Chiropractic Care: How It Works For ACL Tears
Discover how chiropractic care can aid in recovery and improve your overall mobility after an injury like ACL tears.
Chiropractic Care for ACL Injuries: A Comprehensive Guide
Introduction
Picture this: you’re sprinting down the field, ready to make the game-winning move, when—pop—your knee gives out. Or maybe you just misstepped off a curb, and now walking feels like a high-stakes balancing act. Welcome to the world of an anterior cruciate ligament (ACL) injury, where your knee decides it’s had enough and takes an unscheduled vacation. These injuries are no laughing matter, but a little humor might help ease the pain of learning about them.
ACL tears are common, especially among athletes, but they can strike anyone daring enough to move quickly or pivot unexpectedly. The aftermath? Pain, swelling, instability, and a whole lot of frustration as daily tasks like climbing stairs or even standing become daunting challenges. Traditional treatments often involve surgery and months of physical therapy, but there’s another player on the field that might help: chiropractic care.
In this comprehensive guide, we’ll explore why chiropractic care can be a valuable part of ACL injury recovery. We’ll dive into the clinical rationale, drawing from scientific insights and the expertise of Dr. Alexander Jimenez, a distinguished chiropractor in El Paso, Texas. We’ll also highlight the role of chiropractic care in personal injury cases, particularly in El Paso, where Dr. Jimenez serves as a trusted liaison between medical care and legal documentation. So, grab a seat (carefully), and let’s explore how chiropractic care might help you get back on your feet—literally.
Understanding ACL Injuries
The ACL is one of four major ligaments in the knee, acting like a sturdy rope that keeps your tibia (shinbone) from sliding too far forward relative to your femur (thighbone). It also provides rotational stability, making it essential for activities involving quick changes in direction (Smith, 2020). When the ACL tears, it’s like cutting that rope, leaving your knee unstable and prone to further damage.
Causes and Symptoms
ACL injuries typically occur due to:
- Sudden stops or changes in direction (common in sports like soccer or basketball)
- Direct trauma, such as a tackle or collision
- Landing awkwardly from a jump
Symptoms include:
- A loud “pop” sound at the time of injury
- Immediate swelling
- Severe pain
- A feeling of instability or the knee “giving way”
These symptoms can make daily life a struggle. Walking becomes a cautious endeavor, stairs feel like a mountain, and even sitting for long periods can be uncomfortable. For athletes, an ACL tear can sideline them for months, if not longer, potentially derailing their careers. For non-athletes, it disrupts work, social activities, and overall quality of life.
Impact on Daily Life
Imagine trying to chase after your kids, carry groceries, or even walk your dog with a knee that feels like it’s made of jelly. ACL injuries can turn simple tasks into Herculean efforts. The instability can lead to compensatory movements, putting stress on other joints and muscles, which may cause additional pain or injuries. The emotional toll is also significant—being unable to do what you love can lead to frustration and even depression.
Traditional Treatment Approaches
Standard treatment for ACL injuries often follows the RICE protocol (Rest, Ice, Compression, Elevation) in the acute phase, followed by physical therapy to restore strength and mobility. In many cases, surgery (ACL reconstruction) is recommended, especially for active individuals or those with significant instability. Post-surgery, rehabilitation can take 6–12 months, with a focus on strengthening the muscles around the knee and improving proprioception (Krych et al., 2015).
But what if there’s more to the recovery puzzle? Enter chiropractic care, which might just be the missing piece you didn’t know you needed.
The Role of Chiropractic Care in Musculoskeletal Health
Chiropractic care is often stereotyped as just “cracking backs,” but it’s a sophisticated field focused on diagnosing and treating mechanical disorders of the musculoskeletal system, particularly the spine. The core principle is that proper alignment of the body’s structure allows it to function optimally and heal naturally (Cooperstein & Gleberzon, 2000). While chiropractic care is best known for addressing back pain, its benefits extend to other areas, including the extremities like the knees.
Core Principles of Chiropractic Care
Chiropractors use a variety of techniques, including:
- Spinal Adjustments: Manual manipulations to correct misalignments in the spine or joints.
- Soft Tissue Therapy: Techniques like massage or instrument-assisted mobilization to address muscle and ligament issues.
- Rehabilitation Exercises: Targeted exercises to strengthen muscles and improve coordination.
- Lifestyle and Nutritional Guidance: Advice on diet and activity to support overall health.
These techniques aim to restore balance, reduce pain, and enhance function, making chiropractic care a potential ally in ACL injury recovery.
