMed, 2025). Studies indicate that acupuncture may help reduce inflammation and regulate immune responses, potentially leading to fewer flare-ups and improved quality of life (Carey, n.d.).
Evidence-Based Benefits for Autoimmune Conditions
A comprehensive narrative review of experimental and clinical evidence for acupuncture in autoimmune diseases, based on randomized controlled studies, systematic reviews, and meta-analyses from 2000 to 2023, revealed significant findings (PubMed, 2025). Acupuncture in experimental models of rheumatoid arthritis, multiple sclerosis, psoriasis, and ulcerative colitis downregulated inflammatory cytokine expression, increased IL-10 expression, improved regulatory T-cell differentiation, and modulated macrophage polarization (PubMed, 2025).
The anti-inflammatory effect of acupuncture in autoimmune disorders has been demonstrated to involve vagal-adrenal and cholinergic anti-inflammatory pathways (PubMed, 2025). The analgesic effect involves both peripheral and central anti-nociceptive mechanisms (PubMed, 2025).
Randomized controlled studies support the use of acupuncture in rheumatoid arthritis, fibromyalgia, Crohn’s disease, and Sjögren’s syndrome (PubMed, 2025). Evidence indicates that acupuncture may benefit as a symptomatic treatment for multiple sclerosis, myasthenia gravis, psoriasis, and ankylosing spondylitis (PubMed, 2025).
Immune Modulation and Regulation
One of the primary benefits of acupuncture involves its ability to modulate the immune system (Carey, n.d.). Autoimmune diseases often result from an overactive immune response where the body mistakenly attacks its own tissues. Acupuncture helps restore balance by stimulating the production of regulatory T cells, which play a crucial role in controlling immune responses (Carey, n.d.).
This regulation can reduce symptom severity and flare-ups associated with conditions such as rheumatoid arthritis, lupus, and multiple sclerosis (Carey, n.d.). Studies have shown that acupuncture can reduce antibody levels and decrease cytokine production—chemical messengers that can worsen autoimmune symptoms (Dr. Guan PTAP, 2023).
Acupuncture has the potential to regulate inhibition in the management of certain hyperimmune diseases by modulating Th1, Th2, and Th17 immunity and regulatory T-cell homeostasis, thereby restoring immune homeostasis (QJM, 2024). Research found that needling at acupoint ST36 can activate corticotropin-releasing hormone neurons in experimental models and significantly reduce signs of disease and demyelination while restoring the balance of Th1/Th2/Th17/Treg cellular responses (QJM, 2024).
Reducing Inflammation
In addition to immune modulation, acupuncture has been shown to reduce inflammation, a common feature of autoimmune conditions (Carey, n.d.; PubMed, 2025). Inflammation contributes to pain, fatigue, and other debilitating symptoms. Research has shown that acupuncture can reduce pro-inflammatory cytokines and promote the release of anti-inflammatory substances (Carey, n.d.).
Studies have shown that acupuncture primarily modulates the polarization of M1/M2 macrophages by altering cytokine production and recruitment to inflammatory injury sites, thereby enhancing anti-inflammatory effects to reduce inflammatory pain and promote tissue repair (Frontiers in Immunology, 2023; PMC, 2021).
This dual effect of reducing inflammation while enhancing pain relief makes acupuncture an appealing option in a comprehensive management plan (Carey, n.d.). Animal studies show that acupuncture reduced inflammation and pain in affected joints and changed the levels of inflammatory cytokines (Global Autoimmune Institute, 2025). Another study showed that acupuncture had anti-inflammatory and pain-reducing effects, possibly by preventing macrophages from turning into pro-inflammatory cells in inflamed joints (Global Autoimmune Institute, 2025).
Mental and Emotional Well-Being
Acupuncture can significantly impact mental well-being, which is often compromised in those with autoimmune conditions (Carey, n.d.). The stress and anxiety associated with managing chronic illness can exacerbate symptoms and create a cycle of discomfort. Acupuncture has been shown to stimulate the release of endorphins and other neurotransmitters, promoting relaxation and reducing stress (Carey, n.d.).
By addressing both physical and emotional aspects of illness, acupuncture fosters a sense of harmony, making it easier for individuals to cope with their conditions and maintain a positive mindset (Carey, n.d.). Regular acupuncture sessions not only help with physical symptoms but also contribute to a more positive outlook, essential when navigating the challenges of autoimmune disorders.
Improving Circulation and Overall Function
One of the main ways acupuncture helps with autoimmune diseases is by increasing circulation throughout the body (Dr. Guan PTAP, 2023). By stimulating acupuncture points, the treatment increases blood and oxygen flow, which helps regulate the immune system and relieves inflammation associated with autoimmune disorders (Dr. Guan PTAP, 2023).
Studies have found that patients with rheumatoid arthritis experienced reduced pain and improved mobility with regular acupuncture treatments (Dr. Guan PTAP, 2023). Another study observed that patients with multiple sclerosis who received acupuncture experienced improvements in cognitive functioning and speech (Dr. Guan PTAP, 2023).
Eating Right to Feel Better- Video
Integration with Other Therapies
Integrating acupuncture with other lifestyle practices such as nutrition, sleep, and supplements can create a synergistic effect in managing autoimmune conditions (Carey, n.d.). Nutrition plays a critical role in supporting the immune system, while adequate sleep is essential for recovery and overall health. Mindset cultivation also proves pivotal; a positive outlook and resilience can enhance the effectiveness of all healing modalities (Carey, n.d.).
By embracing acupuncture as part of a multifaceted approach, individuals can empower themselves to take control of their health and improve their quality of life while managing autoimmune conditions (Carey, n.d.).
Massage Therapy: Healing Through Touch
Massage therapy offers another powerful tool in the comprehensive management of autoimmune conditions. By addressing muscle tension, improving circulation, and promoting relaxation, therapeutic massage provides both physical and emotional benefits for those living with chronic inflammatory conditions.
How Massage Helps Chronic Pain and Inflammation
Chronic pain often stems from muscle tension, nerve compression, or inflammation, and massage therapy directly targets these underlying causes (Renton Chiropractic Care, 2025). When muscles are tight and overworked from autoimmune-related inflammation, they can lead to discomfort, restricted movement, and pain. Massage therapy works by gently stretching and loosening muscles, relieving tightness and improving flexibility (Physician Partners of America, n.d.; Renton Chiropractic Care, 2025).
Increased blood flow is crucial for the healing process, as it delivers oxygen and nutrients to damaged tissues and helps flush out metabolic waste products such as lactic acid (Renton Chiropractic Care, 2025). Massage therapy stimulates circulation, ensuring that blood and lymph fluid can flow more freely through the body. This enhanced circulation not only promotes healing but also helps reduce swelling and inflammation in affected areas (Renton Chiropractic Care, 2025; Mayo Clinic Health System, 2022).
Breaking the Pain-Inflammation Cycle
Chronic pain and muscle tension can lead to painful bundles of tissue and the buildup of inflammatory toxins (Physician Partners of America, n.d.). If left untreated, these issues can worsen pain and reduce flexibility and mobility in the area. Regular massage therapy can break up these trigger points and promote nutrient-rich blood flow to the area, helping break up toxins (Physician Partners of America, n.d.).
When muscles or tissues press on nearby nerves, they can cause pain, numbness, or tingling (Renton Chiropractic Care, 2025). Therapeutic massage can help reduce pressure on nerves, providing relief from these symptoms and promoting better nerve function, particularly beneficial for conditions like sciatica and nerve-related autoimmune complications (Renton Chiropractic Care, 2025).
