The Benefits of Standing Lower Back Flexion for Pain Management
Could incorporating standing lumbar flexion exercise into a daily routine help decrease pain and improve overall spinal mobility for individuals with low back pain?

Standing Lower Back Flexion Exercise
A chiropractic physical therapy team visit can help determine which exercises are best for an individual’s injury or condition and teach them what to stop doing if they have low back pain. Exercise and proper posture can decrease discomfort and improve mobility for individuals with low back pain. (Suh, J. H. et al., 2019) Sometimes, exercises that bend backward are recommended, while other times, flexion or forward bending movements are the best way to manage lower back pain. Many find the standing Williams lumbar flexion exercises maneuver helpful for low back pain. (Amila A, Syapitri H, Sembiring E. 2021)
Benefits
Individuals with certain diagnoses may benefit from spinal flexion. These diagnoses include:
- Spinal stenosis (Lurie J., & Tomkins-Lane C. 2016)
- Degenerative disc disease
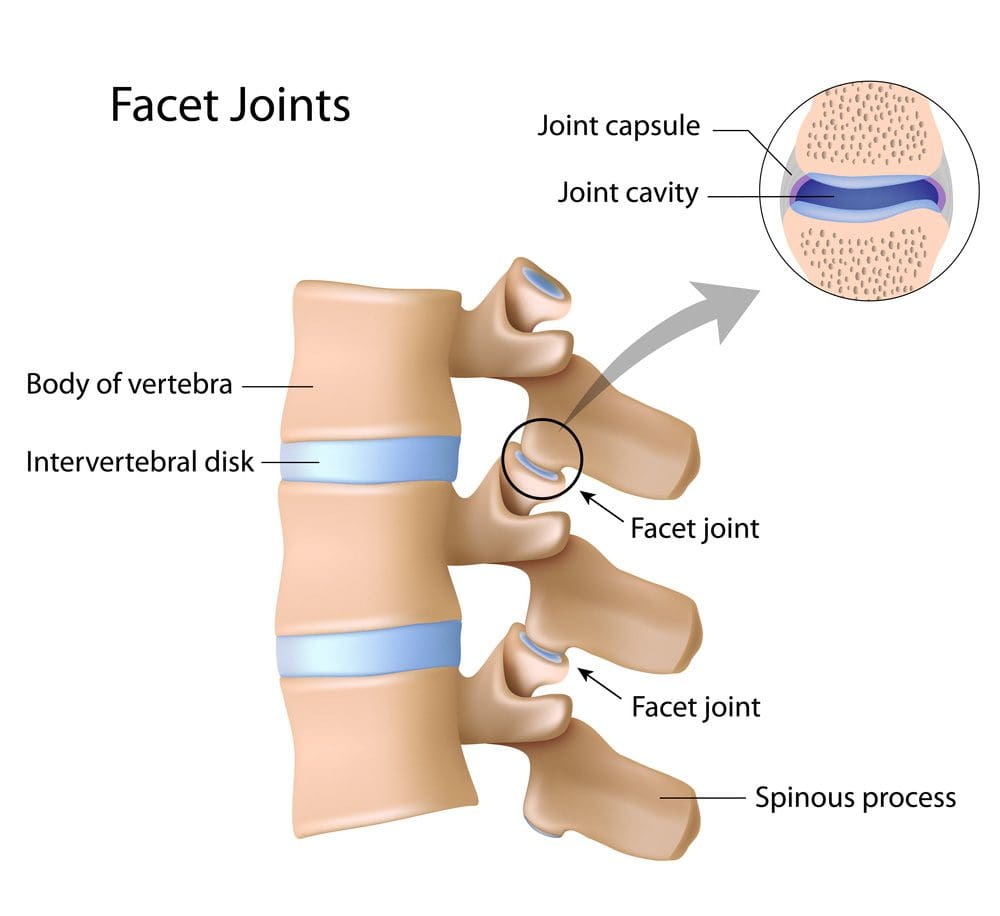
- Facet syndrome
- Spondylolisthesis
Be sure to speak with a healthcare provider to understand the diagnosis and low back symptoms, and work with a physical therapist to be sure that forward flexion of the spine is the correct exercise for your back.
When To Avoid Lumbar Flexion
Some should avoid excessive forward bending, which could cause further damage or injury to the spine. Reasons to avoid flexion include:
- Forward bending causes symptoms to worsen.