Why Chiropractic Care for ACL Injuries?
While chiropractic care isn’t a cure for ACL tears, it can play a supportive role in several ways:
- Pain Management: Adjustments and soft tissue therapies can reduce pain and inflammation, helping patients manage symptoms without relying heavily on medications (Pollard et al., 2008).
- Biomechanical Correction: Misalignments in the spine or pelvis can affect how the knees function. Correcting these can reduce stress on the injured knee and improve overall movement patterns.
- Rehabilitation Support: Chiropractors can provide exercises to strengthen key muscles like the quadriceps, hamstrings, and glutes, which are crucial for knee stability.
- Holistic Approach: By addressing the entire body, chiropractic care can help prevent compensatory injuries and support overall recovery.
Research on chiropractic care specifically for ACL injuries is limited, but studies on related conditions offer insights. For example, a study on gluteal muscle activation showed that stimulating proprioceptive mechanisms can enhance muscle function, which is vital for knee stability (Bullock-Saxton et al., 1993). This principle can be applied to ACL rehabilitation, where strengthening surrounding muscles is a key focus.
Clinical Rationale for Chiropractic Care in ACL Injuries
The clinical rationale for using chiropractic care in ACL injury recovery lies in its ability to address pain, biomechanics, and rehabilitation. Let’s break it down:
Pain Management and Inflammation Reduction
In the acute phase of an ACL injury, pain and swelling are major hurdles. Chiropractic techniques like spinal adjustments can improve joint mobility and reduce nerve irritation, potentially alleviating pain. Soft tissue therapies, such as active release technique or Graston technique, can break down scar tissue and improve circulation, further reducing inflammation (Pollard et al., 2008).
Biomechanical Correction
The body works as a kinetic chain, where issues in one area can affect others. For example, a misaligned pelvis can cause the knee to track improperly, increasing stress on the ACL. Chiropractic adjustments can correct these misalignments, ensuring that the knee isn’t overcompensating for problems elsewhere in the body (Cooperstein & Gleberzon, 2000).
Rehabilitation and Muscle Strengthening
Rehabilitation is critical for ACL recovery, whether or not surgery is involved. Chiropractors can prescribe exercises to strengthen the muscles around the knee, such as the quadriceps, hamstrings, and glutes. Stronger muscles provide better support for the knee, reducing the load on the healing ligament. Additionally, proprioceptive training can help retrain the body’s sense of balance and coordination, which is often impaired after an ACL injury (Krych et al., 2015).
A study on gluteal muscle activation in walking found that stimulating proprioceptive mechanisms can enhance muscle function, which is crucial for stabilizing joints like the knee (Bullock-Saxton et al., 1993). This supports the idea that chiropractic care, which often includes proprioceptive exercises, can aid in ACL rehabilitation.
Supporting Ligament Healing
Ligaments heal through three phases: inflammation, proliferation, and remodeling. However, the resulting scar tissue is biomechanically inferior, with reduced strength and elasticity (Frank et al., 1999). Chiropractic care can support this process by promoting proper alignment and movement patterns, reducing stress on the healing ligament and preventing further damage.
Table: Phases of Ligament Healing and Chiropractic Support
| Phase | Description | Chiropractic Support |
|---|---|---|
| Inflammation | Hemorrhage and inflammation occur immediately after injury. | Pain management through adjustments and soft tissue therapy to reduce inflammation. |
| Proliferation | Scar tissue forms as cells proliferate to repair the ligament. | Exercises to maintain mobility and prevent excessive scar tissue buildup. |
| Remodeling | Scar tissue matures but remains weaker than original tissue. | Strengthening exercises and biomechanical corrections to support long-term stability. |
Source: Adapted from Frank et al. (1999)
Insights from Dr. Alexander Jimenez
Dr. Alexander Jimenez, a chiropractor and functional medicine practitioner in El Paso, Texas, brings a unique perspective to ACL injury treatment. His practice, accessible at dralexjimenez.com and chiromed.com, integrates chiropractic care with functional medicine, nutrition, and rehabilitation.
Holistic Approach
“An ACL injury isn’t just about the knee,” Dr. Jimenez explains. “It’s about the entire body. We need to look at the foot, ankle, hip, and spine to understand why the injury happened and how to prevent it from happening again.” His approach involves assessing the entire kinetic chain to identify contributing factors, such as misalignments or muscle imbalances.