Natural Pain Relief and Stress Reduction
Massage therapy encourages the release of endorphins, the body’s natural painkillers (Renton Chiropractic Care, 2025; Texas Health School, 2024). These “feel-good” hormones help block pain signals and provide a natural, drug-free way to alleviate discomfort. Regular massage therapy can help reduce the frequency and intensity of chronic pain by boosting the body’s natural pain management (Renton Chiropractic Care, 2025).
Chronic pain is often exacerbated by stress, anxiety, and emotional tension (Renton Chiropractic Care, 2025). Massage therapy has a profound effect on the nervous system, promoting relaxation and reducing stress levels. By calming the nervous system, massage therapy can help break the cycle of pain and tension, allowing the body to heal more efficiently (Renton Chiropractic Care, 2025).
In addition to physical benefits, massage therapy offers relief from mental stress and anxiety around pain (Physician Partners of America, n.d.). The emotional and mental health aspects of pain can be just as significant as physical symptoms. The relaxation response from massage can soothe the mind, helping people more effectively manage their pain (Physician Partners of America, n.d.).
Physical Benefits for Autoimmune Conditions
For most patients, massage therapy serves as an important part of specific medical treatment plans to help them return to daily activities (Mayo Clinic Health System, 2022). Physical benefits of massage include improved circulation, reduced muscle stiffness, reduced joint inflammation, better sleep quality, quicker recovery between activities, improved flexibility, reduced pain and soreness, and a strengthened immune response (Mayo Clinic Health System, 2022).
Research has shown specific benefits for autoimmune conditions. In a study conducted at the University of Miami, a 15-minute moderate-pressure massage daily led to reduced pain and anxiety and improved grip strength in 22 adults diagnosed with hand or wrist arthritis (Arthritis Foundation, 2021). The participants received four weekly massages from a therapist and were taught to massage their sore joints daily at home. Results showed that massage combinations could reduce hand pain by up to 57% (Arthritis Foundation, 2021).
A study found that people receiving 10 weekly sessions of either relaxation massage or structural massage had less pain and were better able to perform daily activities than those receiving usual care (Arthritis Foundation, 2021). A separate 2014 study found that deep tissue massage alone relieved back pain equally as well as the combination of massage and nonsteroidal anti-inflammatory drugs (Arthritis Foundation, 2021).
Types of Therapeutic Massage
- Swedish Massage: This gentle and relaxing technique uses long, smooth strokes, kneading, and circular movements to improve circulation and relieve muscle tension (Renton Chiropractic Care, 2025). It’s ideal for people with mild to moderate chronic pain and is often used to promote relaxation and stress relief.
- Deep Tissue Massage: This technique targets the deeper layers of muscle and connective tissue, making it an excellent choice for individuals dealing with chronic tension, muscle stiffness, or injuries (Renton Chiropractic Care, 2025). By applying firm pressure and slower strokes, this technique helps break up scar tissue, reduce muscle knots, and relieve pain associated with chronic conditions like fibromyalgia and chronic back pain.
- Trigger Point Therapy: This approach focuses on specific areas of muscle tension, known as “trigger points” or “muscle knots” (Renton Chiropractic Care, 2025). These points can refer pain to other areas of the body, leading to discomfort in seemingly unrelated regions. By applying direct pressure to these trigger points, massage therapists can release tension and alleviate pain, often providing significant relief.
Integration into Holistic Care
For many people, therapeutic massage represents an effective part of a holistic interventional pain management program (Physician Partners of America, n.d.). Treatments can also include physical therapy, lifestyle changes such as posture improvement and nutritional counseling, therapeutic injections when necessary, and other integrative approaches.
By incorporating massage therapy into a comprehensive autoimmune management plan alongside chiropractic care, acupuncture, targeted exercise, proper nutrition, and stress management, individuals can experience synergistic benefits that address both physical symptoms and overall well-being.
Targeted Exercise and Rehabilitation: Building Strength and Resilience
Exercise and rehabilitation programs specifically designed for autoimmune conditions offer powerful tools for managing symptoms, preventing complications, and improving quality of life. When properly tailored to individual needs and limitations, targeted exercise can reduce inflammation, strengthen vulnerable areas, and enhance overall function.
The Foundation of Injury Prevention
Injury prevention hinges on proactively identifying and addressing deficits in strength, mobility, balance, and movement control (South Island Physio, 2025). Strength training, in particular, is among the most evidence-based strategies to reduce injury risk across all age groups and activity levels. Studies show that strengthening exercises can reduce sports-related injuries by up to 50% (South Island Physio, 2025; Ozark PT Specialists, 2024).
For individuals with autoimmune conditions who may already experience joint instability, muscle weakness, and increased inflammation, preventing additional injuries becomes crucial. A well-rounded exercise program should include specific exercises targeting common weak points such as hips, core, and rotator cuff; balance exercises to enhance neuromuscular control; stretching exercises and dynamic stretches to improve flexibility and range of motion; and gradually increasing training loads to build resilience and avoid overuse (South Island Physio, 2025).
Benefits of Targeted Exercise for Autoimmune Conditions
- Strengthening Vulnerable Areas: Targeted exercises reduce the risk of common injuries such as sprains, strains, and tears by strengthening muscles, stabilizing joints, and improving biomechanics (Ozark PT Specialists, 2024). For those with autoimmune conditions affecting joints and connective tissue, this strengthening provides crucial support and protection.
- Promoting Recovery: Exercise aids recovery by increasing blood flow, reducing inflammation, and promoting tissue repair (Ozark PT Specialists, 2024). This helps individuals bounce back quicker from disease flares or intense activity sessions. As the body transitions from the inflammatory to the repair phase, targeted exercises become critical for restoring a full range of motion, rebuilding strength in and around affected areas, preventing stiffness and muscle weakness, and improving joint stability and mobility (South Island Physio, 2025).
- Enhancing Mental Focus: Targeted exercises promote mental focus and concentration, helping individuals stay present and engaged (Ozark PT Specialists, 2024). For those dealing with brain fog and cognitive difficulties common in autoimmune conditions, this mental benefit proves particularly valuable.
- Reducing Inflammation: Regular physical activity has been shown to reduce systemic inflammation when performed at appropriate intensity and duration (Ozark PT Specialists, 2024). This anti-inflammatory effect complements other interventions and helps manage autoimmune symptoms.
Essential Exercise Components
- Dynamic Warm-Up: Beginning workouts with dynamic movements such as leg swings, arm circles, and hip rotations increases blood flow, warms up muscles, and improves joint mobility (Ozark PT Specialists, 2024). This preparation reduces injury risk and enhances exercise effectiveness.
- Strength Training: Incorporating exercises that target major muscle groups—including squats, lunges, deadlifts, push-ups, and rows—builds strength, stability, and muscular endurance (Ozark PT Specialists, 2024). For patients with autoimmune conditions, modifications may be necessary based on joint involvement and current symptom levels.
- Flexibility Exercises: Performing stretches for key muscle groups involved in daily activities, focusing on areas prone to tightness and imbalances such as hamstrings, quadriceps, hip flexors, calves, shoulders, and chest, maintains and improves range of motion (Ozark PT Specialists, 2024). Gentle stretching proves particularly beneficial for those with rheumatoid arthritis and other joint-affecting conditions.
- Core Stability: Strengthening core muscles with exercises like planks, bridges, Russian twists, and bicycle crunches improves posture, balance, and overall stability, reducing the risk of lower back and hip injuries (Ozark PT Specialists, 2024). Core stability training is effective in reducing injury rates (PMC, 2012).
Personalized Exercise Programs
Therapists implement targeted exercises that strengthen muscles and improve joint stability, effectively preventing common ailments and minimizing the likelihood of disease-related setbacks (Simply PT, 2025). By conducting comprehensive assessments, physical therapists identify potential vulnerabilities and provide personalized recommendations to address specific needs (Simply PT, 2025).
