Cellular Health and Fascia Wellness From Systemic Inflammation
Understand the importance of cellular health and fascia in managing systemic inflammation. Enhance your wellness journey today.
By Dr. Alex Jimenez, DC, FNP-APRN
Introduction: Charting the Course for a Longer, Healthier Life
Welcome to this in-depth exploration of the new frontier in longevity and cellular health. As a practitioner dedicated to both the structural and systemic aspects of human wellness, holding credentials as a Doctor of Chiropractic (DC) and a Family Nurse Practitioner (FNP-APRN), I have always been driven by a singular mission: to integrate the most advanced, evidence-based research into practical, effective clinical strategies. This post is the culmination of that mission, designed to distill complex, cutting-edge science into a clear, actionable framework for health. We are moving beyond the traditional, fragmented view of the body and embracing a holistic, interconnected systems-based approach. We will not be talking in hypotheticals; instead, we will present the latest findings from leading researchers in the field, showcasing their work through modern, evidence-based research methods to illuminate the path toward a longer, more vibrant life.
In the sections that follow, we will embark on a comprehensive journey into the very fabric of our being. We will begin by demystifying the concept of aging itself, reframing it not as an inevitable decline but as a modifiable process rooted in what modern science calls the “Hallmarks of Aging.” A central theme will be the concept of “inflammaging,” the chronic, low-grade inflammation that silently accelerates the aging process and underlies nearly every chronic disease. We will discuss why establishing a baseline of your unique biological data from a young age is no longer a luxury but a necessity for predictive and personalized medicine.
From there, our exploration will dive deep into the fascinating world of the fascial system—the body’s ubiquitous connective tissue network. Once dismissed as mere “packing material,” fascia is now recognized as a primary sensory and communication organ, a “body-wide web” that influences everything from our posture and movement to our immune function and cellular health. We will unpack the intricate physiology of fascia, its relationship with the extracellular matrix (ECM), and the pivotal role of its health in optimal cellular signaling, nutrient exchange, and waste removal. You will learn how the fascial system can become dense and fibrotic due to injury, stress, and inflammation, creating a “cellular prison” that perpetuates dysfunction and pain.
A significant portion of our discussion will focus on the immune system’s intimate relationship with the fascial network and the ECM. We will examine how immune cells, such as macrophages, lymphocytes, and mast cells, reside within and are influenced by this matrix. We will explore the Cell Danger Response (CDR), a universal metabolic response to threat, and how a persistent CDR can lead to chronic inflammation and a breakdown in immune tolerance, setting the stage for autoimmune conditions and accelerated aging. This will lead us to a critical analysis of modern metabolic health, particularly the hidden dangers of hyperinsulinemia and its devastating impact on cellular function, even in individuals with “normal” blood sugar. We’ll present a compelling case for why measuring fasting insulin alongside glucose is a non-negotiable aspect of any true health assessment.
Finally, we will translate this deep physiological understanding into practical, evidence-based interventions. We will critically evaluate therapies such as cryotherapy (cold treatment) and thermotherapy (heat therapy), moving beyond simplistic advice to provide nuanced guidelines for their proper application in acute injury versus chronic remodeling. We will also touch on the powerful potential of targeted interventions such as peptides (e.g., BPC-157) and photobiomodulation (red light therapy) to support tissue repair, modulate the immune system, and restore cellular homeostasis. Throughout this post, my goal is to empower you with knowledge—to help you understand the why behind the what, so you can become a more informed and active participant in your own health journey. This is not about chasing fads; it is about building a foundation of resilient health based on the profound and elegant principles of human physiology.
Redefining Aging: From Inevitability to a Modifiable Process
For centuries, we’ve viewed aging as a one-way street of inevitable decline. However, a seismic shift is occurring in medical science. We are beginning to understand aging not merely as the passage of time, but as a specific, definable biological process characterized by a collection of interconnected dysfunctions known as the “Hallmarks of Aging.” This perspective is revolutionary because it reframes aging as a condition that can be studied, understood, and, most importantly, modified.
The conversation has moved from “how long we live” to “how well we live” for the duration of our lives—our healthspan. The goal is no longer to add years to life, but to add life to our years. This involves actively working to re-function, regenerate, and create resilience within our own biology.
The Critical Importance of a Biological Baseline
One of the most foundational principles of this new paradigm is establishing a biological baseline. Imagine trying to navigate a complex journey without a map or a starting point. That’s precisely what we do when we wait for a disease to manifest before taking a deep look at our health.
