Chiropractic Care Approaches for The Gut-Liver Connection
Uncover the benefits of understanding the gut-liver connection with chiropractic care and its role in holistic health for individuals.
Restoring Balance Through the Gut-Liver Axis: Chiropractic and Integrative Approaches for Pain Relief and Optimal Health
Chronic pain, digestive issues, or persistent fatigue can significantly hinder daily life, often signaling deeper imbalances within the body. The gut-liver axis, a critical physiological network, plays a central role in overall health, influencing digestion, inflammation, and musculoskeletal function. This article examines the scientific foundation of how the gut supports essential bodily processes, the impact of environmental factors on this balance, and how these disruptions lead to overlapping symptoms affecting digestion, muscles, and joints. We’ll provide a clinical rationale for the role of chiropractic care in addressing this axis, complemented by nonsurgical interventions such as targeted exercises, massage, acupuncture, and integrative medicine, which prioritize natural healing and patient education over physical strength alone.
Written for clarity and grounded in peer-reviewed research, this guide draws on insights from Dr. Alexander Jimenez, a functional medicine expert, to offer evidence-based strategies for holistic wellness and pain management. Always consult a healthcare professional for personalized guidance.
The Gut-Liver Axis: A Foundation for Health and Recovery
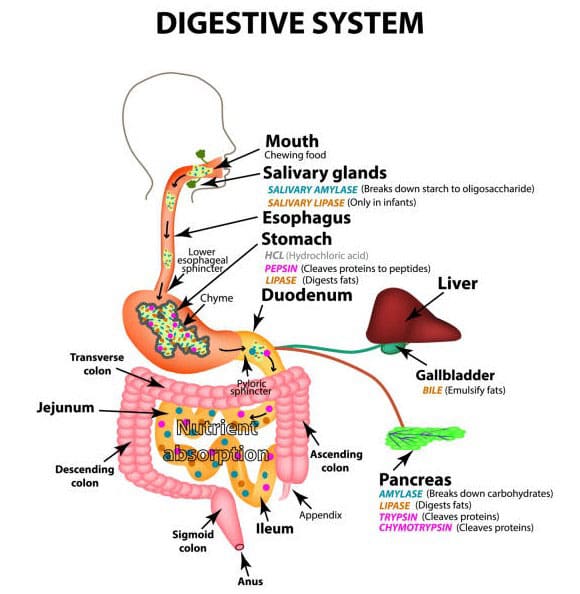
The gut-liver axis is a bidirectional communication system linking the intestines and liver through the portal vein, which transports nutrients, microbial metabolites, and toxins from the gut to the liver for processing. The liver reciprocates by producing bile acids to aid fat digestion and regulate gut microbiota, ensuring efficient nutrient absorption and detoxification. This synergy supports energy production, immune function, and tissue repair, all of which are critical for maintaining musculoskeletal health.
Disruptions in this axis can trigger systemic inflammation, exacerbating pain or mobility issues. For instance, gut dysbiosis may increase endotoxins, such as lipopolysaccharides (LPS), which induce hepatic inflammation that amplifies musculoskeletal pain through the release of cytokines (Wang et al., 2021). Functional medicine clinicians, such as Dr. Jimenez, utilize advanced diagnostics, including microbiome analysis and liver function tests, to assess this axis. They design nonsurgical interventions to restore balance and alleviate symptoms (Jimenez, n.d.).
The Gut’s Pivotal Role in Body Function and Pain Relief
The gastrointestinal system is a cornerstone of health, orchestrating the absorption of nutrients, regulating the immune system, and facilitating neural signaling. Its microbiome—comprising over 100 trillion microorganisms—metabolizes dietary fibers into short-chain fatty acids (SCFAs), such as butyrate, which nourish intestinal cells and reduce systemic inflammation. Hosting approximately 70% of the body’s immune cells, the gut defends against pathogens while maintaining microbial balance, which is critical for preventing chronic inflammation.
Through the gut-brain axis, mediated by the vagus nerve, the gut influences pain perception and stress responses, which can exacerbate musculoskeletal conditions like back or joint pain. Dysbiosis disrupts this balance, increasing intestinal permeability and systemic inflammation, which can potentially manifest as somatic pain through viscerosomatic reflexes (Farmer et al., 2009). Dr. Jimenez integrates nutritional interventions and microbiome testing, noting that patients with optimized gut health often report reduced pain and improved mobility (Jimenez, n.d.).
