Peroneal Tendon Injuries and Their Symptoms
Are individuals with high foot arches or participating in sports involving repetitive ankle motion at risk for developing peroneal tendon injuries?
Peroneal Tendon Injuries
The peroneal tendons connect the muscles of the outer side of the lower leg to the foot. They may be acute—occurring suddenly—or chronic—developing over time. The basic types of peroneal tendon injuries are tendonitis, tears, and subluxation.
Anatomy and Function
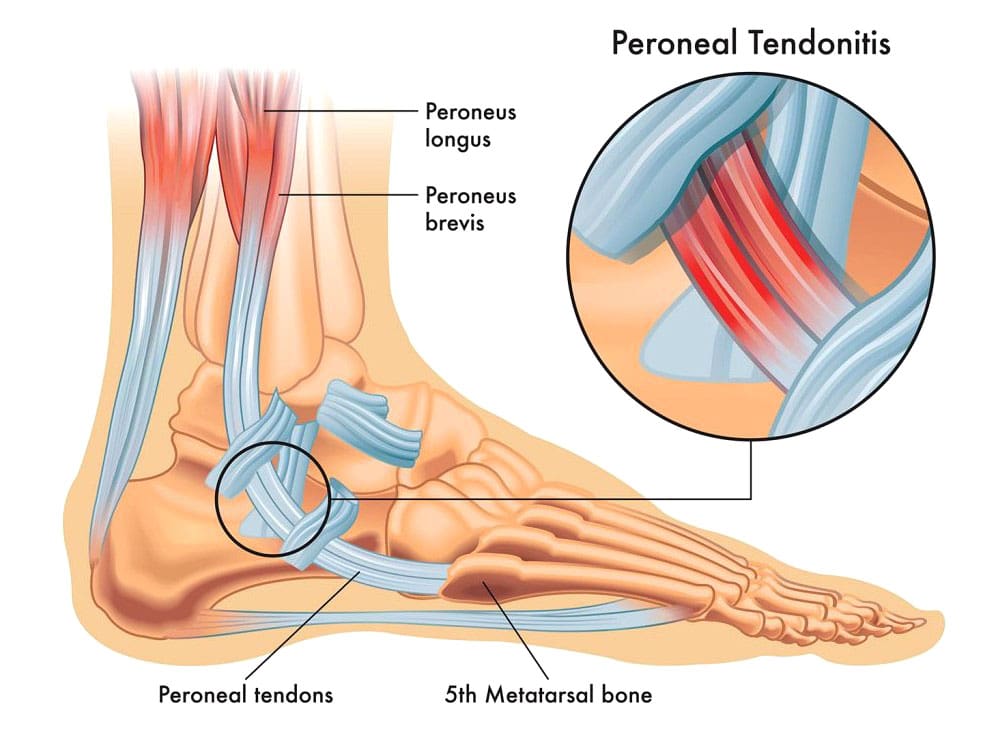
The two major peroneal muscles (peroneus longus and peroneus brevis) are outside the lower leg, next to the calf muscles. The peroneal tendons run along the outer side of the ankle and attach to the foot, connecting these muscles to bone. They help stabilize the ankle joint, point the foot downward (plantarflexion), and turn the foot outward (eversion). In normal gait, the motion of the peroneal muscles is balanced by the muscles that invert the foot or rock the foot inward from the ankle. The two peroneal tendons sit one on top of the other right behind the fibula (the smaller lower leg bone). This closeness can contribute to problems with the peroneal tendons, as they rub together behind the ankle.
Tendonitis
The most common problem is inflammation or tendonitis. The tendons are usually inflamed just behind the fibula bone at the ankle joint. This part of the fibula is the bump on the outside of the ankle, and the peroneal tendons are located just behind that bony prominence. Tendonitis can either result from repetitive overuse or an acute injury. Common symptoms of tendonitis include:
- Pain behind the ankle
- Swelling over the peroneal tendons
- Tenderness of the tendons
- Pain usually worsens if the foot is pulled down and inwards, stretching the peroneal tendons.