When I work with patients, whether they are young children or their aging parents, the first and most crucial step is to capture a comprehensive snapshot of their current physiological state. This isn’t just a standard physical; it’s a deep dive into their molecular and cellular world. This baseline becomes our immutable point of reference.
For example, if a patient comes to me today, in 2024, and we run a comprehensive panel of biomarkers, that data is locked in. If they return in 2026 after experiencing a health challenge or simply as part of a proactive monitoring plan, we don’t have to guess what “normal” looks like for them. We can compare their new results directly to their unique baseline. This allows us to detect subtle shifts and deviations long before they snowball into a full-blown clinical diagnosis. It’s the essence of predictive and preventative medicine.
Ideally, this process should begin in youth. By understanding an individual’s genetic predispositions and establishing their unique physiological “signature” early on, we create a roadmap for a lifetime of personalized health optimization. This is about being in a constant state of readiness. Like a well-prepared military, we aren’t waiting for a crisis to happen; we are building the resources and intelligence to anticipate and mitigate threats before they escalate.
Aging as an Informational Problem: Senescence and Geriatric Genes
At its core, aging can be viewed as an informational problem. Our DNA is the blueprint, but it’s the epigenome—the layer of chemical tags that tells our genes when to turn on and off—that acts as the software. Over time, due to environmental insults, lifestyle factors, and metabolic dysfunction, this “software” can become corrupted.
This leads to a phenomenon called cellular senescence, where cells lose their ability to divide and function properly. These “zombie cells” don’t just sit there quietly; they secrete a cocktail of inflammatory signals known as the Senescence-Associated Secretory Phenotype (SASP), which poisons the surrounding tissue environment and accelerates the aging of neighboring cells.
This is an informational breakdown. The cell’s internal programming has been disrupted. For example, in an aging liver or ovary, the epigenetic signals can begin to turn on what we might call “geriatric genes”—genes that promote fibrosis, inflammation, and a loss of functional capacity. Our goal is to maintain the integrity of that original, youthful genetic “software” for as long as possible. Understanding a person’s baseline is the first step in monitoring and protecting that precious informational code.
The Fascial System: Your Body’s Intelligent, Interconnected Web
If we are to understand health and longevity truly, we must look beyond individual organs and systems and appreciate the tissue that connects them all: fascia. For too long, fascia was dismissed in anatomy labs as the white, fibrous “stuff” that you had to cut through to get to the “important” structures like muscles and organs. Modern research, however, has unveiled fascia as one of the most vital and intelligent systems in the body.

Think of it as a continuous, body-wide tensional network that exists from head to toe, from skin to bone. It’s not just a series of disconnected sheets; it’s a single, uninterrupted web. This web has three main layers:
- Superficial Fascia: Located just beneath the skin, rich in fat, nerves, and blood vessels.
- Deep Fascia: The dense, fibrous layer that envelops and separates muscles, bones, and organs, forming compartments and transmitting mechanical force.
- Visceral Fascia: The layer that surrounds and suspends our organs within their cavities.
But it goes even deeper. Fascia continues into the structures it surrounds. The connective tissue wrapping a muscle (epimysium), a muscle bundle (perimysium), and even a single muscle fiber (endomysium) are all part of this continuous fascial matrix. It even extends to the covering of our nerves (epineurium, perineurium, endoneurium). It is, in every sense, the fabric that holds us together.
Fascia as a Primary Sensory and Communication Organ
Perhaps the most groundbreaking discovery is that fascia are among our richest sensory organs. It is densely populated with mechanoreceptors—nerve endings that sense pressure, tension, and movement. In fact, it’s estimated that the fascial network contains a staggering number of sensory nerve endings, potentially rivaling or even exceeding that of the retina. Some leading researchers, like Dr. Robert Schleip, posit that up to 80% of our interoceptive information—the sense of our body’s internal state—originates from the sensory nerves embedded in our fascia, not just from our muscles.

This has profound implications. When you feel “stiff,” “tight,” or have a poor sense of your body’s position in space, you are receiving signals from your fascial network. This system is constantly communicating with the central nervous system, providing a real-time feedback loop on our mechanical status, hydration levels, and overall physiological well-being. It is the physical substrate of our mind-body connection. Energy and information travel through this network at incredible speed. While we are roughly 70% water by weight, the molecules that make up our bodies are 99% water molecules. This aqueous, crystalline matrix of the fascia is the perfect medium for conducting bioelectric and mechanical signals.