The Gut-Liver Connection: Mechanisms of Interdependence
The gut and liver are intricately linked through enterohepatic circulation. The portal vein delivers 70% of the liver’s blood supply, carrying gut-derived substances for metabolism or detoxification. Bile acids, synthesized by the liver, are secreted into the gut to emulsify fats and modulate microbial populations, preventing pathogenic overgrowth.
Research indicates that gut dysbiosis alters bile acid profiles, leading to the increased production of secondary bile acids that induce hepatic inflammation, as observed in non-alcoholic fatty liver disease (NAFLD) (Federico et al., 2017). Alcohol consumption exacerbates this by compromising tight junctions, leading to endotoxemia and liver damage, which can heighten systemic pain (Chae et al., 2024). Dr. Jimenez applies this evidence, utilizing biomarkers such as zonulin to assess gut permeability and tailor interventions that support both organs, thereby reducing pain and inflammation (Wellness Doctor RX, n.d.).
Environmental Factors: Disrupting Balance and Triggering Symptoms
Environmental stressors profoundly impact the gut-liver axis, often leading to symptoms that overlap with musculoskeletal complaints. Diets high in processed sugars or fats alter microbiota composition, leading to increased LPS production and intestinal permeability, which triggers systemic inflammation that can manifest as joint or muscle pain (Di Vincenzo et al., 2023). Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, altering gut motility and barrier function, which may refer pain to somatic regions (Konturek et al., 2011).
Xenobiotics, such as antibiotics and pollutants, deplete beneficial microbes, thereby fostering dysbiosis. Alcohol, on the other hand, strains both the gut and liver, exacerbating inflammation (Nicholson et al., 2012). These imbalances can lead to visceral pain hypersensitivity, where gut inflammation amplifies somatic pain, mimicking conditions such as chronic back pain (Zia et al., 2022). Dr. Jimenez uses environmental exposure assessments to identify triggers, creating targeted plans to restore gut health and alleviate pain.
Table: Environmental Factors and Their Impact on the Gut-Liver Axis
| Factor | Mechanism of Disruption | Overlapping Symptoms and Pathways |
|---|---|---|
| High-Sugar/Fat Diets | Increases LPS, reduces SCFA production | Systemic inflammation, joint/muscle pain |
| Chronic Stress | HPA axis activation, barrier dysfunction | Referred pain, muscle tension via neural pathways |
| Alcohol/Toxins | Disrupts tight junctions, dysbiosis | Hepatic stress, fatigue, myalgia |
| Antibiotics/Infections | Depletes beneficial bacteria | Chronic inflammation, immune dysregulation |
| Pollutants | Alters microbial metabolism | Fatigue, heightened pain sensitivity |
This table synthesizes mechanistic data to guide evidence-based interventions.
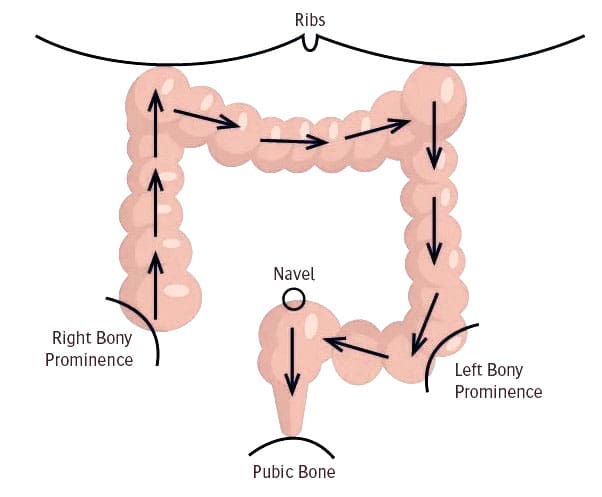
Clinical Rationale: Chiropractic Care’s Role in the Gut-Liver Axis
Chiropractic care, grounded in neurophysiology, addresses the gut-liver axis by optimizing the function of the autonomic nervous system (ANS). Spinal misalignments (subluxations) in the thoracic and lumbar regions can disrupt sympathetic innervation to the gut and liver, impairing motility and detoxification. Clinical studies suggest spinal manipulation reduces visceral hypersensitivity by modulating somato-autonomic reflexes, decreasing inflammatory cytokines that exacerbate pain (Elsenbruch et al., 2015).
Probiotics, often used in conjunction with chiropractic care, help restore microbial balance, thereby reducing liver stress and systemic inflammation (Hojsak, 2024). Dr. Jimenez integrates spinal adjustments with gut-liver biomarkers, noting that patients with chronic pain or mobility issues experience significant relief when inflammation is addressed holistically, emphasizing neural optimization over physical force (Jimenez, n.d.).
