Cognitive Impairment Overview With Traumatic Brain Injury
Learn how cognitive impairment relates to traumatic brain injury. Discover symptoms, diagnosis, and recovery strategies.
Introduction
One of the biggest health problems of our time is brain damage, which affects millions of individuals every year and has effects that endure long after the original injury. Over 30% of injury-related fatalities in the US include some kind of brain trauma, making traumatic brain injuries a leading cause of mortality and disability globally (Bailes & Borlongan, 2020). These wounds set off an intricate series of events that alter not only how the brain works but also how the body as a whole functions. missionlegalcenter Two separate stages of damage occur when a person gets a traumatic brain injury. The main harm occurs when external forces instantly induce mechanical damage to brain tissue at the point of contact. A secondary damage phase follows, when biochemical processes such as oxidative stress, inflammation, cell death, and other detrimental alterations cause the brain to gradually deteriorate over the course of days, weeks, and even months after the original trauma (Bailes & Borlongan, 2020). Healthcare professionals may create more effective treatment plans that address both short-term issues and long-term healing requirements by having a better understanding of these injury patterns. missionlegalcenter Cognitive impairment represents one of the most common and challenging consequences of traumatic brain injury. Problems with attention, memory, and executive functioning emerge as the primary neurocognitive consequences across all levels of injury severity (Cognitive Impairment Following Traumatic Brain Injury, 2002). These cognitive disruptions profoundly affect daily life, making it difficult for individuals to work, maintain relationships, manage household tasks, and participate fully in their communities. Because attention and memory serve as foundational cognitive abilities, their disruption can trigger additional problems with executive function, communication, and other complex mental processes (Cognitive Impairment Following Traumatic Brain Injury, 2002).pubmed.ncbi.nlm.nih
The connection between brain and body becomes especially important when considering traumatic brain injury recovery. The brain controls virtually every function in the human body through an intricate network of nerves and chemical signals. The central nervous system, comprising the brain and spinal cord, regulates awareness, movement, sensation, thought, speech, and memory (Anatomy and physiology of the nervous system, 2020). When injury disrupts these control centers, the effects ripple throughout the entire body, affecting muscles, bones, organs, and metabolic processes.cancer An integrative approach that combines chiropractic care with nurse practitioner oversight offers promising possibilities for individuals recovering from traumatic brain injuries. This collaborative model addresses the neurological, musculoskeletal, cognitive, emotional, and metabolic aspects of recovery. Chiropractic care focuses on restoring nervous system function through spinal adjustments, soft-tissue therapies, and targeted exercises, while nurse practitioners provide comprehensive medical management, cognitive support, and coordination of overall health needs. Together, these providers can create comprehensive treatment plans that support the brain’s natural healing processes and help patients regain function and improve their quality of life.
What is a Traumatic Brain Injury?
Traumatic brain injury refers to brain damage caused by an outside force that disrupts normal brain function. This external force can take many forms, including a forceful bump, blow, or jolt to the head or body, or an object penetrating the skull and damaging brain tissue (Traumatic Brain Injury, 2023). The injury occurs when the brain moves violently inside the skull or when an external object breaks through the skull barrier. Common causes include motor vehicle accidents, falls, sports injuries, violence, and blast exposures from explosions (Types of Traumatic Brain Injury, 2024).ninds.nih+1 Healthcare providers classify traumatic brain injuries according to their severity, which helps guide treatment decisions and predict outcomes. The three main categories include mild, moderate, and severe traumatic brain injury. Medical professionals use several measures to determine severity, including the Glasgow Coma Scale score, duration of loss of consciousness, length of post-traumatic amnesia, and results from brain imaging studies (Criteria used to classify TBI severity, 2012).ncbi.nlm.nih+1
- Mild traumatic brain injury, often called a concussion, generally does not cause prolonged loss of consciousness. If unconsciousness occurs, it typically lasts less than thirty minutes. The Glasgow Coma Scale score ranges from thirteen to fifteen for mild injuries. Common symptoms include headaches, dizziness, confusion, nausea, vision problems, difficulty thinking clearly, balance issues, sleep disturbances, sensitivity to light and sound, problems with attention and concentration, fatigue, anxiety, irritability, and emotional changes (4 Types of Brain Injuries and 3 Levels of Severity, 2021). Memory loss associated with mild traumatic brain injury usually lasts less than twenty-four hours. Most people with mild injuries recover within a few days to weeks with appropriate rest and management (4 Types of Brain Injuries and 3 Levels of Severity, 2021).missionlegalcenter
- Moderate traumatic brain injury involves unconsciousness lasting more than thirty minutes but less than twenty-four hours. The Glasgow Coma Scale score falls between nine and twelve. Individuals with moderate injuries experience all the symptoms associated with mild traumatic brain injury, plus additional concerning signs. These include headaches that worsen or do not improve, seizures or convulsions, numbness or weakness in the arms and legs, repeated vomiting, inability to wake from sleep, and slurred speech (4 Types of Brain Injuries and 3 Levels of Severity, 2021). Post-traumatic amnesia lasts more than one day but less than seven days. Brain imaging may show abnormalities such as bleeding, bruising, or swelling (Criteria used to classify TBI severity, 2012).ncbi.nlm.nih+1
- Severe traumatic brain injury represents the most serious category, with loss of consciousness exceeding twenty-four hours. The Glasgow Coma Scale score ranges from three to eight. Post-traumatic amnesia persists for more than seven days. Individuals with severe injuries often require intensive medical care and extended rehabilitation. They may experience altered consciousness states, including coma, vegetative state, or minimally conscious state (Traumatic Brain Injury, 2023). Brain imaging typically reveals significant abnormalities including bleeding within the brain tissue, bleeding over the brain surface, bleeding in the brain’s ventricles, swelling, and tissue damage (Types of Traumatic Brain Injury, 2024).medschool.ucla+1
The type of traumatic brain injury also provides important classification information. Closed head injuries occur when the head experiences impact or rapid movement without skull penetration. Concussions, diffuse axonal injury, and contusions fall into this category. Diffuse axonal injury, one of the most common types, involves widespread damage to the brain’s white matter, which contains nerve fibers that facilitate communication between different brain regions. This type of injury commonly happens in auto accidents, falls, and sports-related trauma (Traumatic Brain Injury, 2023). Penetrating brain injuries occur when an object breaks through the skull and enters brain tissue, as seen with gunshot wounds or impalement injuries (Types of Traumatic Brain Injury, 2024).ninds.nih+1 Understanding whether an injury is primary or secondary helps guide treatment approaches. Primary traumatic brain injury refers to the immediate structural damage inside the brain resulting directly from the initial impact. This includes bruising, bleeding, and tearing of brain tissue and blood vessels. Secondary traumatic brain injury describes complications that develop after the initial trauma and cause additional damage to an already compromised brain. Secondary injury mechanisms include increased pressure inside the skull, progressive brain swelling, damage to blood vessels triggering stroke or seizures, and lack of oxygen related to blood pressure drops or breathing difficulties (Types of Traumatic Brain Injury, 2024).medschool.ucla
How TBI Causes Cognitive Impairment
Traumatic brain injury triggers a complex series of events that disrupt normal brain function and lead to cognitive impairment. Understanding these mechanisms enables healthcare providers to develop targeted interventions that support recovery and effectively manage symptoms.