- Vertebral compression fracture (Sfeir J. G., Drake M. T., Sonawane V. J., & Sinaki M. 2018)
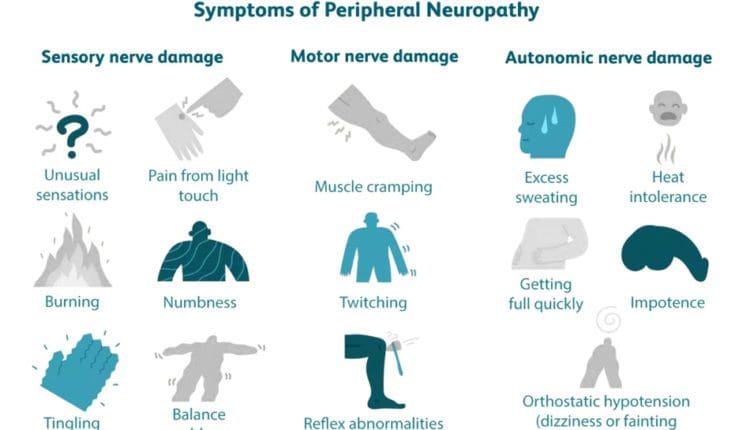
- Neurological signs such as difficulty urinating or controlling bowel movements (Howell E. R. 2012)
Before starting this or any other exercise program for your spine, check with a healthcare provider or physical therapist.
How to Perform
Gradually progressing with other gentle lumbar flexion exercises before full-standing lumbar flexion is recommended. These include performing a week or two of lumbar flexion lying down, followed by a couple weeks of lumbar flexion seated. Once these exercises are easy to perform and pain-free, progress with lumbar flexion standing postures.To perform, follow these steps:
- Stand with your feet shoulder-width apart.
- Slowly bend forward by sliding your hands down the front of your thighs.
- Reach down as far as possible and let your lower back bend forward.
- Grab your ankles and gently pull into more forward flexion to increase the backstretch.
- Hold the end position for a second or two, then slowly return to the starting position.
As you exercise, be sure to monitor changes in symptoms. Pain worsening in the back or traveling down your leg indicates that you should stop the exercise (Spine-health, 2017). If the pain decreases in your leg or centralizes to your back, continue the exercise. Standing lumbar flexion can be repeated for 10 repetitions a couple of times daily. It can help decrease low back or leg pain symptoms and stretch tight hamstrings and back muscles. (Montefiore Pediatric Orthopedic and Scoliosis Center, 2003)
Injury Medical Chiropractic and Functional Medicine Clinic
Exercise can also prevent future lower back problems. Standing back flexion, postural correction, regular physical activity, and exercise are tools for keeping the spine healthy. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems.
What Causes Disc Herniation?
References
Suh, J. H., Kim, H., Jung, G. P., Ko, J. Y., & Ryu, J. S. (2019). The effect of lumbar stabilization and walking exercises on chronic low back pain: A randomized controlled trial. Medicine, 98(26), e16173. https://doi.org/10.1097/MD.0000000000016173
Amila A, Syapitri H, Sembiring E. (2021). The effect of William Flexion Exercise on reducing pain intensity for elderly with low back pain. Int J Nurs Health Serv., 4(1), 28-36. https://doi.org/https://doi.org/10.35654/ijnhs.v4i1.374
Lurie, J., & Tomkins-Lane, C. (2016). Management of lumbar spinal stenosis. BMJ (Clinical research ed.), 352, h6234. https://doi.org/10.1136/bmj.h6234
Sfeir, J. G., Drake, M. T., Sonawane, V. J., & Sinaki, M. (2018). Vertebral compression fractures associated with yoga: a case series. European journal of physical and rehabilitation medicine, 54(6), 947–951. https://doi.org/10.23736/S1973-9087.18.05034-7
Howell E. R. (2012). Conservative management of a 31 year old male with left sided low back and leg pain: a case report. The Journal of the Canadian Chiropractic Association, 56(3), 225–232.
Spine-health. (2017). Exercise with lower back pain: Should you work through the pain? Spine-health
Knowledge from Veritas. https://www.spine-health.com/blog/exercising-lower-back-pain-should-you-work-through-pain
Montefiore Pediatric Orthopedic and Scoliosis Center. Center, M. P. O. a. S. (2003). Low Back Strain. https://www.cham.org/File%20Library/Global%20Navigation/Expertise%20And%20Programs/Pediatric%20Expertise/Orthopedics/Monte-LOW-BACK-STRAIN-WITH-EXERCISES.pdf