Customized exercise plans often include strengthening and flexibility routines that target key areas, enhancing overall performance and reducing injury risk (Simply PT, 2025). This personalized approach ensures each individual receives the specific interventions necessary to maintain optimal health and function.
Rehabilitation Strategies
- Engaging in Customized Routines: Exercise routines help strengthen specific muscles and improve joint flexibility (Harter Physical Therapy, 2024). These exercises focus on strengthening weakened areas and gradually restoring strength and function.
- Joint Mobilizations: Therapists use precise movements to improve joint mobility, reduce stiffness, and alleviate pain (Harter Physical Therapy, 2024). This approach proves particularly valuable for autoimmune conditions involving joint inflammation.
- Corrective Exercises: These exercises address muscle imbalances and faulty movement patterns, reducing the risk of injuries (Simply PT, 2025). By targeting specific weaknesses, they ensure individuals perform activities safely and efficiently.
- Functional Training: This enhances the ability to execute daily movements, aiding in effective pain management without excessive reliance on medication (Simply PT, 2025). Tailored programs empower individuals to maintain function and recover swiftly from exertion.
Integration with Professional Guidance
Assessment of movement patterns is vital in reducing injury risk, as it identifies issues and weaknesses (Simply PT, 2025). Physical therapists develop customized exercise regimens targeting specific needs to enhance coordination between the brain and muscles. Routine follow-ups and adjustments ensure ongoing effectiveness and adapt to progress, fostering sustained improvement (Simply PT, 2025).
Neglecting exercise therapy during rehabilitation can lead to persistent deficits and a higher chance of symptom recurrence (South Island Physio, 2025). By incorporating targeted exercise into comprehensive autoimmune management plans alongside chiropractic care, acupuncture, massage therapy, proper nutrition, and stress management, individuals can achieve optimal outcomes and long-term health.
Nutrition and Dietary Approaches for Autoimmune Wellness
Nutrition plays a pivotal role in managing autoimmune conditions by supporting immune function, reducing inflammation, and promoting overall health. The foods we consume can either fuel inflammation or help calm the immune response, making dietary choices a powerful tool in managing autoimmune conditions.
The Anti-Inflammatory Diet Foundation
Anti-inflammatory diets have garnered attention as a lifestyle approach to modulating unregulated immune responses (PMC, 2024). They are characterized by high consumption of fruits, vegetables, whole grains, legumes, fatty fish, nuts, olive oil, and phytochemicals, while limiting intake of foods with potentially pro-inflammatory properties such as red meat, refined carbohydrates, and alcohol (PMC, 2024).
The rationale for anti-inflammatory diets lies in their capacity to decrease levels of pro-inflammatory biomarkers and positively influence pathways involved in the inflammatory cascade (PMC, 2024). Foods rich in omega-3 fatty acids, antioxidants, and polyphenols have been shown to reduce the expression of pro-inflammatory genes and decrease circulating levels of inflammatory biomarkers (PMC, 2024).
Anti-inflammatory food plans include the Mediterranean diet, vegetarian and vegan diets, ketogenic diets, and foods rich in omega-3 fatty acids and fiber (Global Autoimmune Institute, 2025). Popular anti-inflammatory dietary patterns include the Mediterranean diet, DASH diet, and vegetarian diets (Harvard Nutrition Source, 2025).
Key Anti-Inflammatory Foods
- Omega-3 Fatty Acids: Present in fatty fish like salmon, mackerel, sardines, as well as flaxseeds and walnuts, these fats help reduce inflammation (Dr. Farheen, n.d.; Harvard Nutrition Source, 2025). Studies show that consuming foods rich in omega-3 PUFAs is associated with lower levels of pro-inflammatory biomarkers (PMC, 2024).
- Fruits and Vegetables: Rich in antioxidants and phytonutrients, colorful fruits and vegetables help combat oxidative stress and inflammation (Carey, n.d.; Dr. Farheen, n.d.). Berries, leafy greens like spinach, kale, and Swiss chard, and colorful vegetables are particularly beneficial due to their high levels of vitamins A, C, and K, as well as magnesium and iron (Carey, n.d.).
- Whole Grains: Foods like brown rice, quinoa, and whole oats provide essential nutrients and fiber, promoting digestive health and reducing inflammation (Dr. Farheen, n.d.; Global Autoimmune Institute, 2025).
- Nuts and Seeds: Almonds, chia seeds, walnuts, and sunflower seeds offer healthy fats and antioxidants that support joint health (Carey, n.d.; Dr. Farheen, n.d.).
- Healthy Fats: Olive oil and avocados are excellent sources of monounsaturated fats, which can help reduce inflammation (Carey, n.d.; Dr. Farheen, n.d.; Harvard Nutrition Source, 2025).
- Herbs and Spices: Turmeric and ginger contain natural anti-inflammatory compounds that can aid in pain relief and inflammation reduction (Dr. Farheen, n.d.; Harvard Nutrition Source, 2025). Components found in rosemary, basil, garlic, anise, red pepper, onions, and cloves exhibit efficacy against chronic diseases by inhibiting inflammatory pathways and reducing inflammatory cytokines (PMC, 2024).
- Fermented Foods: Including yogurt, kefir, sauerkraut, and kimchi, these foods support gut health by providing probiotics (Carey, n.d.). A healthy gut microbiome is increasingly recognized for its role in immune regulation, making these foods valuable for autoimmune management.
The Autoimmune Protocol (AIP) Diet
The Autoimmune Protocol diet is an elimination diet that aims to reduce inflammation and symptoms associated with autoimmune disorders (Healthline, 2020; Cleveland Clinic, 2023). The AIP diet eliminates all possible food-based triggers for inflammation and slowly reintroduces them until individual triggers are identified (Cleveland Clinic, 2023).
Research shows promising results for the AIP diet. In an 11-week study of 15 people with inflammatory bowel disease on an AIP diet, participants reported significantly fewer IBD-related symptoms by the end of the survey (Healthline, 2020). Another study had 16 women with Hashimoto’s thyroiditis follow the AIP diet for 10 weeks. By the end, inflammation and disease-related symptoms decreased by 29% and 68%, respectively (Healthline, 2020).
Foods to Avoid
- Processed Foods: These often contain additives, preservatives, and artificial ingredients that can disrupt gut health and trigger inflammation (Carey, n.d.). Common examples include packaged snacks, sugary cereals, and frozen meals. High levels of refined sugars and unhealthy fats in processed foods can lead to insulin resistance and increased inflammation (Carey, n.d.).
- Gluten: A protein found in wheat, barley, and rye, gluten can provoke immune responses in individuals with celiac disease or non-celiac gluten sensitivity (Carey, n.d.). Even in those without diagnosed sensitivities, gluten can contribute to gut permeability and inflammation, making it beneficial to eliminate gluten-containing foods and explore gluten-free alternatives (Carey, n.d.).
- Dairy Products: While dairy can be a good source of calcium and vitamin D, it can trigger inflammation and digestive issues in some individuals (Carey, n.d.). Many report experiencing symptoms such as bloating, gas, or fatigue after consuming dairy. Plant-based alternatives such as almond or coconut milk can serve as substitutes while still providing essential nutrients (Carey, n.d.).
- High-Sugar Foods and Beverages: Excessive sugar intake can increase inflammation and raise the risk of chronic diseases (Carey, n.d.). Sugary drinks, desserts, and snacks can spike blood sugar levels, leading to energy crashes and mood swings. Focusing on natural sources of sweetness, such as fruits, and incorporating healthy fats and proteins can provide more stable energy (Carey, n.d.).
The Gut-Immune Connection
The gut microbiome plays a crucial role in immune system regulation, with research highlighting strong links between autoimmune diseases and gut microbiota (Oxford Academic, 2024). Analysis revealed that autoimmune disease had the strongest association with variations in gut microbiota compared to other diseases (Oxford Academic, 2024).