- The physical damage from traumatic brain injury affects brain structure and function in multiple ways. When the brain experiences trauma, nerve cells can be stretched, torn, or destroyed. The white matter tracts that connect different brain regions become damaged, disrupting the communication networks essential for coordinated brain function. Diffuse axonal injury particularly affects these communication pathways, as the nerve fibers that transmit signals between brain cells break down and lose their ability to conduct information efficiently (Traumatic Brain Injury, 2023).ninds.nih
- Bleeding within the brain creates additional problems. When blood vessels rupture, blood accumulates in spaces where it does not belong, creating pressure that compresses surrounding brain tissue. This compression damages cells both directly through physical pressure and indirectly by reducing blood flow to affected areas. Swelling further compounds these problems, as increased fluid within the rigid skull creates mounting pressure that can damage brain tissue and reduce oxygen delivery (Types of Traumatic Brain Injury, 2024).medschool.ucla
At the cellular level, traumatic brain injury initiates harmful biochemical cascades. Cell membranes become disrupted, allowing excessive calcium and sodium to enter neurons. This triggers a series of destructive processes including activation of enzymes that break down cellular components, production of free radicals that damage cell structures, mitochondrial dysfunction that impairs energy production, and release of inflammatory molecules that promote further injury (Bailes & Borlongan, 2020). These processes can continue for days, weeks, or even months after the initial injury, explaining why symptoms sometimes worsen or new problems emerge well after the traumatic event.missionlegalcenter
- Inflammation plays a particularly important role in post-traumatic brain injury cognitive impairment. Within seconds after trauma, inflammatory responses activate in the brain. The blood-brain barrier, which normally protects the brain from harmful substances in the bloodstream, becomes damaged and allows inflammatory cells and molecules to enter brain tissue. While some inflammation helps with healing and clearing damaged tissue, excessive or prolonged inflammation damages healthy brain cells and interferes with recovery. Inflammatory molecules affect neurotransmitter systems, disrupt nerve signaling, and impair the formation of new neural connections needed for cognitive recovery (Mesenchymal stem cell therapy alleviates the neuroinflammation, 2020).medicine.washu
Different brain regions show varying vulnerability to traumatic injury, which explains the specific cognitive impairments that develop. The frontal lobes, responsible for executive functions such as planning, decision-making, impulse control, and working memory, are particularly susceptible to damage from trauma. The temporal lobes, involved in memory formation and language processing, also commonly sustain injury. Damage to the hippocampus, a structure critical for forming new memories, explains why memory problems rank among the most frequent cognitive complaints after traumatic brain injury (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Attention and concentration problems emerge as foundational deficits following traumatic brain injury. Individuals may struggle to focus, pay attention to relevant information while filtering out distractions, or attend to more than one task at a time. This leads to restlessness, easy distractibility, difficulty finishing projects, problems carrying on conversations, and trouble sitting still for extended periods. Because attention skills serve as building blocks for higher-level cognitive abilities, people with attention problems often develop additional difficulties with memory, reasoning, and problem-solving (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Processing speed commonly slows after brain injury. Individuals take longer to understand what others are saying, need more time to follow directions, struggle to keep up with television shows or movies, require additional time to read and comprehend written material, and show delayed reactions to stimuli. This slowed processing affects everyday activities and can make tasks that were once automatic feel laborious and exhausting. The reduced reaction time poses particular concerns for activities requiring quick responses, such as driving (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Memory impairments manifest in various ways after traumatic brain injury. Short-term memory problems make it difficult to hold information in mind temporarily, such as remembering a phone number long enough to dial it or recalling items on a shopping list. Long-term memory difficulties affect the ability to store and retrieve information over extended periods. People may struggle to remember recent events, learn new information, or recall facts and procedures they previously knew well. Working memory, which involves holding and manipulating information simultaneously, becomes compromised, affecting complex cognitive tasks like mental arithmetic, following multi-step directions, and reasoning (Cognitive Impairment Following Traumatic Brain Injury, 2002).pubmed.ncbi.nlm.nih
- Executive function deficits represent another hallmark of traumatic brain injury cognitive impairment. Executive functions include the mental processes that help people plan activities, organize information, initiate tasks, monitor performance, shift between tasks flexibly, solve problems, make decisions, and control impulses. When these abilities become impaired, individuals struggle with goal-directed behavior, adapting to new situations, regulating emotions, and functioning independently in daily life (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
The Brain-Body Connection
The relationship between the brain and body represents one of the most fundamental aspects of human physiology. This intricate connection enables all body functions, from voluntary movements to unconscious processes that sustain life. Understanding this connection becomes especially important when considering how traumatic brain injury affects not just cognitive abilities but overall physical health and function.
- The central nervous system serves as the command center for the entire body. Made up of the brain and spinal cord, this system controls awareness, movements, sensations, thoughts, speech, and the five senses of seeing, hearing, feeling, tasting, and smelling (Central nervous system function, 2025). The brain manages most body functions by processing information from sensory receptors throughout the body and sending out instructions through an extensive network of nerves. The spinal cord acts as an extension of the brain, carrying messages between the brain and peripheral nerves that reach every part of the body (Central nervous system function, 2025).healthdirect
- The peripheral nervous system complements the central nervous system by connecting the brain and spinal cord to the rest of the body. This network of nerves and ganglia sends signals to and receives signals from the central nervous system, enabling two-way communication between the brain and body tissues. The peripheral nervous system divides into the somatic nervous system, which controls voluntary movements like walking and grasping objects, and the autonomic nervous system, which manages involuntary functions that the body performs automatically, such as breathing, heartbeat, digestion, and blood pressure regulation (Anatomy and physiology of the nervous system, 2020).cancer
- The autonomic nervous system further separates into two complementary branches that maintain balance in body functions. The sympathetic nervous system prepares the body for situations requiring strength, heightened awareness, or rapid response, commonly known as the fight-or-flight response. Activation of this system increases heart rate, elevates blood pressure, speeds breathing, dilates pupils, and increases metabolic rate. The parasympathetic nervous system creates opposite effects, returning heart rate and breathing to normal, constricting pupils, and slowing metabolism to conserve energy and promote rest and recovery (Anatomy and physiology of the nervous system, 2020).cancer
- Research demonstrates that the brain and body maintain constant, bidirectional communication through multiple pathways. Recent studies show that parts of the brain area controlling movement connect directly to networks involved in thinking, planning, and control of involuntary body functions such as blood pressure and heartbeat. This literal linkage of body and mind in brain structure helps explain phenomena like why anxiety makes people pace, why vagus nerve stimulation can alleviate depression, and why regular exercise improves mental outlook (Mind-body connection is built into brain, 2023).medicine.washu
- The vagus nerve exemplifies this brain-body connection. This cranial nerve carries signals between the brain and internal organs, providing information about organ function and regulating processes like digestion and heart rate. Signals traveling through the vagus nerve are coded independently by specialized neurons, allowing the brain to discriminate precisely among various body signals and respond appropriately. This sophisticated communication system enables the brain to monitor and adjust organ function continuously based on changing body needs and environmental demands (Revealing Communications Between Brain and Body, 2022).medicine.yale
- Blood flow represents another critical aspect of brain-body connection. The brain, despite constituting only about two percent of total body mass, consumes over twenty percent of the body’s glucose-derived energy. Continuous glucose metabolism supports neuronal signaling, as adenosine triphosphate, the cell’s energy currency, powers action potentials, maintains ionic gradients, and supports synaptic transmission. Because the brain cannot synthesize or store glucose independently, it depends entirely on glucose from dietary intake and blood circulation. Any disruption to blood flow or energy metabolism can significantly impair brain function (Metabolic hormones mediate cognition, 2009).sciencedirect
- The musculoskeletal system connects intimately with brain function through sensory feedback and motor control. Muscles contain specialized receptors that constantly send information to the brain about body position, movement, and force. This proprioceptive feedback allows the brain to coordinate movement, maintain posture, and adjust to environmental demands. The brain processes this information and sends motor commands back to muscles, enabling precise, coordinated movement. When traumatic brain injury disrupts these communication pathways, both sensory perception and motor control become impaired (Nervous System Function, 2024).clevelandclinic
- Hormonal systems provide another dimension of brain-body connection. The hypothalamus and pituitary gland, located deep within the brain, regulate hormonal signals that control growth, metabolism, reproduction, stress response, and many other functions. These structures form a feedback loop, with the hypothalamus releasing hormones that signal the pituitary gland, which then distributes hormones to various body systems including the adrenal glands, thyroid, reproductive organs, skin, bone, and muscle. This hormonal regulation affects mood, memory, metabolism, muscle mass, energy levels, stress response, and reproductive function (Neuroendocrine Disturbances Following TBI, 2023).biausa
- The immune system also maintains constant communication with the brain. Immune cells and inflammatory molecules can cross from the bloodstream into brain tissue, particularly when the blood-brain barrier becomes damaged following injury. The brain, in turn, can influence immune function through neural and hormonal signals. This bidirectional communication becomes particularly important following traumatic brain injury, when both local brain inflammation and systemic immune responses affect recovery and long-term outcomes (Multiorgan Dysfunction After Severe TBI, 2021).pmc.ncbi.nlm.nih
Causes and Symptoms of Cognitive Impairment
Cognitive impairment following traumatic brain injury arises from multiple interrelated causes that affect brain structure and function. Understanding these causes enables healthcare providers to identify risk factors, develop effective prevention strategies, and tailor targeted treatment approaches.