- X-rays of the ankle are taken.
- MRI may show inflammation and fluid around the tendons. (Walt J. & Massey P. 2023)
Typical treatment of peroneal tendonitis is accomplished by:
Ice application
- Applying ice to the area can help reduce swelling and control pain.
Rest
- Resting is important to allow the tendon to heal.
- A supportive device (walking boot or ankle brace) or crutches can help in severe cases.
- Braces and boots provide support, reduce tendons’ stress, and allow rest and inflammation to subside.
Anti-inflammatory Medications
- Motrin or Aleve are anti-inflammatory and can reduce the swelling around the tendon.
Physical Therapy
- Physical therapy can help restore normal ankle joint mechanics, help with swelling and pain relief, and correct strength imbalances.
Cortisone Injections
- Cortisone injections are low-risk if administered to the area around the tendon and not more often than every three months.
- Ultrasound guidance can help ensure the medication is injected into the correct area. (Walt J. & Massey P. 2023)
Tendon Tears
Tears can occur and are more likely to happen in the peroneus brevis tendon. Tears are believed to be the result of two issues with the tendon. One is the blood supply. Tears of the peroneus brevis tendon almost always occur in the area where the blood supply and nutrition of the tendon are the poorest.
The second issue is the closeness between the two tendons, causing the peroneus brevis tendon to be wedged between the peroneus longus tendon and the bone. (Saxena A., & Bareither D. 2001) Tears of the peroneus brevis tendon are often treated with the same treatments for tendonitis. About half of the tears diagnosed by imaging are found to be asymptomatic. For individuals who don’t find lasting relief from symptoms, surgery may be necessary. Surgical options for peroneal tendon tears (Dombek M. F. et al., 2001)
Tendon Debridement and Repair
- During a tendon debridement, the damaged tendon and the surrounding inflammatory tissue are removed.
- The tear can be repaired, and the tendon can be tubularized to restore its normal shape.
Tenodesis
- A tenodesis is a procedure where the damaged area of the tendon is sewn to the normal tendon.
- In this case, the damaged segment of the peroneal tendon is removed, and the ends left behind are sewn to the adjacent remaining peroneal tendon.
- Tenodesis is often recommended for tears involving more than 50% of the tendon. (Castilho R. S. et al., 2024)
Depending on the surgical procedure, Recovery after surgery can take several weeks of restricted weight-bearing and immobilization. Following immobilization, therapy can begin. Recovery is usually six to 12 weeks, depending on the surgery, but a full return to sports and activities may take several months. Risks of surgery include infection, stiffness, skin numbness near the incision, persistent swelling, and persistent pain.
Injury Medical Chiropractic and Functional Medicine Clinic
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems.
The Difference of Using Custom Foot Orthotics
References
Walt, J., & Massey, P. (2025). Peroneal Tendon Syndromes. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/31335074
Saxena, A., & Bareither, D. (2001). Magnetic resonance and cadaveric findings of the “watershed band” of the Achilles tendon. The Journal of foot and ankle surgery: official publication of the American College of Foot and Ankle Surgeons, 40(3), 132–136. https://doi.org/10.1016/s1067-2516(01)80078-8
Dombek, M. F., Orsini, R., Mendicino, R. W., & Saltrick, K. (2001). Peroneus brevis tendon tears. Clinics in podiatric medicine and surgery, 18(3), 409–427.
Castilho, R. S., Magalhães, J. M. B., Veríssimo, B. P. M., Perisano, C., Greco, T., & Zambelli, R. (2024). Minimally Invasive Peroneal Tenodesis Assisted by Peroneal Tendoscopy: Technique and Preliminary Results. Medicina (Kaunas, Lithuania), 60(1), 104. https://doi.org/10.3390/medicina60010104





