The Healing Diet: Combat Inflammation, Embrace Wellness: Video
Nonsurgical Interventions: Evidence-Based Strategies for Healing
Nonsurgical approaches target the gut-liver axis to promote healing and pain relief. Anti-inflammatory diets, rich in fiber, omega-3 fatty acids, and probiotics, help repair the gut lining and support liver detoxification, thereby reducing systemic inflammation. Targeted exercises, such as lumbar stabilization or yoga, enhance spinal alignment and visceral function, thereby mitigating inflammation according to biomechanical research.
Massage therapy promotes lymphatic drainage, easing hepatic congestion, while acupuncture stimulates vagal pathways, reducing inflammatory markers. Integrative medicine incorporates nutraceuticals like probiotics and curcumin to prevent chronic conditions like arthritis or NAFLD. Dr. Jimenez’s protocols combine these with patient education, ensuring adherence to achieve sustained pain relief and improved mobility.
Insights from Dr. Alexander Jimenez: Advancing Chiropractic Care
Dr. Alexander Jimenez, DC, APRN, FNP-BC, blends chiropractic expertise with functional medicine to address pain and wellness holistically. His evidence-based approach uses microbiome and liver function tests to inform interventions, targeting viscerosomatic pain patterns where gut-liver issues manifest musculoskeletally. Clinical data show reduced inflammatory markers post-adjustment, with patients reporting enhanced mobility and vitality due to his clear, empathetic communication (Jimenez, n.d.).
Practical Steps for Gut-Liver Health and Pain Relief
Begin with diagnostic assessments (e.g., microbiome analysis), adopt anti-inflammatory diets, and incorporate regular chiropractic care and stress management. Monitor biomarkers, such as liver enzymes, for sustained results.
This guide highlights the role of the gut-liver axis in pain management, advocating for chiropractic and integrative care for holistic relief.
References
- Chae, Y.-R., et al. (2024). Diet-Induced Gut Dysbiosis and Leaky Gut Syndrome. Journal of Microbiology and Biotechnology, 34(4), 747-756. https://pubmed.ncbi.nlm.nih.gov/38321650/
- Di Vincenzo, F., et al. (2023). Gut microbiota, intestinal permeability, and systemic inflammation: a narrative review. Internal and Emergency Medicine, 19(2), 275-293. https://pubmed.ncbi.nlm.nih.gov/37505311/
- Elsenbruch, S., et al. (2015). [Visceral pain]. Schmerz, 29(5), 496-502. https://pubmed.ncbi.nlm.nih.gov/26271911/
- Farmer, A. D., et al. (2009). Visceral pain hypersensitivity in functional gastrointestinal disorders. British Medical Bulletin, 91, 123-136. https://pubmed.ncbi.nlm.nih.gov/19620136/
- Federico, A., et al. (2017). Gut microbiota and the liver. Minerva Gastroenterologica e Dietologica, 63(4), 385-398. https://pubmed.ncbi.nlm.nih.gov/28927250/
- Hojsak, I. (2024). Probiotics in Functional Gastrointestinal Disorders. Advances in Experimental Medicine and Biology, 1449, 157-174. https://pubmed.ncbi.nlm.nih.gov/39060737/
- Jimenez, A. (n.d.). Injury Specialists. https://dralexjimenez.com/
- Jimenez, A. (n.d.). LinkedIn Profile. https://www.linkedin.com/in/dralexjimenez/
- Konturek, P. C., et al. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. Journal of Physiology and Pharmacology, 62(6), 591-599. https://pubmed.ncbi.nlm.nih.gov/22314561/
- Nicholson, J. K., et al. (2012). Host-gut microbiota metabolic interactions. Science, 336(6086), 1262-1267. https://pubmed.ncbi.nlm.nih.gov/22674330/
- Wang, R., et al. (2021). Gut microbiome, liver immunology, and liver diseases. Cellular & Molecular Immunology, 18(1), 4-17. https://pubmed.ncbi.nlm.nih.gov/33318628/
- Wellness Doctor RX. (n.d.). The Gut-Liver Connection. https://wellnessdoctorrx.com/the-gut-liver-connection/
- Zia, J. K., et al. (2022). Risk Factors for Abdominal Pain-Related Disorders of Gut-Brain Interaction in Adults and Children: A Systematic Review. Gastroenterology, 163(4), 995-1023.e3. https://pubmed.ncbi.nlm.nih.gov/35716771/