- The primary cause of cognitive impairment stems from direct damage to brain tissue at the moment of injury. When the brain experiences sudden acceleration, deceleration, or rotational forces, nerve cells stretch and tear, blood vessels rupture, and tissue bruises. The specific location and extent of damage determine which cognitive functions become impaired. Injuries to the frontal lobes typically affect executive functions, attention, and working memory. Damage to the temporal lobe disrupts memory formation and language processing. Parietal lobe injuries interfere with sensory processing and spatial awareness, while occipital lobe damage affects visual processing (Traumatic Brain Injury, 2023).ninds.nih
- Secondary injury mechanisms compound the initial damage. Swelling increases pressure within the rigid skull, compressing brain tissue and reducing blood flow. Bleeding creates masses that displace normal brain structures and increase intracranial pressure. Chemical imbalances develop as damaged cells release excessive amounts of neurotransmitters, particularly glutamate, which overstimulates neighboring neurons and triggers cell death. Free radicals produced during cellular metabolism damage cell membranes and DNA. Mitochondrial dysfunction impairs energy production, leaving neurons unable to maintain normal function. These secondary processes continue for days to weeks after the initial injury, explaining why cognitive symptoms may worsen or emerge gradually (Bailes & Borlongan, 2020).missionlegalcenter
- Inflammation represents a major contributor to cognitive impairment following traumatic brain injury. The inflammatory response activates within seconds after trauma and can persist for months or even years. While acute inflammation helps remove damaged tissue and initiate healing, chronic inflammation damages healthy neurons and interferes with recovery. Inflammatory molecules disrupt neurotransmitter systems, impair synaptic plasticity, reduce the production of growth factors needed for neural repair, and contribute to the ongoing death of brain cells. This persistent inflammation particularly affects cognitive functions requiring complex neural networks and plasticity, such as learning, memory consolidation, and executive function (Mesenchymal stem cell therapy alleviates the neuroinflammation, 2020).medicine.washu
- Disrupted blood flow contributes to cognitive impairment by reducing oxygen and nutrient delivery to brain tissue. Traumatic brain injury can damage blood vessels directly, alter blood pressure regulation, and trigger vasospasm where blood vessels constrict excessively. The brain requires constant, abundant blood supply to meet its high metabolic demands. Even brief or partial reductions in blood flow can impair neural function and contribute to cell death. Chronic reductions in cerebral blood flow may explain some persistent cognitive deficits that remain long after the initial injury (Long-term Consequences of TBI in Bone, 2018).pmc.ncbi.nlm.nih
- Hormonal disruptions following traumatic brain injury affect cognition through multiple pathways. The hypothalamus and pituitary gland, structures that regulate hormonal systems, are particularly vulnerable to traumatic injury due to their location and delicate structure. Damage to these areas causes hypopituitarism, a condition where insufficient hormone production affects growth, metabolism, stress response, and reproduction. Growth hormone deficiency, thyroid hormone deficiency, and sex hormone deficiencies all contribute to cognitive impairment, affecting memory, attention, processing speed, and executive function (Neuroendocrine Disturbances Following TBI, 2023).biausa
The symptoms of cognitive impairment following traumatic brain injury vary widely depending on injury severity, location, and individual factors. Attention and concentration problems rank among the most common complaints. Individuals struggle to focus on tasks, become easily distracted by environmental stimuli, have difficulty filtering out irrelevant information, and cannot maintain attention for extended periods. These problems make it challenging to follow conversations, complete work tasks, read for comprehension, or perform activities requiring sustained mental effort (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Memory impairments manifest in various ways. Short-term memory problems make it difficult to remember recent events, conversations, or instructions. People may repeatedly ask the same questions, forget appointments, or lose track of items. Long-term memory difficulties affect the ability to recall past events, previously learned information, or familiar procedures. Working memory deficits interfere with tasks requiring simultaneous information holding and manipulation, such as mental calculations, following multi-step directions, or reasoning through problems (Cognitive Impairment Following Traumatic Brain Injury, 2002).pubmed.ncbi.nlm.nih
- Processing speed reductions cause delays in understanding and responding to information. Individuals take longer to comprehend spoken or written language, need extra time to formulate responses, show slowed reaction times, and struggle to keep pace in conversations or fast-moving situations. This slowed processing affects virtually all cognitive tasks and creates frustration when individuals recognize their difficulties but cannot overcome them through effort alone (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Executive function deficits create problems with higher-order cognitive processes. People struggle with planning and organizing activities, initiating tasks without prompting, maintaining focus on long-term goals, shifting flexibly between tasks or mental sets, monitoring their own performance, solving novel problems, making sound decisions, and controlling impulses. These difficulties severely impact independence, as they interfere with managing finances, maintaining employment, keeping appointments, completing household tasks, and regulating behavior in social situations (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Communication problems often accompany cognitive impairment. Individuals may have difficulty finding the right words, organizing their thoughts coherently, following complex conversations, understanding nonliteral language like sarcasm or idioms, interpreting social cues, or maintaining appropriate topics in conversation. These challenges affect relationships and social participation, contributing to isolation and reduced quality of life (Cognitive Impairment Following Traumatic Brain Injury, 2002).pubmed.ncbi.nlm.nih
- Learning difficulties emerge when cognitive impairment affects the ability to acquire new information or skills. People need more repetition to learn new material, struggle to transfer learned skills to new situations, have difficulty recognizing patterns, and cannot efficiently organize information for storage and retrieval. These learning problems affect vocational rehabilitation, academic pursuits, and adaptation to life changes necessitated by the injury (Cognitive Impairment Following Traumatic Brain Injury, 2002).pubmed.ncbi.nlm.nih
Effects on Musculoskeletal and Neurological Systems
Traumatic brain injury creates widespread effects throughout the musculoskeletal and neurological systems, affecting movement, coordination, sensation, and physical integrity. These effects arise from both direct injury to neural structures that control these systems and secondary changes that develop over time. The musculoskeletal system experiences significant impacts following traumatic brain injury through multiple mechanisms. Spasticity, characterized by increased muscle tone and involuntary muscle contractions, develops in a substantial proportion of individuals with moderate to severe traumatic brain injury. The degree of spasticity varies from mild muscle stiffness to severe, painful, uncontrollable muscle spasms. Affected muscles may resist passive stretching, contract involuntarily, and develop shortened resting length over time. Spasticity interferes with movement, positioning, comfort, and functional activities. It can lead to joint contractures, pain, skin breakdown, and difficulty with daily care (TBI-Induced Spasticity, 2015).ncbi.nlm.nih
- Muscle weakness and paralysis occur when traumatic brain injury damages motor cortex areas or descending motor pathways that transmit movement commands from brain to muscles. The pattern and severity of weakness depend on injury location. Hemiparesis, weakness affecting one side of the body, develops when injury occurs to motor areas in one brain hemisphere. Quadriparesis involves weakness in all four limbs. Even mild weakness significantly impacts function, affecting walking, reaching, grasping, and other essential movements. Muscle atrophy, or wasting, develops over time when muscles cannot be used normally due to weakness or inactivity (Physical effects of brain injury, n.d.).headway
- Balance and coordination problems represent common musculoskeletal consequences of traumatic brain injury. Damage to the cerebellum, a brain structure that coordinates movement, causes ataxia characterized by unsteady gait, difficulty with fine motor tasks, tremor during purposeful movements, and impaired ability to judge distances. Balance problems also arise from vestibular system damage, proprioceptive deficits, visual processing impairments, and motor control difficulties. These balance and coordination deficits increase fall risk, limit mobility, and reduce independence in daily activities (Physical effects of brain injury, n.d.).headway
- Post-traumatic seizures develop in some individuals following traumatic brain injury, representing neurological system dysfunction. Seizures can occur immediately after injury, within the first week, or months to years later. They result from abnormal electrical activity in damaged brain tissue. The risk increases with injury severity, presence of bleeding in the brain, skull fractures, and penetrating injuries. Seizures interfere with daily activities, increase injury risk, and may worsen cognitive impairment if not well controlled (Traumatic Brain Injury, 2023).ninds.nih
- Sensory disturbances commonly accompany traumatic brain injury. Individuals may experience numbness, tingling, burning sensations, or altered temperature perception. Pain syndromes develop, including headaches, neck pain, and widespread body pain. These sensory changes result from damage to sensory processing areas in the brain, peripheral nerves, or spinal structures often injured concurrently with traumatic brain injury. Chronic pain significantly affects quality of life, mood, sleep, and rehabilitation participation (Pain and Traumatic Brain Injury, 2024).health
- Vestibular dysfunction affects up to fifty percent of traumatic brain injury patients at five years post-injury. The vestibular system, which controls balance and spatial orientation, can be damaged at the peripheral level in the inner ear, at the central level in the brain, or both. Common vestibular diagnoses following traumatic brain injury include benign paroxysmal positional vertigo, where calcium crystals in the inner ear become displaced causing brief spinning sensations with position changes; acute unilateral peripheral vestibular loss, where one inner ear loses function; and migraine-associated vertigo. Vestibular dysfunction causes dizziness, vertigo, imbalance, nausea, and difficulty with activities requiring head movement. Interestingly, many individuals with objective vestibular dysfunction do not report symptoms, likely because traumatic brain injury affects perceptual mechanisms (Vestibular dysfunction in acute TBI, 2019).pmc.ncbi.nlm.nih
- Vision and eye movement problems affect up to ninety percent of traumatic brain injury patients. These problems include difficulty tracking moving objects smoothly, impaired ability to shift gaze rapidly between targets, reduced convergence ability needed for near vision tasks, double vision from misalignment of the eyes, difficulty focusing, reduced visual field, and light sensitivity. These visual disturbances result from damage to cranial nerves that control eye muscles, brain areas that process visual information, or brain regions that coordinate eye movements. Visual dysfunction significantly impacts reading, driving, balance, and participation in rehabilitation activities (Eye Movement Problems After Brain Injury, 2021).optometrists+1
- The skeletal system experiences long-term consequences from traumatic brain injury that are less obvious but clinically significant. Research shows that traumatic brain injury patients have increased risk of osteopenia and osteoporosis, conditions characterized by reduced bone mineral density and increased fracture risk. Bone loss occurs through multiple mechanisms, including reduced physical activity, hormonal disruptions affecting bone metabolism, vitamin D deficiency, inflammation, and altered bone formation and resorption signaling. Adults with traumatic brain injury show accelerated bone mineral density loss in the femur, particularly within the first year after injury. This increased skeletal fragility raises concern for future fractures that could complicate recovery and independence (Long-term Consequences of TBI in Bone, 2018).pmc.ncbi.nlm.nih
- Heterotopic ossification, the formation of bone in soft tissues where bone should not normally exist, develops in some traumatic brain injury patients. This condition commonly affects muscles and soft tissues around major joints, particularly the hips, knees, elbows, and shoulders. Heterotopic ossification causes pain, limits joint range of motion, and interferes with positioning and movement. The mechanisms involve altered signaling from the injured brain that activates bone-forming cells in abnormal locations, increased inflammation, and changes in local blood flow (Long-term Consequences of TBI in Bone, 2018).pmc.ncbi.nlm.nih
Effects on Vital Organs
Traumatic brain injury extends its impact beyond the brain to affect vital organs throughout the body. This multiorgan dysfunction occurs through autonomic nervous system disruption, inflammatory mediators, hormonal changes, and metabolic alterations that the injured brain cannot properly regulate.