Gut dysbiosis, characterized by altered diversity and function, is consistently associated with autoimmune conditions such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes (Frontiers in Microbiomes, 2025). The microbiota exerts a protective influence on autoimmunity by promoting immune regulation, although it can also trigger pro-inflammatory immune responses when disrupted (Frontiers in Microbiomes, 2025).
A disruption to the gut microbiome or an impaired mucosal barrier can allow antigens to enter and interact with the mucosal immune system in a pro-inflammatory manner (Frontiers in Microbiomes, 2025). Over time, this dysfunction can trigger a systemic immune response, driving pathogenic immune cells and the development of autoimmune disease.
Restoring gut health through the use of probiotics, prebiotics, and dietary changes can significantly improve immune function and reduce autoimmune symptoms (Flourish Counseling, MD, 2025). By prioritizing gut health through appropriate nutrition, individuals can create a foundation for better immune regulation and reduced inflammation.
Sleep: The Underestimated Pillar of Autoimmune Health
Sleep represents a fundamental aspect of overall health, particularly for those managing autoimmune conditions. Quality sleep enables vital restorative processes, including tissue repair, muscle growth, and hormone regulation (Carey, n.d.). Disrupted sleep can exacerbate symptoms of autoimmune diseases, leading to increased fatigue, pain, and inflammation.
The Sleep-Immune Connection
Sleep exerts an immune-supportive function, promoting host defense against infection and inflammatory insults (Nature, 2021). Sleep deprivation has been associated with alterations of innate and adaptive immune parameters, leading to a chronic inflammatory state and increased risk for infectious and inflammatory pathologies, including cardiometabolic, neoplastic, autoimmune, and neurodegenerative diseases (Nature, 2021).
Research has shown a strong connection between sleep disturbances and the exacerbation of autoimmune symptoms (Carey, n.d.). Conditions such as rheumatoid arthritis, lupus, and multiple sclerosis often see a worsening of symptoms with poor sleep quality. Sleep deprivation can lead to hormonal imbalances, increased stress levels, and a weakened immune response, all of which can further complicate autoimmune disease management (Carey, n.d.).
Sleep’s Impact on Immune Function
The sleep cycle consists of several stages, including light sleep, deep sleep, and REM sleep (Carey, n.d.). Each stage plays a crucial role in physical and mental health. Deep sleep is particularly important for physical recovery and immune function, while REM sleep supports cognitive processes like memory consolidation and emotional regulation (Carey, n.d.).
Quality sleep helps regulate the immune response, promoting the production of cytokines—proteins involved in inflammation and immune responses (Carey, n.d.). Insufficient sleep can lead to an imbalance, causing the immune system to become overactive or underactive. For those with autoimmune conditions, this can mean heightened symptoms and flare-ups (Carey, n.d.).
Seven days after experimental sleep deprivation, levels of IL-17A and TNF-α remained elevated (PMC, 2022). These results suggest that some inflammatory effects of sleep deprivation may be long-lasting and possibly not easily reversible, thus impacting the risk of autoimmune diseases (PMC, 2022). A meta-analysis of more than 50,000 patients found a significant increase in CRP and IL-6 levels in subjects with sleep disturbances (PMC, 2022).
Sleep Deficiency and Autoimmune Risk
Studies demonstrate that disturbed sleep may be a trigger or risk factor for autoimmune diseases (PMC, 2015). Regulatory T cells (Treg) are key players in suppressing inappropriate immune responses and maintaining self-tolerance (PMC, 2015). Breakdown of self-tolerance is central to the pathogenesis of most autoimmune diseases. In experimentally sleep-deprived healthy persons, the suppressive activity of Treg is reduced, providing a link between sleep disorders and autoimmune diseases (PMC, 2015).
Non-apnea sleep disorders can increase the risk of developing autoimmune diseases such as rheumatoid arthritis, ankylosing spondylitis, systemic lupus erythematosus, and systemic sclerosis by disrupting immunologic self-tolerance and increasing the production of several pro-inflammatory cytokines (Nufactor, 2023). Even temporary sleep deprivation may lead to suppression of Treg cells and excessive immune response (Nufactor, 2023).
It is theorized that sleep deprivation may directly increase susceptibility to immune system diseases by elevating circulating leukocyte levels, increasing circulating pro-inflammatory markers, and reducing natural killer cell activity (Nufactor, 2023). Gene expression changes related to immune and inflammatory processes and oxidative stress were also specifically observed in those with deprived sleep (Nufactor, 2023).
Strategies for Improving Sleep Quality
- Establish Consistent Sleep Schedule: Going to bed and waking up at the same time each day helps regulate the body’s internal clock (Carey, n.d.). This consistency makes it easier to fall asleep and wake up refreshed, particularly beneficial for those experiencing fatigue as a symptom of autoimmune conditions.
- Create Optimal Sleep Environment: A comfortable, dark, and quiet bedroom facilitates better sleep (Carey, n.d.). Consider investing in blackout curtains to block light, using earplugs or a white noise machine to minimize noise disruptions, and keeping the room cool. Ensure the mattress and pillows provide adequate support and comfort (Carey, n.d.).
- Develop Bedtime Routine: Creating a calming bedtime routine signals the body that it’s time to wind down (Carey, n.d.). This might include relaxing activities such as reading, gentle stretching, or meditation. Limiting screen time before bed is essential, as blue light from devices can interfere with melatonin production.
- Practice Relaxation Techniques: Mindfulness, meditation, or deep-breathing exercises can help calm the mind and prepare it for sleep (Carey, n.d.). Journaling before bed can also be beneficial, allowing expression of thoughts and feelings, which may reduce anxiety and promote peace.
- Address Nutrition: Certain foods can promote sleep, such as those rich in magnesium, tryptophan, and melatonin (Carey, n.d.). Incorporating a balanced diet that emphasizes whole foods, healthy fats, and lean proteins can support better sleep and overall health. Limiting caffeine and sugar intake, especially in the hours before bedtime, can help prevent sleep disturbances (Carey, n.d.).