Fascial Lines and the Transmission of Force
Fascia is not arranged randomly. It organizes itself along lines of tension, creating what pioneers like Tom Myers have termed “Anatomy Trains” or myofascial meridians. These are continuous lines of fascial connection that link different parts of thebody.
A classic example is the Superficial Back Line, which runs from the bottom of your feet, up the calves and hamstrings, over the sacrum, up the erector spinae muscles, and over the top of the skull to your eyebrows. This explains why tension in your feet can contribute to headaches, or why tightness in your hamstrings can cause low back pain.
Another crucial line is the Spiral Line, which loops around the body like a double helix, connecting, for example, the left shoulder to the right hip. This is the line that governs rotational movements, like throwing a ball or walking. An imbalance or restriction anywhere along this line will compromise the efficiency and fluidity of the entire chain. This is why a therapist might work on your hip to resolve a shoulder problem—they are not treating the site of pain, but the source of the dysfunction within the interconnected fascial web. This interconnectedness is the very reason why a holistic approach to the body is not just a philosophy, but a physiological necessity.
The Extracellular Matrix (ECM): The Cellular Neighborhood
To understand how fascia influences health at the most fundamental level, we must zoom in from the macroscopic fascial planes to the microscopic environment surrounding every cell in our body: the Extracellular Matrix (ECM). The ECM is the non-cellular component of all tissues. If the cells are the residents of a neighborhood, the ECM is the entire infrastructure—the roads, communication lines, waste-disposal systems, and public parks.
The ECM is a complex, gel-like substance primarily produced and maintained by cells called fibroblasts. It is composed of a rich “cocktail” of molecules, including:
- Collagen: The primary structural protein, providing tensile strength and stability. There are many types, with Type I being the most abundant and providing rigidity. At the same time, Type III (reticular collagen) is finer and more flexible, often found in new tissue and during the early stages of wound healing.
- Elastin: A protein that allows tissues to stretch and recoil, providing elasticity.
- Proteoglycans and Glycosaminoglycans (GAGs): These are large molecules (like hyaluronic acid) that attract and hold vast amounts of water, creating the hydrated, gel-like consistency of the ECM. This hydration is critical for shock absorption and for facilitating the diffusion of nutrients and signaling molecules.
The ECM is not passive scaffolding. It is a dynamic, biologically active environment in constant, bidirectional communication with the cells living within it. Cells use the ECM to impart strength and shape to tissues, but the ECM, in turn, dictates cell behavior. It provides physical and biochemical cues that influence cell differentiation, migration, proliferation, and survival. Hormones, growth factors, and cytokines all travel through and are modulated by the ECM to reach their target cells.
When the Neighborhood Goes Bad: Fibrosis and the Cell Danger Response
In a healthy state, the ECM is a fluid, adaptable, and resilient environment. However, following injury, chronic inflammation, or metabolic stress, this neighborhood can become a very hostile place.
This is where the Cell Danger Response (CDR) comes into play. The CDR, a concept brilliantly articulated by Dr. Robert Naviaux, is a universal, evolutionarily conserved metabolic response that a cell initiates when it perceives a threat—be it a virus, a toxin, or a physical injury. The cell essentially shifts its priorities from “peacetime” functions (growth, repair, social interaction with other cells) to “wartime” functions (defense). It hunkers down, hardens its membrane, and changes its metabolism.
If this threat is acute and resolved quickly, the cell returns to its normal state. But if the danger is chronic—persistent inflammation, ongoing metabolic stress, unresolved emotional trauma—the CDR can get “stuck” in the “on” position. This has devastating consequences for the ECM.
In a state of chronic CDR, cells like fibroblasts are signaled to go into overdrive. They begin to churn out excessive amounts of collagen, particularly the thick, rigid Type I collagen. They also produce enzymes that cross-link these fibers, making the ECM dense, stiff, and fibrotic. The once-fluid, gel-like matrix becomes more like hardened cement.
This densification and fibrosis of the fascia and ECM create a “cellular prison.”
- Impaired Communication: The stiff matrix physically blocks the flow of signaling molecules, nutrients, and oxygen to the cells.
- Waste Accumulation: Metabolic waste products cannot be efficiently cleared, creating a toxic local environment. This further lowers the local pH, making the tissue more acidic, which in itself is a powerful inflammatory signal.