- The cardiovascular system experiences significant effects following traumatic brain injury. Severe injuries trigger massive catecholamine release and autonomic nervous system activation, leading to elevated heart rate, increased blood pressure, and altered heart rhythm. While these changes may initially help maintain blood flow to the injured brain, they can become harmful if excessive or prolonged. Cardiac complications include neurogenic stress cardiomyopathy, where the heart muscle weakens temporarily; cardiac arrhythmias; and increased myocardial oxygen demand that can trigger ischemia in vulnerable individuals. Blood pressure dysregulation complicates management, as both very high and very low blood pressure can worsen brain injury outcomes (Multiorgan Dysfunction After Severe TBI, 2021).pmc.ncbi.nlm.nih
- The pulmonary system suffers frequent complications after traumatic brain injury. Acute lung injury develops in many patients with severe brain trauma due to neurogenic pulmonary edema, where fluid accumulates in the lungs from autonomic nervous system dysfunction and altered blood vessel permeability. Pneumonia occurs frequently due to impaired ability to protect the airway, reduced cough effectiveness, and prolonged mechanical ventilation when required. Acute respiratory distress syndrome, a severe form of lung injury, can develop. These pulmonary complications reduce oxygen delivery to the injured brain and other organs, potentially worsening outcomes (Multiorgan Dysfunction After Severe TBI, 2021).pmc.ncbi.nlm.nih
- The gastrointestinal system demonstrates vulnerability to traumatic brain injury effects. Autonomic nervous system disruption alters gut motility, reduces blood flow to intestinal tissues, and changes the gut microbiome composition. These changes increase intestinal permeability, potentially allowing bacteria and bacterial products to enter the bloodstream. Stress ulcers develop in the stomach and duodenum from reduced mucosal blood flow and altered protective mechanisms. Feeding intolerance complicates nutritional support. Gastrointestinal complications affect nutrient absorption, contribute to systemic inflammation, and may influence brain recovery (Multiorgan Dysfunction After Severe TBI, 2021).pmc.ncbi.nlm.nih
- Kidney function becomes impaired in many traumatic brain injury patients through multiple mechanisms. Sympathetic nervous system activation reduces blood flow to the kidneys, decreasing glomerular filtration. Inflammatory mediators released from the injured brain affect kidney cells directly. Acute kidney injury develops in a significant proportion of patients with severe traumatic brain injury, potentially requiring dialysis and affecting long-term kidney function. Impaired kidney function complicates medication dosing, fluid management, and elimination of metabolic waste products (Multiorgan Dysfunction After Severe TBI, 2021).pmc.ncbi.nlm.nih
- The liver, which synthesizes proteins and lipids crucial for brain recovery, experiences altered function following traumatic brain injury. Inflammatory signals affect hepatic protein synthesis, lipid metabolism, and glucose production. The liver may become a source of inflammatory mediators that worsen brain injury. Liver dysfunction affects drug metabolism, coagulation factor production, and nutritional status. Recent research suggests the liver plays a crucial role in traumatic brain injury pathogenesis through its metabolic and inflammatory functions (Traumatic brain injury from a peripheral axis perspective, 2025).sciencedirect
- Metabolic and endocrine systems show widespread dysfunction after traumatic brain injury. The hypothalamic-pituitary axis, which regulates hormonal systems, commonly sustains damage. This results in deficiencies of growth hormone, thyroid hormone, adrenal hormones, and sex hormones. Growth hormone deficiency contributes to muscle wasting, bone loss, fatigue, and cognitive impairment. Thyroid hormone deficiency slows metabolism, affects mood and cognition, and impairs recovery. Adrenal insufficiency compromises stress response and blood pressure regulation. Sex hormone deficiencies affect mood, energy, muscle mass, and bone density. These hormonal disturbances can develop acutely or emerge months to years after injury, emphasizing the need for ongoing monitoring (Neuroendocrine Disturbances Following TBI, 2023).biausa
- Blood sugar regulation becomes disrupted following traumatic brain injury, with both hyperglycemia and hypoglycemia occurring. The injured brain has altered glucose metabolism and increased metabolic demands. Insulin resistance can develop, affecting cellular energy metabolism throughout the body. These metabolic changes complicate nutritional management and may affect recovery outcomes. Evidence suggests that metabolic dysregulation contributes to cognitive impairment, as insulin and other metabolic hormones influence neuroplasticity and synaptic function (Metabolic hormones mediate cognition, 2009).sciencedirect
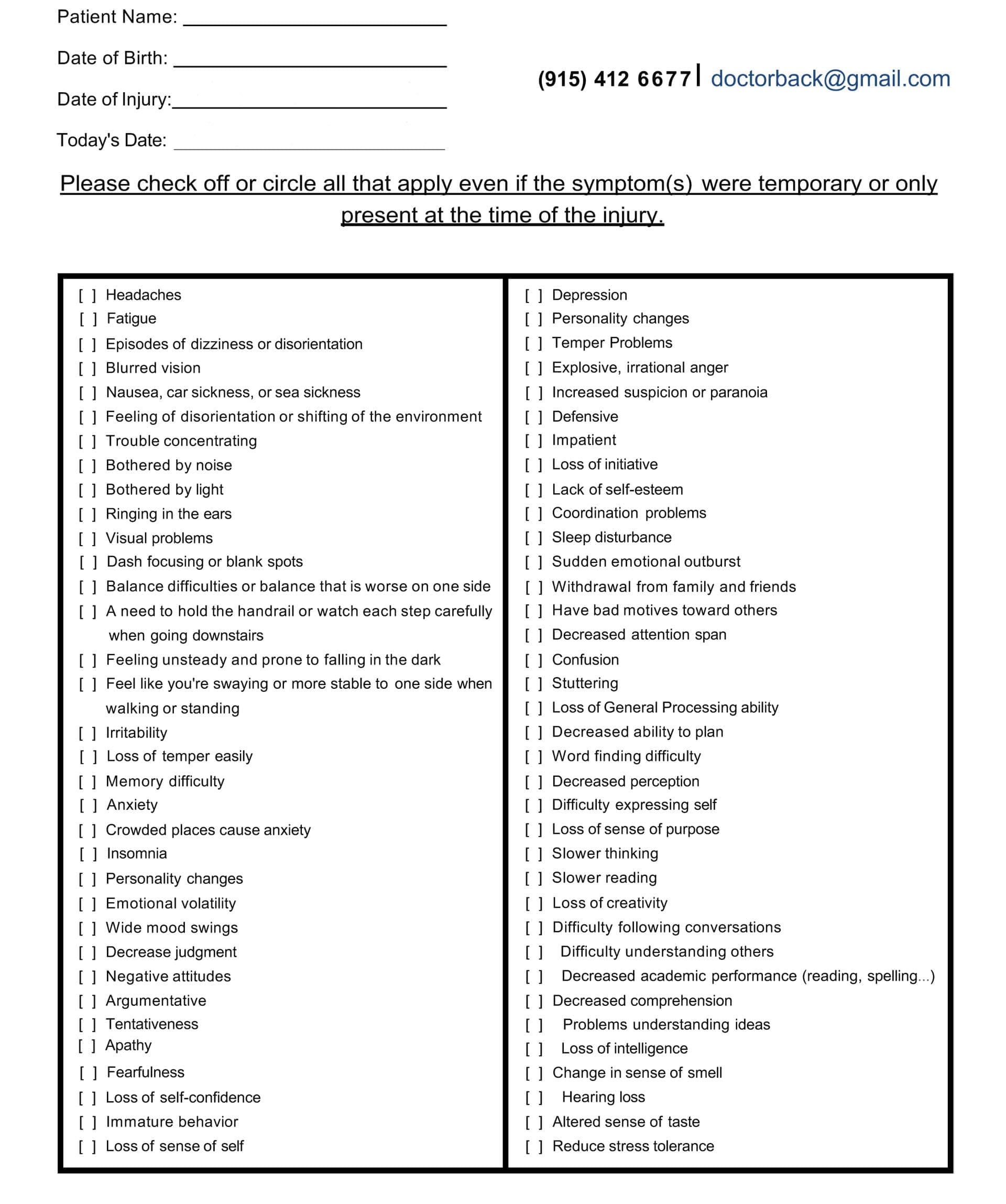
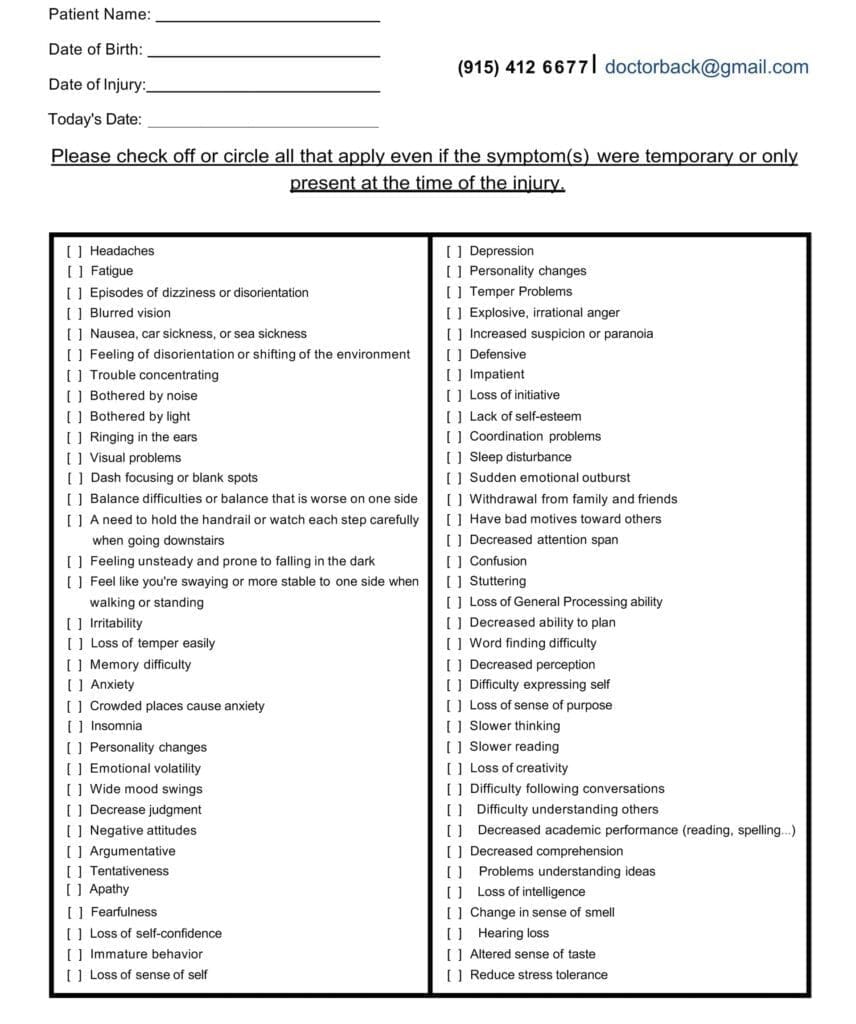
A TBI Symptom Questionnaire Example:
Detailed History and Questioning by Providers
Comprehensive assessment through detailed history-taking and systematic questioning forms the foundation of effective traumatic brain injury care. Both chiropractors and nurse practitioners use specific strategies to uncover cognitive impairment and identify the full scope of injury-related problems. A thorough history begins with understanding the mechanism of injury. Providers need detailed information about how the traumatic event occurred, including the forces involved, direction of impact, presence of acceleration or deceleration, rotational forces, and any loss of consciousness. This information helps predict injury patterns and potential complications. For example, motor vehicle accidents often cause both brain injury and cervical spine trauma, blast injuries affect multiple organ systems, and falls in older adults carry high risk for bleeding complications (Survey of chiropractic clinicians on MTBI, 2018).pmc.ncbi.nlm.nih