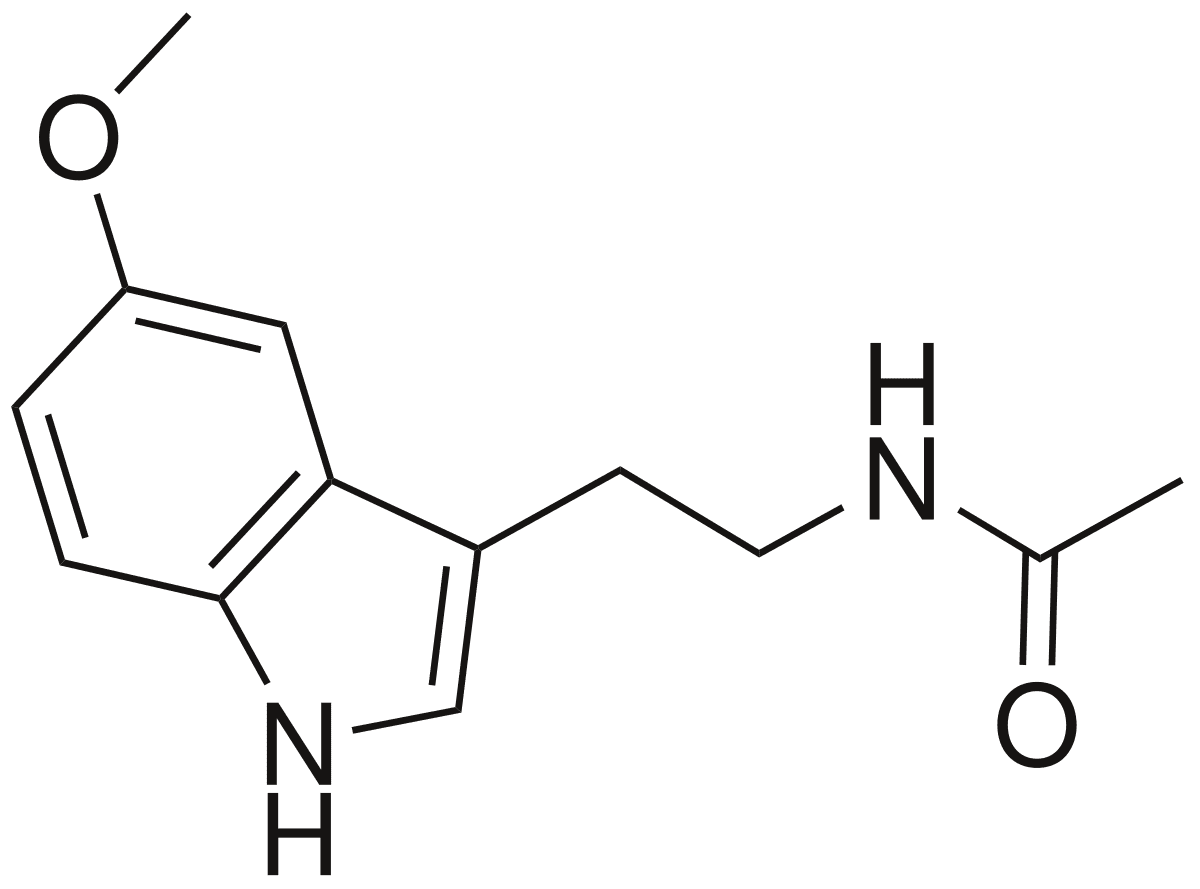
- Consider Sleep Supplements: Melatonin, an essential hormone for regulating sleep-wake cycles, can be particularly beneficial for those struggling with insomnia (Carey, n.d.). Magnesium supplements can also promote relaxation and improve sleep quality. Before starting any new supplements, consult a healthcare provider to ensure safety and effectiveness, especially when used in conjunction with existing treatment plans (Carey, n.d.).
Poor sleep can increase inflammation and weaken the immune system (Flourish Counseling, MD, 2025). Prioritizing quality sleep is essential for managing autoimmune conditions. By implementing these strategies and recognizing sleep as a crucial component of health, individuals can significantly improve their outcomes in managing autoimmune conditions.
Stress Management and Mindset: The Mind-Body Connection
The mind-body connection represents a profound concept that recognizes the intricate relationship between mental, emotional, and physical health (Carey, n.d.). For those managing autoimmune conditions, understanding this connection proves particularly empowering, as stress, anxiety, and emotional turmoil can exacerbate physical symptoms and lead to flare-ups.
Understanding Stress’s Impact on Autoimmune Health
Chronic stress can worsen autoimmune conditions by increasing inflammation and disrupting immune function (Flourish Counseling MD, 2025; MGI Clinic, 2025). Stress management techniques like mindfulness meditation, yoga, and biofeedback help reduce stress and its impact on the body (Flourish Counseling MD, 2025).
Stress is a common trigger for autoimmune flare-ups (Tolpa Holistic Health, 2025). Elevated cortisol over long periods creates imbalances that worsen symptoms. Holistic care emphasizes practices that calm the nervous system and restore balance, including yoga or tai chi for gentle movements that reduce tension; meditation and breathwork as tools that lower cortisol and improve focus; and journaling or nature walks as outlets for emotional release and clarity (Tolpa Holistic Health, 2025).
These practices improve more than symptoms—they strengthen resilience, enhance mood, and support better sleep (Tolpa Holistic Health, 2025). Stress management is considered a cornerstone of long-term autoimmune wellness.
The Power of Meditation for Autoimmune Healing
Meditation offers transformative healing for autoimmune disease, with science-backed symptom relief (PowersBeing, 2025). Research shows that meditation was among the most critical components in achieving remission in autoimmune diseases such as lupus and Hashimoto’s (PowersBeing, 2025).
Physically, meditation has been shown to strengthen immune function, reduce chronic pain, improve sleep, lower risk of cardiovascular disease, lower resting heart rate, and lower blood pressure (PowersBeing, 2025). Research continues to suggest meditation helps in the management of a series of conditions, including autoimmune diseases.
Meditation helps improve cognitive function, enhance stress management, lower anxiety, increase mindfulness, foster self-awareness, reduce negative emotions, increase feelings of patience, tolerance, and compassion, and improve focus (PowersBeing, 2025). With brain fog experienced with autoimmune diseases, cognitive health, and focus are compelling reasons to develop a meditation practice.
A specific type of Heart Coherence Meditation has helped individuals heal from the effects of chronic inflammation associated with autoimmune conditions (Dr. Daniel Lewis, 2021). This meditation allows the heart and brain to synchronize, creating a coherent rhythm between the organs that establishes a new baseline and leads to sustained improvements in health over time (Dr. Daniel Lewis, 2021).
Cultivating a Positive Mindset
Building a positive mindset is essential for navigating the challenges of autoimmune conditions (Carey, n.d.). A positive outlook can significantly influence not only emotional well-being but also physical health. Research shows that a positive mindset can lead to improved immune function, reduced stress levels, and greater ability to cope with symptoms of chronic illness (Carey, n.d.).
- Mindfulness and Meditation Practices: These techniques encourage individuals to focus on the present moment, thereby reducing anxiety and negative thought patterns (Carey, n.d.). Simple mindfulness exercises such as deep-breathing techniques or guided meditations can be incorporated into daily routines. By dedicating just a few minutes each day to these practices, individuals can begin to rewire their brains, promoting a sense of calm and resilience (Carey, n.d.).
- Supportive Community: Surrounding oneself with a supportive community can play a vital role in building a positive mindset (Carey, n.d.). Engaging with others who understand the struggles of autoimmune conditions can provide a sense of belonging and validation. Support groups, both in-person and online, offer safe spaces for sharing experiences, learning from one another, and celebrating progress (Carey, n.d.).
- Gratitude Practice: Cultivating gratitude can serve as a powerful tool for building a positive mindset (Carey, n.d.). Regularly reflecting on and acknowledging things one is thankful for can shift focus from challenges to positive aspects of life. Keeping a gratitude journal, in which individuals jot down daily reflections, can reinforce this practice and offer an opportunity to celebrate small victories (Carey, n.d.).
Mind-Body Techniques for Stress Reduction
Stress management techniques are crucial for those managing autoimmune conditions (Carey, n.d.). Various approaches can be employed to create a more balanced and harmonious life:
- Mindfulness Meditation: This practice encourages individuals to focus on the present moment, reducing anxiety and promoting calm (Carey, n.d.). Regular mindfulness sessions, whether through guided apps or local classes, can empower individuals to regain control over their mental well-being.
- Cognitive Behavioral Strategies: These techniques help shift negative thought patterns and focus on gratitude and acceptance (Carey, n.d.). By reframing negative thoughts, individuals can move their experience of living with an autoimmune condition, thereby increasing motivation to engage in healthy behaviors.
- Biofeedback: This technique helps individuals learn to control physiological functions by receiving real-time feedback about body processes (Flourish Counseling, MD, 2025). It can be particularly helpful for managing stress responses.
- Creative Expression: Engaging in creative activities—whether through art, music, or writing—provides an outlet for stress relief (MGI Clinic, 2025). Creative expression has been shown to lower stress and provide emotional release, which can improve immune system regulation.
Addressing Unmet Needs
Ignoring unmet needs and allowing stress to persist can severely hinder the body’s ability to heal (MGI Clinic, 2025). Unmet needs commonly linked to autoimmune inflammation include time in nature, rest and sleep, intimacy, physical activity, creative expression, and access to healthy food (MGI Clinic, 2025).