- Mechanical Entrapment: Nerves and blood vessels become compressed and entrapped within this fibrotic tissue, leading to pain, numbness, and ischemia (lack of blood flow).
- Perpetuating Inflammation: The stiff ECM itself sends pro-inflammatory signals back to the cells, creating a vicious, self-perpetuating cycle of inflammation and fibrosis. This is a key driver of conditions like hyperalgesia (an amplified pain response) and sustained inflammation seen in chronic pain syndromes.
This process is not limited to musculoskeletal injuries. It is the same fundamental pathology we see in a fibrotic liver (cirrhosis), hardened arteries (atherosclerosis), and the tissue damage following chemotherapy or radiation. Understanding how to address and remodel this dysfunctional ECM is a cornerstone of true healing and longevity.
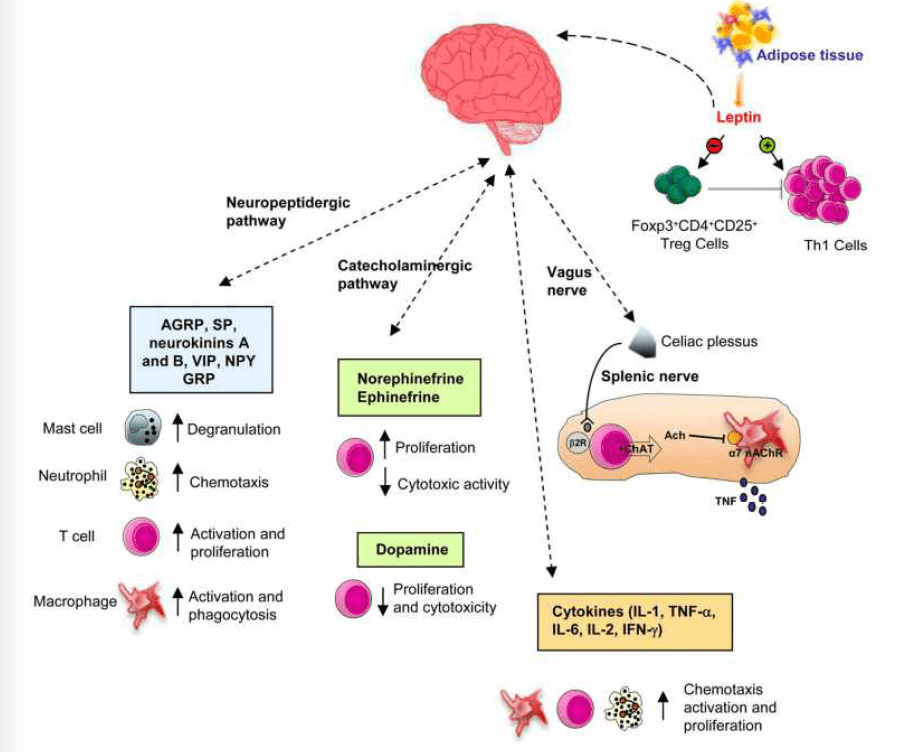
The Immune System’s Role in Fascia and the ECM

The immune system and the fascial/ECM network are inextricably linked. The ECM is not just a passive scaffold; it is a primary residence and playground for a vast array of immune cells. This is where the body’s surveillance and defense operations are headquartered.
Key immune cells that reside within the fascial matrix include:
- Macrophages: the “clean-up crew” of the immune system. They patrol the ECM, engulfing cellular debris, pathogens, and senescent cells. They are also master regulators, capable of shifting their phenotype (behavior) from a pro-inflammatory (M1) state to an anti-inflammatory and pro-repair (M2) state. The state of the ECM heavily influences this shift.
- Mast Cells: These cells are packed with granules containing potent signaling molecules like histamine and cytokines. When they degranulate in response to an injury or allergen, they initiate the inflammatory cascade, increasing blood vessel permeability and recruiting other immune cells to the site.
- Lymphocytes (T cells and B cells): These are the cells of the adaptive immune system. They infiltrate tissues from the bloodstream in response to specific threats, orchestrating targeted attacks and creating immunological memory.
- Dendritic Cells: These are the “scouts” that sample the environment for foreign invaders. They capture antigens and present them to T cells in lymph nodes, thereby initiating a specific immune response.
In a healthy state, these cells work in a beautifully orchestrated symphony. Following an acute injury, they mount a controlled inflammatory response to clear the damage and then transition to a pro-resolving phase to facilitate healing and remodeling of the ECM. This process is called immune tolerance and resolution.