Advanced Diagnostics
Dr. Jimenez uses advanced imaging, including digital X-rays and MRI, to assess the extent of the injury and monitor progress. “These tools give us a clear picture of what’s going on inside the knee,” he says. “They help us create a personalized treatment plan that addresses the specific needs of each patient.”
Soft Tissue Therapy and Nutrition
In addition to adjustments, Dr. Jimenez employs soft tissue therapies like active release technique and Graston technique to improve mobility and reduce scar tissue. He also emphasizes nutrition’s role in recovery. “Adequate protein, vitamins, and minerals are essential for tissue repair and reducing inflammation,” he notes. This holistic approach sets his practice apart, offering patients a comprehensive path to healing.
Contact Information
For more information, contact Dr. Jimenez at:
- Office: 915-850-0900
- Cell: 915-540-8444
- Email: [email protected]
Recovery From ACL Tears-Video
Chiropractic Care in Personal Injury Cases
El Paso, Texas, has a high rate of personal injury cases, often involving motor vehicle accidents, workplace injuries, or sports-related incidents. ACL tears are common in these scenarios, and chiropractic care plays a vital role in helping victims recover.
Why Chiropractic Care Matters
- Medical Documentation: Chiropractors like Dr. Jimenez provide detailed reports that document the injury’s extent and impact, which are crucial for legal proceedings.
- Holistic Recovery: Chiropractic care addresses physical, emotional, and psychological aspects of recovery, helping patients regain their quality of life.
- Rehabilitation Support: By complementing physical therapy, chiropractic care can speed up recovery and improve outcomes.
Dr. Jimenez’s Role in El Paso
Dr. Jimenez is a distinguished practitioner for personal injury victims in El Paso. His ability to associate injuries with advanced imaging and diagnostic evaluations makes him a trusted expert. “In personal injury cases, I act as a bridge between medical care and legal documentation,” he says. “My goal is to ensure patients get the treatment they need and the compensation they deserve.”
His dual-scope procedures—combining chiropractic care with functional medicine—provide comprehensive care that addresses both the injury and its broader impact on the patient’s life.
Table: Benefits of Chiropractic Care in Personal Injury Cases
| Benefit | Description |
|---|---|
| Detailed Documentation | Provides objective evidence of injury for legal claims. |
| Pain Management | Reduces reliance on medications through non-invasive techniques. |
| Holistic Recovery | Addresses physical and emotional aspects of injury. |
| Rehabilitation Support | Complements physical therapy to enhance recovery outcomes. |
A Light-Hearted Take on a Serious Topic
Let’s face it—ACL injuries are about as fun as a root canal without anesthesia. Your knee decides to go rogue, leaving you hobbling around like a pirate with a peg leg. Stairs? Forget it. They’re now your mortal enemy. But here’s where chiropractic care swoops in like a superhero (cape optional). It’s not going to magically knit your ligament back together, but it can help you manage the pain, move better, and maybe even laugh a little through the recovery process.
Think of chiropractic care as the friend who shows up with pizza when you’re having a bad day. It’s not going to solve everything, but it sure makes things a bit more bearable. And who knows? With the right adjustments and exercises, you might just be back to conquering those stairs in no time.
Conclusion
ACL injuries are a serious challenge, but chiropractic care offers a promising avenue for support. By managing pain, correcting biomechanics, and supporting rehabilitation, chiropractors like Dr. Alexander Jimenez can help patients navigate the road to recovery. In El Paso, where personal injury cases are common, his expertise is particularly valuable, providing both medical care and legal support.
However, chiropractic care is not a standalone solution. It works best as part of a multidisciplinary approach that includes orthopedic care, physical therapy, and lifestyle changes. If you’re dealing with an ACL injury, consult with a qualified healthcare professional to create a personalized treatment plan.
Disclaimer: This blog post is for informational purposes only and should not be taken as medical advice. Always consult with a qualified healthcare professional before starting any new treatment. For more information, visit dralexjimenez.com or chiromed.com.
References
- Bullock-Saxton, J. E., Janda, V., & Bullock, M. I. (1993). Reflex activation of gluteal muscles in walking: An approach to restoration of muscle function for patients with low-back pain. Spine, 18(6), 704–708.
- Cooperstein, R., & Gleberzon, B. (2000). Technique systems in chiropractic. Churchill Livingstone.
- Frank, C. B., Hart, D. A., & Shrive, N. G. (1999). Molecular biology and biomechanics of normal and healing ligaments—a review. Osteoarthritis and Cartilage, 7(1), 130–140.