In many cases, individuals dealing with autoimmune inflammation have multiple unmet needs that go unnoticed or unaddressed (MGI Clinic, 2025). When individuals fail to prioritize these needs due to work, family, or social obligations, the immune system continues to struggle, unable to return to a state of balance.
By taking a holistic approach that addresses the root causes of stress and unmet needs, individuals can start to manage inflammation more effectively (MGI Clinic, 2025). Autoimmune inflammation management is about more than treating symptoms; it’s about nurturing overall well-being through intentional changes that help reduce inflammation, improve immune function, and restore balance to the body.
Nutritional Supplements for Autoimmune Support
Supplementation can play a vital role in managing autoimmune conditions by addressing nutrient deficiencies, reducing inflammation, and supporting immune balance (Performance Health and Wellness, 2025). When combined with lifestyle changes and integrative care, targeted supplements can enhance healing and resilience.
Vitamin D: The Immune Regulator
Vitamin D is crucial for immune regulation, with research indicating a significant correlation between low vitamin D levels and the severity of various autoimmune diseases (Carey, n.d.). This vitamin plays a critical role in immune regulation and may help mitigate the risk of flare-ups. Women should consider getting their vitamin D levels tested and consult with a healthcare provider about appropriate supplementation, particularly during winter months or in regions with limited sunlight (Carey, n.d.).
Vitamin D supplementation for five years, with or without omega-3 fatty acids, reduced autoimmune disease by 22% (BMJ, 2022; Cooper Complete, 2024). In a large study of more than 25,000 older adults, vitamin D supplementation at 2000 IU/day for approximately 5 years was associated with a lower incidence of confirmed autoimmune disease than placebo (BMJ, 2022).
When only the last three years of the intervention were considered, the vitamin D group had 39% fewer participants with confirmed autoimmune disease than the placebo group (BMJ, 2022). Vitamin D regulates a wide array of genes involved in inflammation and immunity and has been inconsistently associated with reduced risk of several autoimmune diseases in previous observational studies (BMJ, 2022).
Omega-3 Fatty Acids: Natural Anti-Inflammatories
Omega-3 fatty acids are among the most researched supplements for autoimmune support (Carey, n.d.). Found in fish oil or algae-based sources, these fatty acids possess anti-inflammatory properties that can help alleviate symptoms of conditions such as rheumatoid arthritis and lupus. Regular intake of omega-3s may reduce joint pain and stiffness and support heart health, which is often a concern for those with autoimmune diseases (Carey, n.d.).
Omega-3 fatty acid supplementation, with or without vitamin D, reduced the rate of autoimmune disease by 15% (BMJ, 2022). Several past trials have proven the beneficial effects of omega-3 fatty acid supplementation on systemic inflammation and tender and swollen joints (PMC, 2024). Dietary marine-derived long-chain omega-3 fatty acids decrease systemic inflammation and ameliorate symptoms in some autoimmune diseases (BMJ, 2022).
A study of more than 20,000 participants showed that, two years after a randomized five-year trial, the benefits of vitamin D in preventing autoimmune diseases had waned. At the same time, those of omega-3 remained strong (Medical News Today, 2024). There were 234 confirmed autoimmune disease cases among people who received omega-3 supplements compared with 280 among those who received a placebo—a statistically significant hazard ratio of 0.83 (Medical News Today, 2024; Rheumatology Advisor, 2024).
In the two-year follow-up period after the initial trial, the protective effect of vitamin D alone diminished compared with placebo arms, whereas the effect of omega-3 fatty acids was sustained (Rheumatology Advisor, 2024; Lupus News, 2022).
Probiotics: Supporting Gut Health
Probiotics hold immense potential for managing autoimmune conditions (Carey, n.d.). These beneficial bacteria can enhance gut health, a cornerstone of immune function, increasingly recognized as such. A balanced gut microbiome can influence levels of inflammation and the overall immune response.
Choosing a high-quality probiotic supplement can promote digestive health and may help reduce the frequency and severity of autoimmune flare-ups (Carey, n.d.). Fermented foods such as yogurt and kimchi can further support this effort by providing a diverse array of beneficial bacteria.
Antioxidants: Combating Oxidative Stress
Antioxidants like vitamins C and E, as well as selenium, can provide essential support for those facing autoimmune challenges (Carey, n.d.). These nutrients help combat oxidative stress, which is often elevated in individuals with autoimmune diseases. Incorporating a range of colorful fruits and vegetables into the diet can significantly boost antioxidant intake.
Additionally, considering a comprehensive multivitamin may ensure adequate levels of these vital nutrients, contributing to a more balanced and resilient immune system (Carey, n.d.).
Targeted Supplementation
The role of supplements in managing autoimmune diseases extends beyond basic nutrition (Flourish Counseling, MD, 2025). In addition to traditional medical treatments, integrative therapies combined with targeted supplementation can significantly enhance outcomes.
It’s important to consult healthcare professionals, such as registered dietitians or naturopathic doctors specializing in autoimmune conditions, for personalized recommendations (Carey, n.d.). They can provide guidance based on unique health needs and dietary requirements. This step is particularly important because certain supplements can interact with medications or exacerbate specific symptoms (Carey, n.d.).
When choosing supplements, research the brand and its reputation (Carey, n.d.). Look for companies that prioritize transparency about sourcing, manufacturing processes, and ingredient quality. Check for third-party testing and certifications from reputable organizations to ensure supplements are free from contaminants and accurately labeled.
Creating Your Personalized Autoimmune Wellness Plan
Managing autoimmune conditions requires a comprehensive approach that addresses not just symptoms but underlying causes. By integrating the various modalities discussed—chiropractic care, acupuncture, massage therapy, targeted exercise, nutrition, sleep optimization, stress management, and appropriate supplementation—individuals can create personalized plans that support healing and enhance quality of life.
The Integrative Approach
Integrating acupuncture, nutrition, sleep, mindset, and supplements creates a holistic approach to managing autoimmune conditions (Carey, n.d.). Each of these elements plays a crucial role in overall health and well-being, influencing the body’s ability to heal and maintain balance. When these practices are combined, they can enhance each other’s effects, leading to improved symptom management and better quality of life (Carey, n.d.).
By adopting a holistic approach that integrates multiple modalities, individuals can take charge of their health and navigate the complexities of autoimmune conditions more effectively (Carey, n.d.). This comprehensive strategy addresses the whole person—physical, emotional, and mental—rather than isolated symptoms.
Assessing Your Unique Needs
Assessing unique needs is a critical first step in managing autoimmune conditions effectively (Carey, n.d.). Every person’s experience with autoimmune disorders is distinct, shaped by individual symptoms, lifestyle choices, and personal circumstances. Understanding these unique factors allows for tailoring a management plan that resonates with the body and mind.
Begin by keeping a detailed journal of symptoms, dietary habits, sleep patterns, and emotional responses (Carey, n.d.). This practice helps recognize triggers and guides more effective communication with healthcare providers. Different individuals may react differently to various interventions, making it essential to identify which approaches provide relief and which exacerbate symptoms.
Working with Healthcare Professionals
Consulting with healthcare professionals is crucial in managing autoimmune conditions (Carey, n.d.). Expert guidance can provide clarity on symptoms, treatment options, and lifestyle adjustments that significantly impact overall well-being. When seeking assistance, engage a range of professionals, including primary care physicians, specialists, nutritionists, and alternative medicine practitioners, to create a comprehensive, personalized management plan.
Open communication is essential; sharing experiences and any changes in condition helps physicians tailor their approach to individual needs (Carey, n.d.). Incorporating nutrition guidance from registered dietitians or nutritionists who specialize in autoimmune conditions offers valuable insights into dietary choices that may reduce inflammation and support immune function.