Breaking the Tolerance: From Acute Inflammation to Chronic Disease

The problem arises when this process becomes dysregulated. In the context of a chronically stuck Cell Danger Response and a fibrotic ECM, the immune system’s behavior changes dramatically.
- Vicious Cycle: The stiff, acidic, and hypoxic (low oxygen) ECM sends danger signals that keep macrophages in a pro-inflammatory M1 state. These M1 macrophages, in turn, release cytokines that stimulate fibroblasts to produce even more fibrotic tissue, perpetuating the cycle.
- Loss of Tolerance: The normal resolution process fails. The immune system remains on high alert. T regulatory cells, which are supposed to pump the brakes on the immune response by releasing anti-inflammatory signals such as IL-10, become suppressed or ineffective.
- Auto-reactivity: Chronic inflammation and tissue damage can expose “self-antigens”—proteins normally hidden from the immune system. This can trigger a case of mistaken identity, where the immune system begins to attack the body’s own tissues, leading to autoimmune diseases.
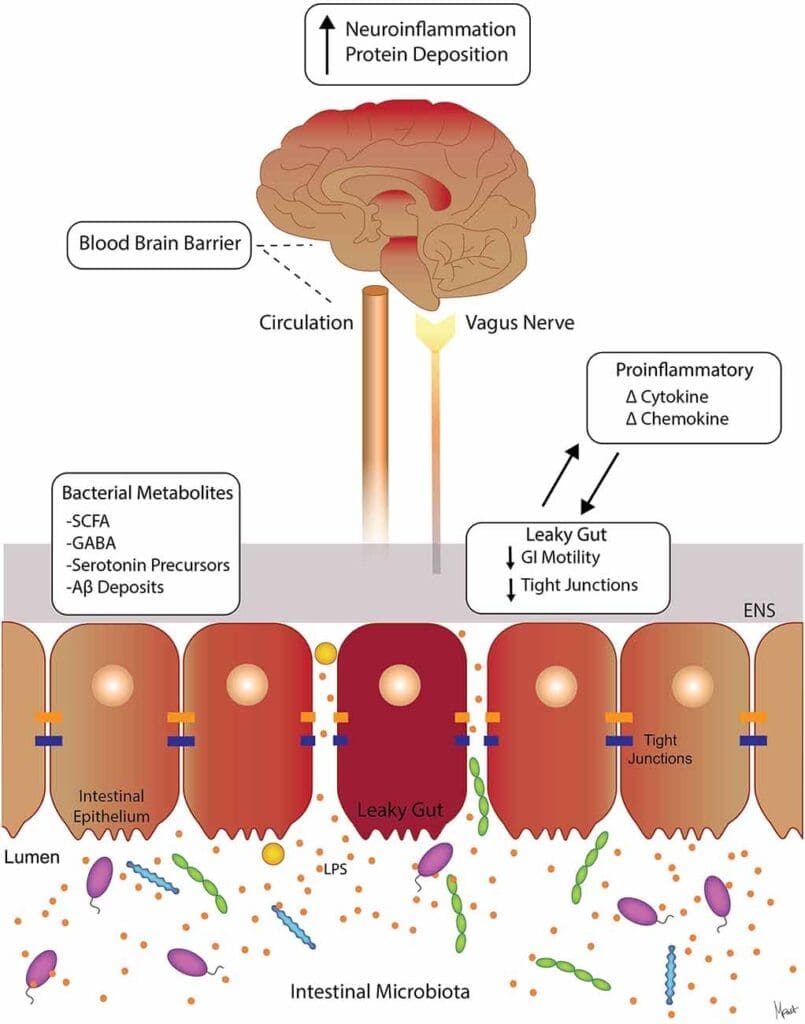
This breakdown of immune tolerance is a central driver of aging and chronic disease. It is the link between a local injury and systemic dysfunction. For example, a “leaky gut” (intestinal barrier hyperpermeability) allows bacterial components, such as lipopolysaccharide (LPS), to enter the bloodstream. This systemic inflammatory trigger can then break down the blood-brain barrier, allowing inflammation to spill into the central nervous system and activate microglia (the brain’s resident immune cells), contributing to neuroinflammation, brain fog, and chronic fatigue. The principles are universal: a breakdown in a barrier, a loss of immune tolerance, and a vicious cycle of inflammation.