- Timeline documentation provides essential context for symptom development. Providers should ask when symptoms first appeared, whether they emerged immediately after injury or developed gradually, how symptoms have changed over time, and whether any factors make symptoms better or worse. Some traumatic brain injury symptoms appear immediately, while others develop days, weeks, or months later. This temporal pattern helps distinguish primary injury effects from secondary complications and guides treatment planning (Survey of chiropractic clinicians on MTBI, 2018).pmc.ncbi.nlm.nih Cognitive symptoms require detailed exploration through specific questioning. Providers should systematically assess attention and concentration by asking about distractibility, ability to complete tasks, difficulty maintaining focus during conversations or activities, and need for frequent breaks. Memory problems should be explored across multiple domains, including difficulty remembering recent events, appointments, or conversations; problems with learning new information; struggles with recalling previously known facts or procedures; and concerns expressed by family members about changes in memory. Executive function difficulties often manifest as problems with planning, organizing, initiating tasks, managing time, making decisions, solving problems, and regulating emotions (Cognitive Problems After Traumatic Brain Injury, n.d.).uwmsktc.washington
- Musculoskeletal symptoms deserve thorough investigation because they often accompany cognitive impairment and affect rehabilitation. Providers should ask about neck pain, back pain, headaches, dizziness, balance problems, muscle weakness, numbness or tingling, muscle stiffness or spasms, and changes in coordination or movement. The cervical spine frequently sustains injury concurrently with traumatic brain injury, and cervical dysfunction can contribute to headaches, dizziness, and cognitive symptoms through its effects on blood flow and proprioceptive input (Chiropractic Management of Post Traumatic Vertigo, 2004).pmc.ncbi.nlm.nih Vestibular symptoms require specific questioning because they are common but often underreported. Providers should directly ask about dizziness, vertigo, lightheadedness, imbalance, motion sensitivity, visual disturbances with movement, and situations that provoke symptoms. Many traumatic brain injury patients have vestibular dysfunction but do not report symptoms spontaneously, possibly because brain injury affects symptom perception. Direct questioning reveals these problems that might otherwise remain unidentified (Vestibular dysfunction in acute TBI, 2019).pmc.ncbi.nlm.nih
- Visual symptoms affect the majority of traumatic brain injury patients and significantly impact function. Providers should systematically assess blurred vision, double vision, difficulty focusing, eye strain, light sensitivity, problems tracking moving objects, difficulty with reading, visual field deficits, and eye misalignment. Because visual dysfunction contributes to balance problems, reading difficulties, and participation limitations, thorough visual assessment guides appropriate referrals and treatment planning (Eye Movement Problems After Brain Injury, 2021).optometrists Sleep disturbances occur in thirty to seventy percent of traumatic brain injury patients and affect recovery. Providers should ask about difficulty falling asleep, frequent nighttime awakenings, early morning awakening, excessive daytime sleepiness, prolonged sleep need, nightmares, and changes in sleep schedule or quality. Sleep disruption worsens cognitive function, mood, pain perception, and overall recovery. Identifying sleep problems allows targeted interventions that may improve multiple outcome domains (Sleep Disorders After Brain Injury, 2025).practicalneurology
- Mood and emotional symptoms commonly develop after traumatic brain injury and require sensitive, direct questioning. Depression affects forty to sixty percent of individuals with moderate to severe traumatic brain injury. Symptoms include persistent sadness, loss of interest in previously enjoyed activities, feelings of hopelessness, changes in appetite, sleep disturbances, fatigue, difficulty concentrating, and suicidal thoughts. Anxiety disorders affect eleven to seventy percent of traumatic brain injury patients, with symptoms including excessive worry, restlessness, tension, hypervigilance, and panic attacks. Emotional dysregulation may manifest as irritability, anger outbursts, emotional lability, or apathy (Mood Disorders Following TBI, 2025).practicalneurology
Functional impacts should be thoroughly explored to understand how symptoms affect daily life. Providers should ask about changes in work or school performance, difficulty managing household tasks, problems maintaining relationships, challenges with self-care activities, driving limitations, and overall quality of life. Understanding functional limitations helps prioritize treatment goals and measure progress over time. Family member or caregiver input provides valuable perspective on functional changes that patients may not fully recognize (Strategies Nurses Use when Caring for Patients with TBI, 2019).pmc.ncbi.nlm.nih Inquiry about significant others’ observations proves particularly valuable, as cognitive impairment can affect self-awareness. Studies show that seventy to eighty-eight percent of healthcare providers inquire about family members’ observations of cognitive changes. Family members often notice personality changes, memory problems, emotional shifts, and functional declines that patients minimize or do not recognize (Survey of chiropractic clinicians on MTBI, 2018).pmc.ncbi.nlm.nih
Associated Symptoms from TBI
Beyond cognitive impairment, traumatic brain injury produces a constellation of associated symptoms that significantly affect quality of life and recovery. Understanding these symptoms helps providers develop comprehensive treatment approaches and set realistic expectations for recovery.
