Length of Time for Muscle Tightness Relief
For individuals dealing with or experiencing muscle pain and stiffness, how long does it take to loosen tight muscles?

Length Of Time to Loosen Tight Muscles
Tight muscles are often caused by overuse or strain, combined with muscle soreness, a common symptom of tight muscles. The soreness peaks around the third day and begins to subside, typically resolving within a few days. But if tightness persists or is accompanied by other symptoms like numbness, inability to move, or swelling, it’s important to consult a medical provider. (Spine Medicine and Surgery of Long Island, 2024) However, it can take much longer for individuals who have never stretched and have had tight muscles for years, depending on the severity, injury history, and underlying causes.
Factors Influencing Timeline
Consistent stretching can take anywhere from a few weeks to a few months to noticeably loosen tight muscles and improve flexibility. The specific time frame depends on factors like the severity of the tightness, underlying causes, and individual consistency with stretching. (Peterson Physical Therapy, 2024)
Severity of Tightness
- Muscle knots and significant limitations in range of motion may take longer to resolve than minor stiffness.
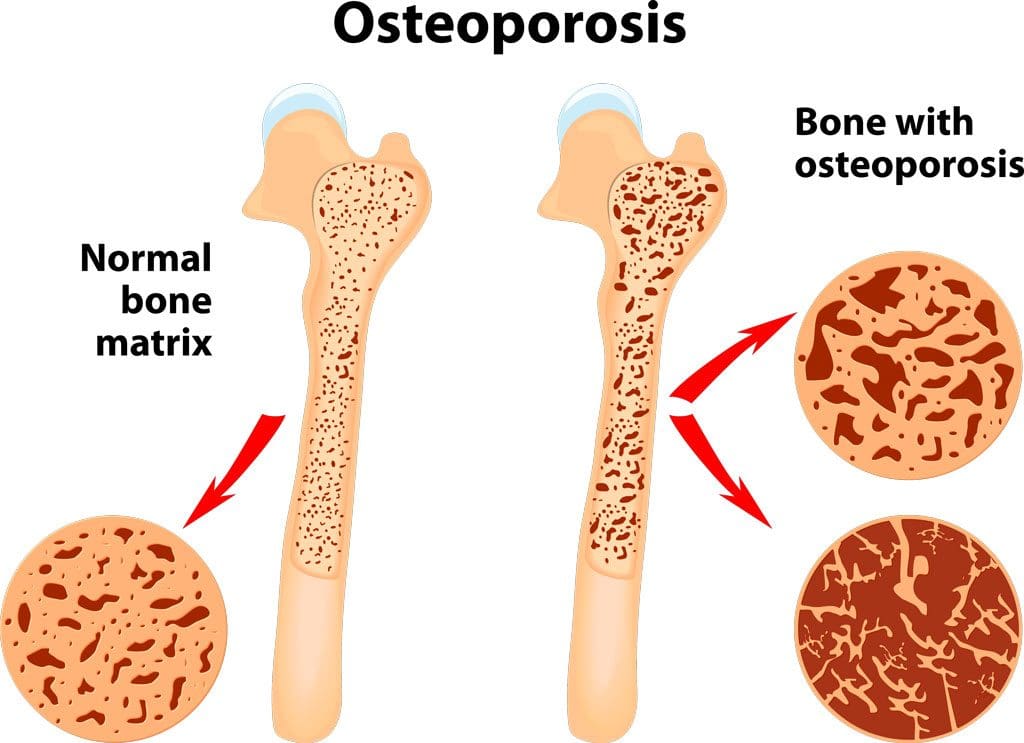
Underlying Causes
- If tightness is due to a specific injury or condition, addressing that cause is important for lasting and maintaining improvements. (Healthline, 2023)
Individual Factors
- Genetics, age, and overall health can influence how quickly muscles adapt to stretching.
Consistency
- Regular stretching, ideally daily or several times a week, is essential for feeling progress. (Mayo Clinic, 2023)
Stretching Routine
The length of time can vary based on the starting flexibility level and the specific stretching routine. (Mayo Clinic, 2023) It typically takes several weeks of consistent stretching, at least 3-4 times a week, to notice flexibility improvements. Longer-term changes, beyond the initial feeling of being looser, usually take 8 to 12 weeks.
Consistency
- Aim for at least 3-4 weekly stretching sessions, each lasting 20-30 minutes. (Harvard Health Publishing, 2022)
Hold Time
- Hold static stretches for at least 30 seconds.
- Longer holds (1-2 minutes) can provide deeper benefits.
Long-term Gains
- For substantial and sustained improvements, stretching consistently for several months is recommended. (Mayo Clinic, 2023)
Initial Changes
- Individuals may notice small improvements in the first few weeks, especially starting from a more inflexible position.
Influencing Factors and Results
- Individual genetics, current flexibility level, and the specific exercises can affect how quickly improvements are seen and felt. (Peterson Physical Therapy, 2024)
What To Expect
Improvements
- Within a few weeks, individuals might notice a decrease in the sensation of tightness or increased ease in reaching a stretch. (Peterson Physical Therapy, 2024)
Longer-Term Changes
- Significant muscle length and flexibility improvements may take several weeks to months of consistent effort.
Maintenance
- Once flexibility improves, ongoing stretching is needed to maintain those gains. (Harvard Health Publishing, 2022)
Treatment Options
- Stretching, physical therapy, massage, and other therapies can help alleviate tight muscles and promote recovery. (Spine Medicine and Surgery of Long Island, 2024)
- Consider professional guidance for specific concerns or limitations. Consult a physical therapist or healthcare provider for personalized recommendations.
The length of time to see results means consistency and patience are important.
Injury Medical Chiropractic and Functional Medicine Clinic
As a Family Practice Nurse Practitioner, Dr. Jimenez combines advanced medical expertise with chiropractic care to address various conditions. Our clinic integrates Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine to create customized care plans that promote natural healing, mobility, and long-term wellness. By focusing on flexibility, agility, and strength, we empower patients to thrive, regardless of age or health challenges. At El Paso’s Chiropractic Rehabilitation Clinic & Integrated Medicine Center, we passionately focus on treating patients after injuries and chronic pain syndromes. We focus on improving your ability through flexibility, mobility, and agility programs tailored for all age groups and disabilities. We use in-person and virtual health coaching and comprehensive care plans to ensure every patient’s personalized care and wellness outcomes.
Understanding Long-Lasting Injuries
References
Spine Medicine and Surgery of Long Island. (2024). How Long Do Muscle Knots Last? Spine Medicine and Surgery of Long Island. https://www.spinemedli.com/how-long-do-muscle-knots-last/#:~:text=The%20duration%20of%20a%20muscle,chronic%20pain%20if%20left%20untreated.
Peterson Physical Therapy. (2024). How Long Does It Take to Improve Flexibility? https://petersenpt.com/how-long-does-it-take-to-improve-flexibility#:~:text=Over%20the%20years%2C%20I’ve,takes%20to%20become%20more%20flexible.
Healthline. (2023). Everything You Need to Know About Muscle Stiffness. https://www.healthline.com/health/muscle-stiffness
Mayo Clinic. (2023). Stretching: Focus On Flexibility. https://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/stretching/art-20047931#:~:text=Stretch%20in%20a%20smooth%20movement,hold%20for%20around%2060%20seconds.
Harvard Health Publishing. (2022). Everyday Stretching. https://www.health.harvard.edu/everyday-stretching#:~:text=A%20daily%20regimen%20will%20deliver,or%20three%20times%20a%20week.