The Case of the 19-Year-Old Woman: A Lesson in Immune Dysregulation
To make this tangible, let me share a clinical example. I recently worked with a 19-year-old young woman whose parents were concerned about her neurodivergent tendencies and a general lack of vitality. Her standard blood work was largely unremarkable, but a deeper dive revealed a story of profound immune dysregulation.
Her neutrophil count was persistently elevated. While neutrophils are our first responders to acute infection, chronically high levels suggest a state of sterile, low-grade inflammation. A closer look at her lymphocyte subsets and viral antibody panels told the real story. She had sky-high IgG antibodies to Epstein-Barr Virus (EBV).
Now, many people have been exposed to EBV. But her pattern was different. She had elevated antibodies to multiple viral components (VCA, EA, and EBNA), indicating a chronic, poorly controlled viral reactivation. Her immune system was “stuck” fighting a ghost. This constant battle was consuming vast amounts of energy and resources, contributing to her fatigue and neurological symptoms. Her immune system was unable to achieve resolution. It was locked in a state of perpetual, ineffective warfare, and her fascial and extracellular matrix environment was undoubtedly paying the price, becoming progressively more inflamed and dysregulated. This case highlights why we cannot look at any one system in isolation. Her neurological symptoms were a direct reflection of her immune dysregulation.
Metabolic Health: The Unseen Driver of Cellular Dysfunction
No discussion of cellular health and longevity is complete without a deep dive into metabolism, and specifically, the role of insulin. We live in an epidemic of metabolic dysfunction, and much of it is hidden, lurking beneath the surface of “normal” blood sugar readings.
The standard American diet, laden with processed carbohydrates and sugars, forces the pancreas to pump out large amounts of insulin to shuttle glucose out of the bloodstream and into cells. Over time, cells become resistant to this constant hormonal shouting. They “turn down the volume” on their insulin receptors. This is insulin resistance.
In response, the pancreas has to shout even louder, producing even more insulin to get the job done. This condition is called hyperinsulinemia (high insulin levels). For years, even decades, this compensatory mechanism can keep blood glucose levels in the “normal” range. The person’s A1C might be 5.5, and their fasting glucose might be 95 mg/dL. Their doctor tells them everything is fine.
But everything is not fine.
The Hidden Opportunity for Intervention
This period of “normoglycemic hyperinsulinemia” is a massive, missed opportunity for intervention. Insulin is a potent pro-growth and pro-inflammatory hormone. Chronically high levels of insulin are a powerful driver of the negative changes we’ve been discussing:
- It promotes fat storage, particularly in the form of inflammatory white adipose tissue (WAT).
- It directly stimulates inflammatory pathways.
- It contributes to cell proliferation and can accelerate cancer growth.
- It damages the endothelium (the lining of blood vessels), driving atherosclerosis.
- It fuels the inflammatory processes within the ECM.
This is why it is absolutely critical to measure fasting insulin alongside fasting glucose and HbA1c. A fasting insulin level above 8 μIU/mL, and certainly above 10, is a major red flag, even if glucose is normal. I once had a physician patient whose fasting glucose was only 100 mg/dL, but his fasting insulin was over 30. He was on the brink of a metabolic catastrophe and didn’t even know it. This wasn’t a knowledge gap; it was a measurement gap. By addressing his profound hyperinsulinemia with targeted dietary changes, we averted a crisis.
The popular GLP-1 agonists work by improving insulin sensitivity and promoting satiety. While they can be powerful tools, they should never be used in a vacuum. If the underlying lifestyle and dietary habits that drive insulin resistance are not addressed, these drugs become a mere crutch. The foundation must be restoring the body’s natural insulin sensitivity through whole foods, proper nutrient timing, and movement. For example, simply adding glycine, an amino acid that can improve insulin signaling, can be a supportive measure alongside these broader strategies.
The Non-Surgical Approach to Wellness with Chiropractic Care- Video
Practical Interventions: Modulating the Fascial-Immune-Metabolic Axis
Understanding this complex interplay among the fascial system, the immune system, and our metabolism enables us to be much more strategic and precise in our interventions. The goal is to break the vicious cycles of inflammation and fibrosis and restore the body’s innate capacity for healing and resolution.
Heat and Cold: A Nuanced Approach
Thermotherapy (heat) and cryotherapy (cold) are ancient and powerful tools, but they are often used indiscriminately. Their effects are profoundly different, and their application must be timed correctly.