- Krych, A. J., Woodcock, J. A., & Morgan, J. A. (2015). Treatment of anterior cruciate ligament tears: 25 years later, the controversy continues. Sports Health, 7(4), 362–368.
- Pollard, H., Bolt, J., & Aghabaglou, E. (2008). The use of the chiropractic left shift technique in the treatment of low back pain: A case report. Chiropractic & Osteopathy, 16, 16.
- Smith, J. (2020). Anterior cruciate ligament injury. StatPearls Publishing.












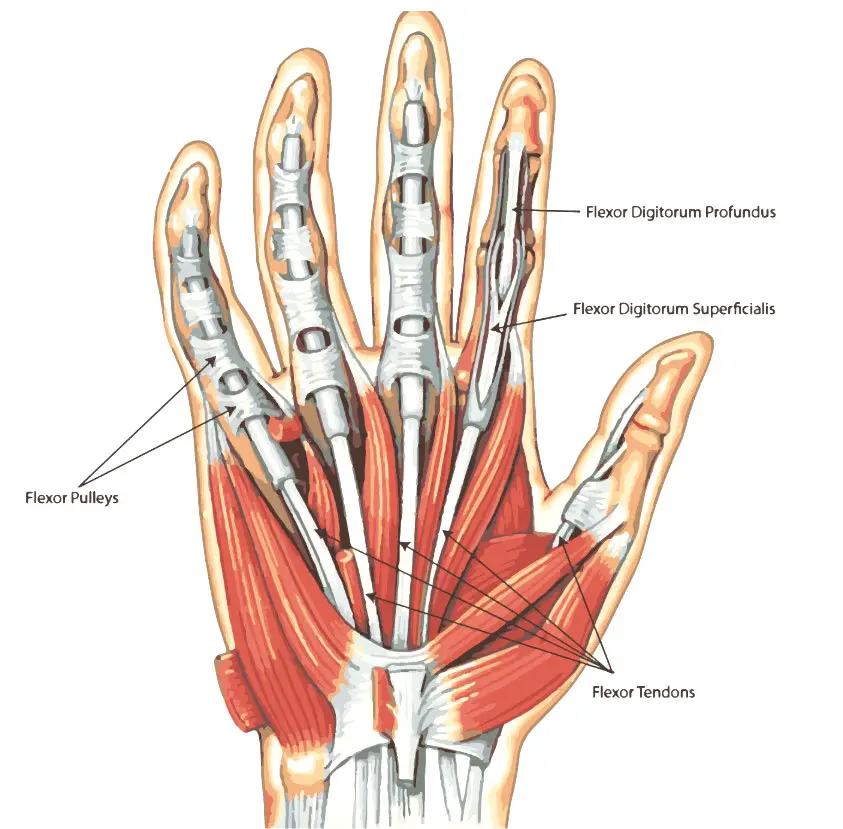
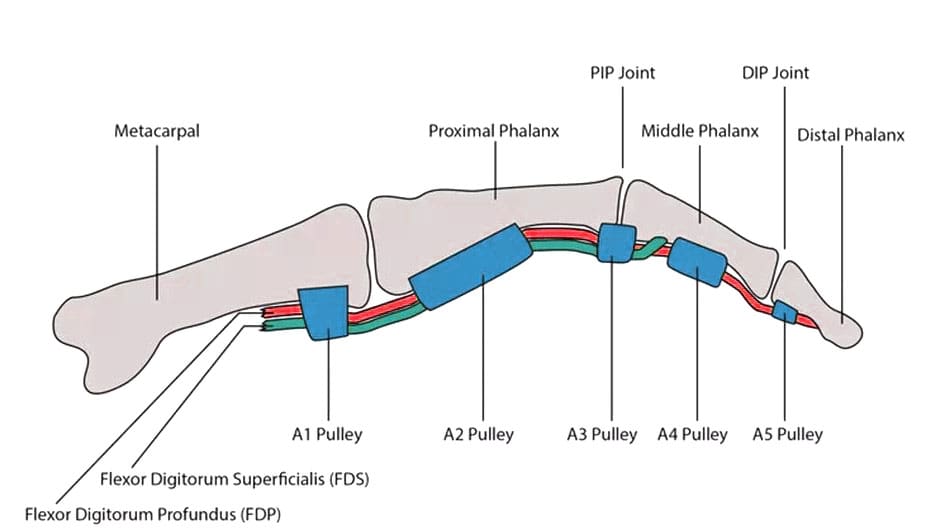 Digital Pulleys
Digital Pulleys