Alternative therapies such as acupuncture can be beneficial when coordinated with the healthcare team (Carey, n.d.). Discussing these options ensures a coordinated approach that considers all aspects of health. Maintaining consistent dialogue with healthcare professionals about mental health and mindset is also essential, as chronic health conditions can lead to feelings of anxiety or depression that may exacerbate physical symptoms (Carey, n.d.).
Tracking Progress and Adjustments
Tracking progress when managing autoimmune conditions is crucial for understanding what strategies are effective and what may need adjustment (Carey, n.d.). Keeping a journal documenting daily symptoms, diet, sleep patterns, and emotional states helps identify trends and triggers that impact health. This information provides valuable data for discussing with healthcare providers, enabling more personalized and effective treatment plans.
Incorporating various therapies into a wellness routine can lead to significant improvements, but progress may vary (Carey, n.d.). Noting changes in symptoms after interventions helps identify which approaches yield better results. If symptoms persist despite adjustments, it may be necessary to consult specialists to refine strategies.
Regularly assessing mental well-being through self-reflection or mindfulness practices helps track emotional fluctuations (Carey, n.d.). If negative emotions persist, consider engaging in therapy or support groups. Monitoring progress in these areas not only enhances resilience but also empowers individuals to take an active role in health management.
Celebrating Achievements
Celebrating achievements, no matter how small, is an essential part of managing autoimmune conditions (Carey, n.d.). Recognizing and celebrating progress can help shift mindset, reinforce positive behaviors, and motivate continued effort on the healing journey. Whether it’s a successful treatment session, improved habits, better sleep patterns, or a positive change in mindset, acknowledging these milestones can significantly enhance well-being.
Keeping a journal dedicated to the health journey can serve as a reflection of progress (Carey, n.d.). Writing down accomplishments allows tracking of growth over time and provides a tangible reminder of how far one has come. Sharing achievements with a support network—friends, family, or a community of others who understand the unique challenges—can foster connection and encouragement.
By cultivating self-compassion and recognizing that progress is not always linear, individuals can remain grounded and realistic about their journey (Carey, n.d.). Celebrating achievements includes recognizing the effort put into managing health, regardless of outcomes. By nurturing a supportive inner dialogue, individuals can propel themselves forward, celebrating victories today while looking forward to future possibilities.
Conclusion: Embracing a New Path to Wellness
Autoimmune diseases are very hard to deal with and affect millions of people, especially women. They affect almost every part of life. But research and clinical experience show that these conditions don’t have to define or limit the quality of life. Individuals can achieve substantial improvements in health and well-being through functional wellness methodologies that target underlying causes rather than merely alleviating symptoms. To fully manage autoimmune diseases, you need to understand how the immune system works, how inflammation affects disease processes, and how these diseases differ from one another. Integrative approaches that address the whole person—body, mind, and spirit—can help people regain balance and heal naturally.
Chiropractic care, as demonstrated by Dr. Alexander Jimenez’s integrative practice in El Paso, provides effective methods to enhance nervous system function, diminish inflammation, improve mobility, and promote overall health. When you add acupuncture’s immune-modulating effects to massage therapy’s ability to reduce pain and promote relaxation, targeted exercise programs that strengthen weak areas, anti-inflammatory nutrition that supports gut health, restorative sleep practices, stress management techniques, and the right supplements, you get a healing effect that works together. Practitioners like Dr. Jimenez, who has training in both chiropractic and functional medicine, have observed clinical correlations showing that addressing the causes of injuries and improving health through targeted, nonsurgical treatments can have remarkable effects. Practitioners can help reduce overlapping pain symptoms, improve function, and enhance quality of life by combining spinal adjustments, acupuncture, massage therapy, and rehabilitative exercises. This will also help fix the imbalances that are causing autoimmune dysfunction.
The functional wellness approach may be most important because it empowers people to take an active role in their own healing. People don’t have to feel helpless when they have a chronic illness. They can make smart choices about diet, exercise, stress management, and other lifestyle factors that significantly affect how autoimmune diseases progress. This feeling of control and agency, along with full professional support, makes for the best setting for healing and long-term health. As we learn more about autoimmune diseases and improve integrative treatment methods, the future looks bright for even better ways to manage them. People with autoimmune diseases can take comfort in knowing that there are many safe, effective, and natural ways to improve their health, ease their symptoms, and improve their quality of life.
The path to health may take time and require patience, but people can make significant strides with the right mix of professional help, lifestyle changes, and holistic therapies. People with autoimmune diseases can go beyond just surviving and really thrive by accepting functional wellness and working with knowledgeable professionals who understand how body systems are connected.
References
- A4M. (2016, December 31). Dr. Alex Jimenez, DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html
- Anchor to Health. (2023, March 2). Can chiropractic care help autoimmune conditions? How? https://anchortohealth.com/2023/03/03/can-chiropractic-care-help-autoimmune-conditions-how/
- Arthritis Foundation. (2021, January 27). Benefits of massage. https://www.arthritis.org/health-wellness/treatment/complementary-therapies/natural-therapies/benefits-of-massage
- Atlas Chiropractic. (2024, February 29). 6 benefits of chiropractic care for autoimmune conditions. https://atlastchiropractic.com/6-benefits-of-chiropractic-care-for-autoimmune-conditions/
- Better Health Victoria. (1999, October 11). Immune system explained. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/immune-system
- BMJ. (2022, January 25). Vitamin D and marine omega-3 fatty acid supplementation and autoimmune disease. https://www.bmj.com/content/376/bmj-2021-066452
- Carey, C. (n.d.). Healing harmony: A woman’s guide to managing auto-immune conditions.