- Cold Therapy (Cryotherapy): Cold causes vasoconstriction (narrowing of blood vessels) and has a potent acute anti-inflammatory effect. It slows down metabolic processes and reduces the initial swelling and pain signals immediately following an injury. Therefore, cold is best used for acute problems. Think of an athlete who just sprained their ankle. A short, targeted cold application can be very beneficial in the first 24-48 hours.
- However, chronic, long-term use of cold can be counterproductive to healing. By persistently suppressing inflammation, you also suppress the signals necessary for repair and remodeling. You are essentially hitting the “pause” button on the healing process. Short-term application is key.
- Heat Therapy (Thermotherapy): Heat causes vasodilation (widening of blood vessels), increasing blood flow to an area. This is crucial for the remodeling phase of healing. Increased blood flow brings in the oxygen and nutrients needed for fibroblasts to lay down new, healthy ECM. It also helps to flush out metabolic waste products that have accumulated in the area.
- Therefore, heat is best used for chronic conditions, stiffness, and to promote the later stages of tissue repair after the acute inflammatory phase has subsided. It helps to make the fascial matrix more pliable and supports the long-term process of restoring tissue quality.
Clinical Guideline:
- Acute Phase (0-72 hours post-injury): Use short-term, intermittent cold therapy to manage pain and swelling.
- Subacute/Chronic Phase (After 72 hours): Transition to heat therapy to promote blood flow, tissue relaxation, and remodeling. Avoid daily, habitual cold plunging if your goal is tissue repair and adaptation.
Beyond Temperature: Photobiomodulation and Peptides
Modern science offers even more targeted ways to influence this system.
- Photobiomodulation (PBM) / Red Light Therapy: This involves exposing the body to specific wavelengths of red and near-infrared light. The mitochondria, the powerhouses of our cells, absorb this light energy. The primary effect is to stimulate ATP production (cellular energy) and, in a controlled manner, transiently increase reactive oxygen species (ROS), triggering the body’s antioxidant and repair mechanisms. PBM can reduce inflammation, stimulate fibroblast activity for healthy collagen production, improve circulation, and modulate the immune response. It is a powerful tool for changing the phenotypic expression of cells—shifting them from a “danger” state to a “healing” state.
- Peptides: Peptides are short chains of amino acids that act as precise signaling molecules. They offer a way to give the body specific instructions. For example, BPC-157 (Body Protection Compound-157) is a peptide that has been shown in extensive research to accelerate the healing of a wide variety of tissues—muscle, tendon, ligaments, and even the gut lining. It appears to work by promoting angiogenesis (the formation of new blood vessels), modulating growth factor signaling, and protecting the endothelial barrier. When dealing with a “leaky gut” or a chronic tendon injury, BPC-157 can be a remarkable tool for restoring barrier integrity and facilitating repair.
The ultimate strategy involves a multi-pronged approach. We must change the terrain. This means cleaning up the diet to reverse hyperinsulinemia, using strategic movement to hydrate and mobilize the fascia, managing stress to calm the nervous system, and then layering in targeted therapies like PBM or peptides to provide the specific signals the body needs to break out of chronic dysfunction and re-engage its powerful, innate healing programs.
Disclaimer
The information contained in this educational post is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. It is not intended for self-diagnosis or to replace a qualified healthcare professional’s consultation. Dr. Alex Jimenez, DC, FNP-APRN, is not your medical provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this web page. All individuals must obtain recommendations for their personal situations from their own medical providers. Reliance on any information provided in this post is solely at your own risk.
Summary, Conclusion, and Key Insights
Summary
This educational post has provided a comprehensive overview of a modern, systems-based approach to health, longevity, and the treatment of chronic conditions. We began by redefining aging as a modifiable biological process, emphasizing the critical need for establishing a physiological baseline early in life for predictive and personalized medicine. We then delved into the profound importance of the fascial system and the Extracellular Matrix (ECM), recasting them as a dynamic, body-wide sensory and communication network rather than passive structural elements. We explored how this network’s health is determined by the behavior of cells such as fibroblasts, and how chronic inflammation and the Cell Danger Response (CDR) can lead to fibrosis, creating a “cellular prison” that impairs function and perpetuates disease. The intimate relationship between the fascial/ECM environment and the immune system was highlighted, explaining how immune dysregulation and a loss of tolerance can drive chronic inflammatory and autoimmune conditions. Furthermore, we identified hyperinsulinemia as a key, often hidden, metabolic driver of this systemic inflammation. Finally, we translated this complex physiology into a practical intervention framework, discussing the nuanced application of heat and cold therapies and introducing advanced modalities such as photobiomodulation and peptides as targeted tools to restore cellular function, modulate the immune response, and promote tissue remodeling.