- Fatigue represents one of the most common and debilitating symptoms after traumatic brain injury. Research indicates that as many as ninety-eight percent of people who have experienced traumatic brain injury have some form of fatigue. This fatigue differs from normal tiredness in that it does not improve adequately with rest, appears disproportionate to activity level, and significantly limits function. Physical fatigue manifests as muscle weakness, reduced endurance, and increased need for rest. Mental fatigue involves reduced ability to sustain cognitive effort, difficulty concentrating as the day progresses, and overwhelming sense of mental exhaustion. Fatigue worsens other symptoms, including pain, cognitive problems, and mood disturbances (Fatigue After Brain Injury, 2021).biausa
- Headaches affect up to eighty percent of traumatic brain injury survivors and may persist for months or years. Post-traumatic headaches take various forms, including tension-type headaches characterized by band-like pressure, migraine-type headaches with throbbing pain and associated symptoms, cervicogenic headaches originating from neck dysfunction, and neuralgic headaches involving specific nerve distributions. Headaches interfere with concentration, sleep, mood, and participation in rehabilitation activities. The mechanisms involve inflammation, altered pain processing, muscle tension, cervical spine dysfunction, and vascular changes (Traumatic Brain Injury, 2023).ninds.nih
- Sleep disorders affect thirty to seventy percent of traumatic brain injury patients and take various forms. Insomnia, characterized by difficulty initiating or maintaining sleep, affects approximately twenty-nine percent of patients. Sleep apnea, where breathing repeatedly stops during sleep, occurs in about twenty-five percent. Hypersomnia, excessive sleepiness or prolonged sleep need, affects twenty-eight percent. Narcolepsy develops in approximately four percent. These sleep disturbances result from damage to brain structures regulating sleep-wake cycles, hormonal disruptions affecting sleep, pain interfering with rest, and mood disturbances. Poor sleep quality worsens cognitive function, mood, pain, fatigue, and overall recovery (Impact of TBI on sleep, 2019).pmc.ncbi.nlm.nih
- Depression emerges as a frequent complication, affecting thirteen to fifty-three percent of traumatic brain injury survivors. Post-traumatic depression may result from direct brain damage affecting mood-regulating circuits, particularly in frontotemporal regions, or from psychological response to injury-related losses and life changes. Symptoms include persistent sadness, loss of interest, feelings of worthlessness, guilt, changes in appetite and sleep, fatigue, difficulty concentrating, psychomotor agitation or retardation, and suicidal ideation. Depression significantly impairs rehabilitation participation, functional recovery, and quality of life. It increases caregiver burden and raises risk of suicide (Mood Disorders Following TBI, 2025).pmc.ncbi.nlm.nih+1
- Anxiety disorders develop in eleven to seventy percent of traumatic brain injury patients. Post-traumatic stress disorder occurs particularly in those whose injuries resulted from violence, combat, or accidents. Generalized anxiety disorder involves excessive, uncontrollable worry about multiple life domains. Panic disorder includes unexpected panic attacks with physical symptoms like rapid heartbeat, sweating, trembling, and fear of dying. Social anxiety involves fear of social situations and negative evaluation. Anxiety often co-occurs with depression and exacerbates cognitive symptoms, sleep problems, and pain (Anxiety and Depression Following TBI, 2023).connectivity+1
- Irritability and emotional dysregulation commonly follow traumatic brain injury, resulting from damage to frontal lobe regions that regulate emotions and control impulses. Individuals may experience frequent anger, decreased frustration tolerance, emotional outbursts disproportionate to triggers, rapid mood shifts, and difficulty calming down once upset. These symptoms strain relationships, interfere with community reintegration, and may limit employment options (Traumatic brain injury and mood disorders, 2020).pmc.ncbi.nlm.nih
- Sensory sensitivities develop in many traumatic brain injury survivors. Light sensitivity, or photophobia, makes normal lighting uncomfortable and can trigger headaches. Noise sensitivity causes ordinary sounds to seem overwhelmingly loud or irritating. Some individuals develop increased sensitivity to touch, temperature, or smells. These sensitivities result from altered sensory processing in the injured brain and often accompany headaches and cognitive symptoms. They limit participation in bright or noisy environments and affect quality of life (Traumatic Brain Injury, 2023).ninds.nih
Beyond the Surface: Understanding the Effects of Personal Injury- Video
Integrative Approach: Chiropractic and Nurse Practitioner Care
An integrative approach combining chiropractic care with nurse practitioner oversight offers comprehensive support for individuals recovering from traumatic brain injuries. This collaborative model addresses the complex, multifaceted nature of brain injury by bringing together complementary expertise and treatment approaches. Chiropractic care focuses on the nervous system and musculoskeletal health through manual therapies, rehabilitative exercises, and supportive interventions. Chiropractors assess and address spinal alignment, particularly in the cervical spine which commonly sustains injury alongside traumatic brain injury. Cervical spine dysfunction contributes to many post-traumatic brain injury symptoms, including headaches, neck pain, dizziness, balance problems, and potentially cognitive symptoms through effects on blood flow and proprioceptive input (Chiropractic Care Supports TBI Healing, 2009).pinnaclehealthchiro
- Spinal adjustments form a core component of chiropractic care for traumatic brain injury patients. These precise, controlled movements applied to spinal joints aim to restore proper alignment, reduce nerve interference, and optimize nervous system function. In the cervical spine, adjustments may improve blood flow to the brain by reducing compression on vertebral arteries. Research demonstrates that correction of cervical lordosis associates with immediate increases in cerebral blood flow, suggesting that biomechanical improvements can positively affect brain perfusion (Cervical lordosis correction increases cerebral blood flow, 2019).pmc.ncbi.nlm.nih
- Chiropractic care addresses cerebrospinal fluid circulation, which plays important roles in brain health and recovery. Cerebrospinal fluid protects and nourishes the brain, removes metabolic waste products, and facilitates nutrient delivery. Traumatic brain injury can disrupt normal cerebrospinal fluid flow. Manual chiropractic techniques and spinal adjustments may help restore optimal cerebrospinal fluid dynamics, supporting brain healing processes (Chiropractic Care Supports TBI Healing, 2009).pinnaclehealthchiro
- Soft tissue therapies complement spinal adjustments by addressing muscle tension, fascial restrictions, and myofascial pain that commonly develop after trauma. Techniques include manual therapy, instrument-assisted soft tissue mobilization, therapeutic massage, and trigger point release. These interventions reduce pain, improve tissue quality, restore range of motion, and promote healing. Addressing soft tissue dysfunction proves particularly important for cervical and upper thoracic regions where muscle tension contributes to headaches and affects cervical spine mechanics (Chiropractic Care Supports TBI Healing, 2009).elpasochiropractorblog+1
Rehabilitative exercises form an essential component of chiropractic traumatic brain injury care. Exercise programs address specific deficits identified through comprehensive assessment. Cervical strengthening and stabilization exercises improve neck muscle function and support spinal structures. Vestibular rehabilitation exercises help retrain balance systems through specific movements and visual tasks. Oculomotor exercises address eye tracking and coordination problems. Proprioceptive training improves body position awareness and motor control. Progressive strengthening builds overall fitness and supports functional recovery (Therapeutic Interventions for TBI, 2024).physio-pedia
Chiropractic neurologists employ specialized techniques to stimulate nervous system recovery. These approaches use specific sensory inputs, including light, sound, movement, and other stimuli, to activate targeted brain regions and promote neuroplasticity. The principle recognizes that the brain responds to appropriate stimulation similarly to how muscles respond to exercise, strengthening neural pathways through repeated activation. This non-invasive approach may benefit patients who have not responded well to traditional treatments (Chiropractic Neurology Supports Brain Healing, 2025).hmlfunctionalcare+1 Nurse practitioners provide medical oversight and management that complements chiropractic interventions. As board-certified family practice nurse practitioners with advanced training, they perform comprehensive health assessments, order and interpret diagnostic tests, prescribe medications when appropriate, manage medical comorbidities, and coordinate care across specialties. This medical oversight ensures that serious complications are identified and addressed promptly while supporting the body’s natural healing processes (Dr. Alex Jimenez’s Integrative Practice, n.d.).missionlegalcenter
- Cognitive support represents an important aspect of nurse practitioner care for traumatic brain injury patients. Nurse practitioners assess cognitive function using standardized tools, provide education about cognitive symptoms and compensatory strategies, recommend cognitive rehabilitation services, and monitor cognitive recovery over time. They help patients and families understand cognitive changes and develop practical approaches to manage daily activities despite cognitive limitations (Strategies Nurses Use when Caring for Patients with TBI, 2019).nursing.duke+1
- Metabolic and nutritional support provided by nurse practitioners addresses the altered metabolic demands following traumatic brain injury. The injured brain has increased energy requirements and specific nutritional needs. Nurse practitioners assess nutritional status, develop individualized nutrition plans, recommend supplements when indicated, and monitor response to nutritional interventions. Emerging research suggests that specific nutrients, including omega-3 fatty acids, vitamin D, magnesium, and amino acids, may support brain recovery when provided during the acute and subacute phases after injury (Nutritional interventions to support acute mTBI recovery, 2022).frontiersin
- Emotional and psychological support forms another critical component of nurse practitioner care. They screen for depression, anxiety, post-traumatic stress disorder, and other mood disturbances, provide counseling and supportive therapy, prescribe psychotropic medications when appropriate, and refer to mental health specialists when needed. Addressing emotional health proves essential for overall recovery, as mood disturbances affect rehabilitation participation, cognitive function, and quality of life (Mood Disorders Following TBI, 2025).practicalneurology
- Sleep management represents an area where nurse practitioner expertise particularly benefits traumatic brain injury patients. Nurse practitioners assess sleep quality and quantity, identify specific sleep disorders, recommend sleep hygiene improvements, prescribe sleep aids when appropriate, and coordinate sleep studies when indicated. Improving sleep quality enhances cognitive function, mood, pain management, and overall recovery (Sleep Disorders After Brain Injury, 2025).practicalneurology
The integrative model exemplified by Dr. Alexander Jimenez’s dual-scope practice demonstrates how chiropractic and nurse practitioner expertise can be combined within a single provider or collaborative team. Dr. Jimenez’s approach incorporates functional medicine principles, detailed health assessments, spinal and musculoskeletal care, nutritional support, exercise therapy, and comprehensive medical case management. This holistic model addresses the person as a whole rather than treating isolated symptoms, potentially leading to more complete and sustained recovery (Dr. Alex Jimenez’s Integrative Practice, n.d.).elpasochiropractorblog+1
Holistic Treatment Plans
Comprehensive, holistic treatment plans for traumatic brain injury incorporate multiple therapeutic approaches that address physical, cognitive, emotional, and metabolic aspects of recovery. These plans recognize that healing requires supporting the body’s natural recovery mechanisms while addressing specific symptoms and functional limitations.