- Chiro CT. (2025, January 14). The role of chiropractic care in managing autoimmune conditions. https://chiroct.com/the-role-of-chiropractic-care-in-managing-autoimmune-conditions/
- Cleveland Clinic. (2023, June 27). What is the AIP (autoimmune protocol) diet? https://health.clevelandclinic.org/aip-diet-autoimmune-protocol-diet
- Cooper Complete. (2024, July 16). Vitamin D and omega-3 supplementation and autoimmune diseases. https://coopercomplete.com/blog/supplements-for-autoimmune-disease/
- Dr. Alex Jimenez. (2025, August 16). El Paso, TX, doctor of chiropractic. https://dralexjimenez.com
- Dr. Daniel Lewis. (2021, July 31). Arthritis and the mind-body immune connection. https://www.daniellewis.com.au/health-information/inspiring-stories-of-recovery/arthritis-and-the-mind-body-immune-connection/
- Dr. Farheen. (n.d.). Embracing an anti-inflammatory diet for rheumatoid arthritis. https://www.drfarheen.com/blog/embracing-an-anti-inflammatory-diet-for-rheumatoid-arthritis
- Dr. Guan PTAP. (2023, August 10). How acupuncture can help manage autoimmune diseases. https://www.drguanptap.com/acupuncture-autoimmune-diseases/
- Flourish Counseling, MD. (2025, February 12). Holistic approaches to managing autoimmune diseases. https://flourishcounselingmd.com/managing-autoimmune-diseases/
- Frontiers in Immunology. (2023, April 5). The immunomodulatory mechanisms for acupuncture practice. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1147718/full
- Frontiers in Immunology. (2023, May 2). Emerging role of gut microbiota in autoimmune diseases. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1365554/full
- Frontiers in Immunology. (2023, October 3). The role of inflammation in autoimmune disease. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1267091/full
- Frontiers in Microbiomes. (2025, May 15). The role of gut microbiota in autoimmune disease progression. https://www.frontiersin.org/journals/microbiomes/articles/10.3389/frmbi.2025.1553243/full
- Global Autoimmune Institute. (2025, September 30). Symptoms & signs. https://www.autoimmuneinstitute.org/symptoms-signs/
- Global Autoimmune Institute. (2025, November 17). The spectrum of autoimmune disease treatments. https://www.autoimmuneinstitute.org/the-spectrum-of-autoimmune-disease-treatments/
- Global Autoimmune Institute. (2025, April 13). Culinary medicine: Autoimmunity and healthy eating. https://www.autoimmuneinstitute.org/articles/culinary-medicine-autoimmunity-and-healthful-eating/
- Harter Physical Therapy. (2024, November 6). Key rehabilitation strategies for sports injury recovery. https://harterphysicaltherapy.com/get-back-in-the-game-key-rehabilitation-strategies-for-sports-injuries/
- Harvard Nutrition Source. (2025, September 4). Diet review: Anti-inflammatory diet. https://nutritionsource.hsph.harvard.edu/healthy-weight/diet-reviews/anti-inflammatory-diet/
- Healthdirect. (2025, September 22). Autoimmune diseases – an overview. https://www.healthdirect.gov.au/autoimmune-diseases
- Healthline. (2020, August 24). AIP (autoimmune protocol) diet: A beginner’s guide. https://www.healthline.com/nutrition/aip-diet-autoimmune-protocol-diet
- IdealSpine. (2023, April 2). How chiropractic care can help with autoimmune disorders. https://idealspine.com/how-chiropractic-care-can-help-with-autoimmune-disorders/
- Integrative Medicine AZ. (2022, October 4). Autoimmune disorders and functional medicine: The key to lasting relief. https://integrativemedicineaz.com/autoimmune-disorders-and-functional-medicine-the-key-to-lasting-relief/
- LinkedIn. (2024). Dr. Alexander Jimenez, DC, APRN, FNP-BC, IFMCP, CFMP, ATN. https://www.linkedin.com/in/dralexjimenez
- Lupus News. (2022, January 30). Vitamin D and fish oil supplements for the prevention of autoimmune diseases like lupus. https://www.lupus.org/news/vitamin-d-and-fish-oil-supplements-for-prevention-of-autoimmune-diseases-like-lupus
- Mayo Clinic. (2022, October 20). Lupus – Symptoms & causes. https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789
- Mayo Clinic Health System. (2022, March 21). Benefits of massage therapy. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/benefits-of-massage-therapy
- Medical News Today. (2023, November 28). List of autoimmune diseases. https://www.medicalnewstoday.com/articles/list-of-autoimmune-diseases
- Medical News Today. (2024, February 14). Could vitamin D and omega-3 supplements help prevent autoimmune diseases? https://www.medicalnewstoday.com/articles/omega-3-supplements-vitamin-d-more-effective-preventing-autoimmune-diseases
- Medical News Today. (2025, March 10). The immune system: Cells, tissues, function, and disease. https://www.medicalnewstoday.com/articles/320101
- MGI Clinic. (2025, May 5). How stress and trauma contribute to autoimmune inflammation. https://www.mgiclinic.com/how-stress-and-trauma-contribute-to-autoimmune-inflammation-a-holistic-approach-to-healing/
- Nature. (2021, November 17). Role of sleep deprivation in immune-related disease risk and outcomes. https://www.nature.com/articles/s42003-021-02825-4
- NCBI. (2023, June 5). In brief: How does the immune system work? https://www.ncbi.nlm.nih.gov/books/NBK279364/
- NCBI. (2023, August 13). In brief: The innate and adaptive immune systems. https://www.ncbi.nlm.nih.gov/books/NBK279396/
- Nufactor. (2023, May 31). Sleep’s powerful effects on the immune system. https://www.nufactor.com/resources/ig/articles/ar-sleeps-powerful-effects-on-the-immune-system.html
- Oxford Academic. (2024, February 29). Gut microbiome and autoimmune disorders. https://academic.oup.com/rheumatology/article/63/3/856/7226506
- Ozark PT Specialists. (2024, October 9). Unlocking potential: Targeted exercises for athletes. https://ozarkptspecialists.com/unlocking-potential-targeted-exercises-for-athletes/
- Performance Health and Wellness. (2025, November 11). How a functional medicine approach helps autoimmune conditions. https://performhealthwellness.com/how-a-functional-medicine-approach-helps-autoimmune-conditions/
- Physician Partners of America. (n.d.). Three benefits of therapeutic massage for chronic pain. https://www.physicianpartnersofamerica.com/health-news/health-wellness/three-benefits-of-therapeutic-massage-for-chronic-pain/
- PMC. (2012, December 31). Core stability training for injury prevention. https://pmc.ncbi.nlm.nih.gov/articles/PMC3806175/
- PMC. (2015, March 31). Sleep disorders and increased risk of autoimmune diseases in individuals with non-apnea sleep disorders. https://pmc.ncbi.nlm.nih.gov/articles/PMC4355897/
- PMC. (2019, October 26). The dynamic interplay between the gut microbiota and autoimmune diseases. https://pmc.ncbi.nlm.nih.gov/articles/PMC6854958/
- PMC. (2021, December 20). The anti-inflammatory actions and mechanisms of acupuncture from the perspective of the neuro-immuno-endocrine network. https://pmc.ncbi.nlm.nih.gov/articles/PMC8710088/
- PMC. (2022, August 31). Potential role of sleep deficiency in inducing immune dysfunction. https://pmc.ncbi.nlm.nih.gov/articles/PMC9496201/
- PMC. (2023, October 3). The role of inflammation in autoimmune disease: a therapeutic target. https://pmc.ncbi.nlm.nih.gov/articles/PMC10584158/
- PMC. (2024, October 15). Overview of anti-inflammatory diets and their promising effects on non-communicable diseases. https://pmc.ncbi.nlm.nih.gov/articles/PMC11576095/
- PowersBeing. (2025). Unlock meditation’s healing powers for autoimmune disease. https://powersbeing.com/meditation-autoimmune-healing/
- PubMed. (2025, January 30). Acupuncture therapy in autoimmune diseases: A narrative review. https://pubmed.ncbi.nlm.nih.gov/39586390/
- QJM. (2024, March 26). Acupuncture and its ability to restore and maintain immune homeostasis. https://academic.oup.com/qjmed/article/117/3/167/7198587
- Renton Chiropractic Care. (2025, March 11). Massage therapy: A natural approach to alleviating chronic pain. https://www.rentonchiropracticcare.com/massage-therapy-a-natural-approach-to-alleviating-chronic-pain/
- Rheumatology Advisor. (2024, August 8). Omega-3 fatty acid supplements may offer protection against autoimmune disease. https://www.rheumatologyadvisor.com/news/n-3-fatty-acids-may-help-prevent-autoimmune-disease-beyond-discontontuation/
- Rupa Health. (2025, January 13). Functional medicine protocol for autoimmune diseases. https://www.rupahealth.com/post/functional-medicine-protocol-for-autoimmune-diseases-balancing-the-immune-system
- Simply PT. (2025, July 10). Preventing common sports injuries with physical therapy techniques. https://simplypt.com/preventing-common-sports-injuries-with-physical-therapy-techniques/
- South Island Physio. (2025, May 22). Exercise for injury prevention and sports injury rehabilitation. https://southislandphysio.ca/news/exercise-for-injury-prevention/
- Texas Health School. (2024, December 8). How does a massage therapist help with muscle pain? https://ths.edu/how-does-a-massage-therapist-help-with-muscle-pain/
- Tolpa Holistic Health. (2025, September 29). Natural treatment for autoimmune diseases: Holistic healing guide. https://tolpaholistichealth.com/natural-treatment-autoimmune-diseases-holistic-medicine/
- Tri-State Arthritis. (2025, May 20). 10 signs you may have an autoimmune disease. https://tristatearthritis.com/lupus/10-signs-you-may-have-an-autoimmune-disease/