Conclusion
The future of medicine lies in moving beyond siloed symptom-based treatment and embracing a holistic understanding of the body’s interconnected systems. The fascial network, the immune system, and our metabolic state are not separate entities; they are in constant, dynamic conversation. Health and vitality are emergent properties of a well-functioning, resilient biological system, while chronic disease results from a system stuck in a vicious cycle of dysfunction. By understanding the underlying physiology—from the densification of the ECM to the subtleties of immune cell signaling and the devastating impact of metabolic dysregulation—we can shift our focus from merely managing disease to actively cultivating health. The ultimate therapeutic strategy addresses the root causes: it cleans up the cellular environment, restores proper signaling, provides the necessary resources for repair, and empowers the body’s innate intelligence to heal itself. This evidence-based, integrative approach is the most powerful and promising path toward extending not just our lifespan, but our healthspan.
Key Insights
- Aging is Modifiable: View aging not as a fixed timeline but as a collection of biological processes (the “Hallmarks of Aging”) that can be influenced by lifestyle, environment, and targeted interventions.
- The Baseline is Everything: Proactively establishing a comprehensive biological baseline is the cornerstone of preventive and personalized medicine, enabling early detection of physiological deviations.
- Fascia is an Intelligent System: Your fascial network is a primary sensory and communication organ, not just structural “stuff.” Its health is paramount for overall well-being, movement, and cellular communication.
- The ECM Dictates Cellular Health: The state of the Extracellular Matrix—whether it is hydrated and fluid or dense and fibrotic—directly controls the function, survival, and behavior of every cell in your body.
- The Cell Danger Response (CDR) is a Vicious Cycle: A chronically activated CDR leads to a self-perpetuating cycle of inflammation and fibrosis, which is a root cause of many chronic pain and disease states.
- Measure Fasting Insulin: “Normal” blood sugar can mask dangerous hyperinsulinemia, a potent driver of chronic inflammation and metabolic disease. Measuring fasting insulin is a critical, non-negotiable health metric.
- Interventions Must Be Strategic: Therapies like heat, cold, PBM, and peptides are powerful but must be applied with a nuanced understanding of their physiological effects and the specific stage of tissue healing to be effective. The goal is to break the cycle of dysfunction and restore the body’s innate healing capacity.
References & Keywords
Keywords:
Longevity, Healthspan, Fascia, Fascial System, Extracellular Matrix (ECM), Cell Danger Response (CDR), Inflammation, Inflammaging, Cellular Senescence, Fibroblasts, Collagen, Myofascial Meridians, Immune System, Macrophages, T-cells, Immune Tolerance, Autoimmunity, Metabolic Health, Insulin Resistance, Hyperinsulinemia, Cryotherapy, Thermotherapy, Photobiomodulation (PBM), Red Light Therapy, Peptides, BPC-157, Personalized Medicine, Functional Medicine, Systems Biology, Dr. Alex Jimenez.
Selected References:
- López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M., & Kroemer, G. (2013). The hallmarks of aging. Cell, 153(6), 1194-1217.
- Schleip, R., Jäger, H., & Klingler, W. (2012). What is fascia? A review of different nomenclatures. Journal of Bodywork and Movement Therapies, 16(4), 496-502.
- Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7-17.
- Myers, T. W. (2014). Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists. 3rd ed. Churchill Livingstone.
- Franceschi, C., & Campisi, J. (2014). Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. The Journal of Gerontology: Series A, 69(Suppl_1), S4-S9.
- Crofts, C. A., Zinn, C., & Wheldon, M. (2015). The case for a low-carbohydrate diet in the management of type 2 diabetes. Expert Review of Clinical Pharmacology, 8(3), 263-265. [Note: Thematic reference for hyperinsulinemia concept].
- Hamblin, M. R. (2017). Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics, 4(3), 337-361.
- Seiwerth, S., Sikiric, P., et al. (2018). BPC 157 and standard angiogenic growth factors. Synergistic effects of BPC 157 and VEGF. Current Pharmaceutical Design, 24(18), 1972-1989.
- Bordoni, B., & Mahabadi, N. (2021). Fascia, Function, and Medical Applications. In StatPearls. StatPearls Publishing.
- Langevin, H. M., & Sherman, K. J. (2007). Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Medical Hypotheses, 68(1), 74-80.