- Initial assessment forms the foundation of effective treatment planning. Comprehensive evaluation includes detailed history of the injury and symptom development, neurological examination assessing mental status, cranial nerves, motor function, sensory function, reflexes, coordination, and gait. Cervical spine assessment evaluates posture, range of motion, segmental mobility, muscle tone and strength, and joint function. Vestibular and oculomotor testing examines balance, eye movements, and visual-vestibular integration. Cognitive screening identifies attention, memory, processing speed, and executive function deficits. Mood and sleep questionnaires quantify emotional and sleep-related symptoms (Hidden TBI Symptoms: Integrative Model, 2025).elpasochiropractorblog
- Spinal care targets cervical and upper thoracic dysfunction that commonly accompanies traumatic brain injury. Treatment begins with gentle mobilization techniques before progressing to specific adjustments as tolerated. The approach remains cautious, individualized, and responsive to patient symptoms, as excessive or aggressive treatment could worsen symptoms in vulnerable patients. Spinal adjustments aim to restore proper alignment, reduce nerve interference, improve proprioceptive input, and enhance blood flow to the brain. Treatment frequency and intensity adapt based on patient response, with some individuals benefiting from frequent initial visits that taper as function improves (Hidden TBI Symptoms: Integrative Model, 2025).zakerchiropractic+1
- Soft tissue interventions address muscle tension, trigger points, fascial restrictions, and movement dysfunction. Manual therapy techniques include ischemic compression for trigger points, myofascial release for fascial restrictions, instrument-assisted soft tissue mobilization to address tissue quality, and therapeutic massage for overall relaxation and pain relief. These interventions reduce pain, improve tissue flexibility, restore normal movement patterns, and support overall healing. Treatment focuses particularly on cervical, upper thoracic, and cranial regions where soft tissue dysfunction contributes to headaches, neck pain, and dizziness (Hidden TBI Symptoms: Integrative Model, 2025).elpasochiropractorblog
- Exercise therapy progresses systematically based on symptom tolerance and functional goals. Early-phase exercises focus on gentle range of motion, postural awareness, and basic strengthening within symptom limits. As tolerance improves, exercises advance to include cervical stabilization training to support injured structures, vestibular rehabilitation exercises to retrain balance systems, oculomotor exercises to improve eye coordination and tracking, proprioceptive training to enhance body position awareness, and progressive aerobic and strengthening exercises to build overall fitness. Exercise prescription follows graduated principles, starting with brief, low-intensity activities and progressing gradually while monitoring for symptom exacerbation (Hidden TBI Symptoms: Integrative Model, 2025).elpasochiropractorblog
- Nutritional support addresses the increased metabolic demands and specific nutrient needs following traumatic brain injury. The injured brain requires adequate calories, high-quality protein for tissue repair, essential fatty acids particularly omega-3s for neural membrane health and anti-inflammatory effects, antioxidants to combat oxidative stress, vitamins and minerals for metabolic processes and neurotransmitter synthesis, and adequate hydration for optimal brain function. Nutritional assessment identifies deficiencies and guides supplement recommendations. Evidence suggests that omega-3 fatty acids, vitamin D, magnesium, and certain amino acids may support brain recovery when provided during acute and subacute phases (Nutritional interventions to support acute mTBI recovery, 2022).pmc.ncbi.nlm.nih+1
- Cognitive rehabilitation strategies help individuals compensate for cognitive impairments and retrain affected abilities. Techniques include external memory aids such as written schedules, calendars, lists, and electronic reminders; attention strategies like reducing distractions, taking breaks, and focusing on one task at a time; organization systems that simplify and structure tasks; time management tools that help with planning and prioritization; and specific cognitive exercises that challenge and strengthen affected abilities. Education helps patients and families understand cognitive changes and develop realistic expectations while maintaining hope for continued improvement (Strategies Nurses Use when Caring for Patients with TBI, 2019).nursing.duke+1
- Sleep optimization represents a crucial treatment component that affects multiple outcome domains. Sleep hygiene education covers maintaining consistent sleep-wake schedules, creating optimal sleep environments that are dark, quiet, and cool, limiting screen time before bed, avoiding caffeine and alcohol, and using relaxation techniques. Treatment of specific sleep disorders may include continuous positive airway pressure for sleep apnea, repositioning techniques for positional sleep disorders, or medications when appropriate. Improving sleep quality enhances cognitive function, mood, pain management, and overall recovery (Sleep Disorders After Brain Injury, 2025).practicalneurology
- Pain management employs multiple modalities to address headaches, neck pain, and other pain complaints. Non-pharmacological approaches include manual therapy, therapeutic exercise, heat or cold application, relaxation techniques, and biofeedback. Pharmacological options when needed include appropriate analgesics, muscle relaxants, or nerve pain medications, used cautiously to avoid medication overuse and unwanted side effects. The goal emphasizes restoring function and reducing pain interference rather than complete pain elimination, which may not be achievable (Pain and Traumatic Brain Injury, 2024).health
- Mood and emotional support acknowledges the profound psychological impacts of brain injury and chronic symptoms. Interventions include supportive counseling addressing adjustment to injury and life changes, cognitive-behavioral therapy to modify unhelpful thought patterns and behaviors, stress management techniques, mindfulness and relaxation training, support groups connecting individuals with others facing similar challenges, and psychiatric medications when appropriate. Family involvement and education play a crucial role in creating a supportive home environment that fosters recovery from mood disorders following traumatic brain injury (TBI) (Mood Disorders Following TBI, 2025).practicalneurology
- Coordination across providers ensures comprehensive, efficient care. Regular communication between chiropractors, nurse practitioners, physical therapists, occupational therapists, speech-language pathologists, neuropsychologists, and other specialists involved in care promotes integrated treatment planning. Case conferences discuss patient progress, treatment responses, and plan modifications. This team approach prevents fragmented care and ensures all providers work toward shared goals. Dr. Alexander Jimenez’s practice exemplifies this coordination by offering multiple services within an integrated setting while maintaining referral relationships with specialists for needs beyond the clinic’s scope (Dr. Alex Jimenez’s Integrative Practice, n.d.).missionlegalcenter
Progress monitoring uses both objective measures and subjective reports to assess treatment effectiveness. Standardized outcome measures track symptom severity, functional abilities, and quality of life over time. Regular reassessments identify improvements, plateaus, or declines that necessitate adjustments to treatment. Flexible treatment plans adapt to changing needs as recovery progresses, with some interventions becoming less necessary as function improves, while others may need to be added or intensified. This responsive approach ensures that treatment remains appropriate throughout the recovery trajectory.
Conclusion
Through disturbed neuronal regulation, inflammatory processes, hormonal imbalances, and metabolic alterations, traumatic brain injury is a complicated medical disorder that affects not just the brain but the whole body. One of the most significant effects is cognitive impairment, which affects executive function, processing speed, memory, attention, and other mental skills essential for independent living. Autonomic dysfunction and systemic inflammatory reactions affect essential organs, whereas spasticity, weakness, coordination issues, and balance deficiencies affect the musculoskeletal system. Comprehensive treatment for traumatic brain injury requires an understanding of the brain-body link. Injury disrupts the complex communication networks that connect the brain to muscles, bones, organs, and metabolic systems, resulting in far-reaching impacts that necessitate a variety of therapeutic modalities. Healthcare professionals can identify the complete range of injury-related issues, including cognitive impairments that patients may not voluntarily mention and musculoskeletal or systemic symptoms that have a substantial impact on recovery, by obtaining a thorough history and asking methodical questions.
The multifaceted character of traumatic brain injury rehabilitation is addressed by an integrated strategy that combines chiropractic treatment with nurse practitioner supervision. Through soft tissue treatments, spinal adjustments, and rehabilitative activities that enhance biomechanics, lessen pain, and promote neuroplasticity, chiropractic interventions restore nervous system function. Nurse practitioners provide comprehensive care, including mood management, dietary counseling, medical supervision, cognitive support, and complete care coordination. Dr. Alexander Jimenez’s dual-scope practice exemplifies how this teamwork yields comprehensive treatment regimens that address the mental, emotional, physical, and metabolic aspects of recovery. Holistic treatment regimens include multiple therapy modalities that are customized to each patient’s specific needs and modified in response to those needs. While targeting specific symptoms and functional constraints, these programs recognize that promoting the body’s natural healing processes is crucial to a successful recovery. To promote healing and restore function, various therapies work in concert, including spinal care, soft tissue work, exercise therapy, nutritional assistance, cognitive rehabilitation, sleep optimization, pain management, and emotional support. Throughout the rehabilitation process, interventions are tailored to individual progress via progress tracking and therapeutic adaptability. Depending on a variety of circumstances, including age, location, severity of the damage, and pre-accident health, each person’s road to recovery from traumatic brain injury is unique. Some individuals heal very quickly and completely, while others have long-term functional impairments and lingering symptoms. By treating the whole person rather than just specific symptoms and by promoting the brain’s extraordinary ability to adapt and recover, an integrated, holistic approach gives promise for better results. Recovery prospects for those dealing with traumatic brain injury are expected to be substantially enhanced by ongoing research, better diagnostic instruments, and improved treatment modalities.
References
- Abdullah, N., et al. (2022). Nutrition Management in Patients With Traumatic Brain Injury. https://pmc.ncbi.nlm.nih.gov/articles/PMC9833460/
- Anatomy and physiology of the nervous system. (2020, January 28). Canadian Cancer Society. https://cancer.ca/en/cancer-information/cancer-types/neuroblastoma/what-is-neuroblastoma/the-nervous-system
- Anxiety and Depression Following TBI. (2023, April 3). Connectivity – Traumatic Brain Injury. https://www.connectivity.org.au/symptoms-and-care/tbi-symptoms-explained/anxiety-and-depression-following-tbi/
- Bailes, J. E., & Borlongan, C. V. (2020). Traumatic brain injury. CNS Neuroscience & Therapeutics, 26(6), 593-594. https://pmc.ncbi.nlm.nih.gov/articles/PMC7248541/
- Bonsack, B., et al. (2020). Mesenchymal stem cell therapy alleviates the neuroinflammation associated with acquired brain injury. CNS Neuroscience & Therapeutics, 26(6), 603-615. https://pmc.ncbi.nlm.nih.gov/articles/PMC7248541/
- Central nervous system (CNS) – function, disorders. (2025, September 3). Healthdirect. https://www.healthdirect.gov.au/central-nervous-system
- Chiropractic Care Supports Healing After TBI. (2009, March 19). Pinnacle Health Chiropractic. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi
- Chiropractic Neurology Supports Brain Healing. (2025, July 23). HML Functional Care. https://hmlfunctionalcare.com/how-chiropractic-neurology-supports-brain-healing/
- Cognitive Impairment Following Traumatic Brain Injury. (2002, January 21). PubMed. https://pubmed.ncbi.nlm.nih.gov/11734103/
- Cognitive Problems After Traumatic Brain Injury. (n.d.). MSKTC. https://uwmsktc.washington.edu/sites/uwmsktc/files/files/TBI_cognitive.pdf
- Collins, M. E., & Misukanis, T. M. (2004). Chiropractic Management of a Patient with Post-Traumatic Vertigo of Complex Origin. Journal of Chiropractic Medicine, 4(4), 32-38. https://pmc.ncbi.nlm.nih.gov/articles/PMC2647031/
- Criteria used to classify TBI severity. (2012, June 23). NCBI – NIH. https://www.ncbi.nlm.nih.gov/books/NBK98986/table/introduction.t1/
- Dr. Alex Jimenez’s Integrative Practice. (n.d.). Dr. Alex Jimenez. https://dralexjimenez.com/
- Figueiredo, T. H., et al. (2024). An integrative, holistic treatment approach for veterans with chronic traumatic brain injury and associated comorbidities: case report. Frontiers in Neurology. https://pmc.ncbi.nlm.nih.gov/articles/PMC12081389/
- 4 Types of Brain Injuries and 3 Levels of Severity. (2021, December 9). Mission Personal Injury Lawyers. https://missionlegalcenter.com/blog/4-types-of-brain-injuries-and-3-levels-of-severity/
- Grima, N., et al. (2016). Sleep disturbances in traumatic brain injury: a meta-analysis. Journal of Clinical Sleep Medicine, 12(3), 419-428. https://jcsm.aasm.org/doi/10.5664/jcsm.5598
- Hidden TBI Symptoms: Integrative Model. (2025, September 30). El Paso Chiropractor Blog. https://www.elpasochiropractorblog.com/2025/10/hidden-tbi-symptoms-integrative.html
- Hoffman, J. M., et al. (2024). Collaborative care for TBI pain. National Academies Forum on TBI. https://www.cognitivefxusa.com/blog/traumatic-brain-injury-long-term-effects-and-treatment
- Kanayama, G., et al. (2019). Increase in cerebral blood flow indicated by increased cerebral arterial area and pixel intensity on brain magnetic resonance angiogram following correction of cervical lordosis. Brain Circulation, 5(1), 19-26. https://pmc.ncbi.nlm.nih.gov/articles/PMC6458772/
- Kenney, K., et al. (2018). Long-term Consequences of Traumatic Brain Injury in Bone Metabolism. Frontiers in Neurology, 9, 115. https://pmc.ncbi.nlm.nih.gov/articles/PMC5845384/
- Mind-body connection is built into the brain, study suggests. (2023, April 19). Washington University School of Medicine. https://medicine.washu.edu/news/mind-body-connection-is-built-into-brain-study-suggests/
- Mood Disorders Following Traumatic Brain Injury. (2025, October 28). Practical Neurology. https://practicalneurology.com/diseases-diagnoses/tbi/mood-disorders-following-traumatic-brain-injury/31994/
- Multiorgan Dysfunction After Severe Traumatic Brain Injury. (2021, January 15). Chest Journal. https://pmc.ncbi.nlm.nih.gov/articles/PMC8448997/
- Neuroendocrine Disturbances Following Traumatic Brain Injury. (2023, January 4). Brain Injury Association of America. https://biausa.org/public-affairs/media/neuroendocrine-disturbances-following-tbi
- Nervous System: What It Is, Parts, Function & Disorders. (2024, December 18). Cleveland Clinic. https://my.clevelandclinic.org/health/body/21202-nervous-system
- Nutritional interventions to support acute mTBI recovery. (2022, October 13). Frontiers in Nutrition. https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.977728/fullhttps://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.977728/full
- Oyesanya, T. O., & Thomas, M. A. (2019). Strategies Nurses Use when Caring for Patients with Moderate-to-Severe Traumatic Brain Injury who have Cognitive Impairments. Journal of Clinical Nursing, 28(23-24), 4277-4289. https://pmc.ncbi.nlm.nih.gov/articles/PMC6800766/
- Pain and Traumatic Brain Injury. (2024, August 28). Health.mil. https://health.mil/Reference-Center/Publications/2024/08/29/TBICoE-Research-Review-Pain-and-TBI
- Physical effects of brain injury. (n.d.). Headway. https://www.headway.org.uk/about-brain-injury/individuals/effects-of-brain-injury/physical-effects-of-brain-injury/
- Revealing Communications Between Brain and Body. (2022, March 15). Yale Medicine. https://medicine.yale.edu/news-article/revealing-communications-between-brain-and-body/
- Sleep Disorders After Brain Injury. (2025, October 27). Practical Neurology. https://practicalneurology.com/diseases-diagnoses/sleep/sleep–traumatic-brain-injury/30113/
- Stovell, M. G., et al. (2019). Impact of traumatic brain injury on sleep: an overview. Journal of Clinical Sleep Medicine, 15(8), 1287-1295. https://pmc.ncbi.nlm.nih.gov/articles/PMC6707934/
- Survey of chiropractic clinicians on MTBI. (2018, June 13). Chiropractic & Manual Therapies. https://pmc.ncbi.nlm.nih.gov/articles/PMC6000952/
- TBI-Induced Spasticity. (2015, May 17). NCBI – NIH. https://www.ncbi.nlm.nih.gov/books/NBK299194/
- Therapeutic Interventions for Traumatic Brain Injury. (2024). Physiopedia. https://www.physio-pedia.com/Therapeutic_Interventions_for_Traumatic_Brain_Injury
- Traumatic Brain Injury. (2023, December 31). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi
- Traumatic brain injury and mood disorders. (2020, November 4). Psychopharmacology Bulletin, 50(4 Suppl 1), 131-146. https://pmc.ncbi.nlm.nih.gov/articles/PMC7653730/
- Traumatic brain injury from a peripheral axis perspective. (2025, September 12). ScienceDirect. https://www.sciencedirect.com/science/article/pii/S0301008225000243
- Types of Traumatic Brain Injury. (2024, March 14). UCLA Research Spotlight. https://medschool.ucla.edu/news-article/types-of-traumatic-brain-injury
- Vestibular dysfunction in acute traumatic brain injury. (2019, June 13). Brain Injury, 33(9), 1117-1121. https://pmc.ncbi.nlm.nih.gov/articles/PMC6765474/
- Willing, A. E., et al. (2020). Potential of mesenchymal stem cells alone, or in combination, to treat traumatic brain injury. CNS Neuroscience & Therapeutics, 26(6), 616-627. https://pmc.ncbi.nlm.nih.gov/articles/PMC7248541/