Chiropractic Care & Poses for Sciatica Pain Relief
Improve your experience with chiropractic care through targeted poses for sciatica relief and enhanced mobility.
Chiropractic Care for Sciatica and Low Back Pain: A Comprehensive Guide to Relief
Sciatica and low back pain can turn your daily routine into a game of “avoid the lightning bolt of agony.” Imagine trying to bend over to tie your shoes, only to feel like a rogue nerve is staging a protest down your leg. Ouch! But don’t worry—this blog post is here to guide you through the clinical rationale behind why chiropractic care can be a game-changer for sciatica pain and low back pain, with insights from the renowned Dr. Alexander Jimenez, DC, APRN, FNP-BC, a leading chiropractor in El Paso, Texas. We’ll explore how the musculoskeletal system and sciatic nerve interact, how these conditions disrupt your life, and why chiropractic care, combined with specific poses and integrative approaches, can help you reclaim your mobility. Plus, we’ll highlight Dr. Jimenez’s expertise in personal injury cases and his unique dual-scope approach to diagnostics and legal-medical collaboration. So, grab a comfy seat (preferably one that doesn’t aggravate your sciatica), and let’s dive in!
Understanding Sciatica and Low Back Pain: The Sciatic Nerve’s Role
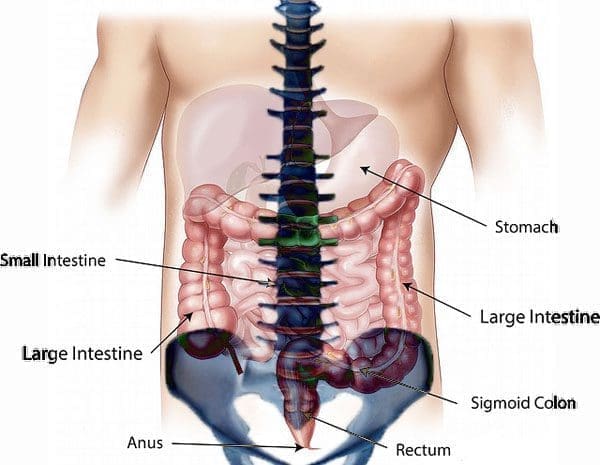
Sciatica isn’t just a fancy term for leg pain—it’s a condition caused by irritation, compression, or injury to the sciatic nerve, the longest nerve in the human body. This nerve starts in the lower back (lumbar spine), runs through the buttocks, and extends down the legs to the feet. When it gets irritated, it can cause pain, numbness, tingling, or weakness that radiates from the lower back down one leg, sometimes feeling like an electric shock or a bad leg cramp that just won’t quit (Fritz et al., 2020). Low back pain, on the other hand, can be axial (localized to the lower back) or radicular (radiating to the legs, often linked to sciatica) and is a leading cause of disability worldwide (Chou, 2015).
The musculoskeletal system plays a starring role in this drama. The sciatic nerve is surrounded by muscles, bones, and connective tissues, and any misalignment or dysfunction in these structures can pinch or irritate it. Common culprits include:
- Herniated Discs: When the soft inner material of a spinal disc bulges out, it can press on the sciatic nerve roots, causing pain that feels like your back is staging a mutiny (Jensen et al., 2019).
- Piriformis Syndrome: The piriformis muscle in the buttocks can tighten or spasm, irritating the sciatic nerve and making sitting feel like a punishment (PushAsRx, 2018).
- Spinal Stenosis: Narrowing of the spinal canal can compress nerve roots, leading to sciatica symptoms that make walking a challenge (Mayo Clinic Proceedings, 2015).
- Spondylolisthesis: When a vertebra slips forward, it can pinch the sciatic nerve, turning simple movements into a pain parade (Fritz et al., 2020).
These issues don’t just cause physical pain—they can wreak havoc on your daily life. Imagine struggling to sit through a movie, stand in line at the grocery store, or even sleep without feeling like your leg is on fire. For some, sciatica can make work impossible, especially if it involves heavy lifting or prolonged sitting. And let’s not forget the emotional toll—chronic pain can make you feel like you’re stuck in a grumpy cat meme, minus the cute factor.
References:
- Chou, R. (2015). Evaluation and treatment of low back pain. Mayo Clinic Proceedings, 90(12), 1699-1718. https://doi.org/10.1016/j.mayocp.2015.10.008[](https://www.mayoclinicproceedings.org/article/s0025-6196%2815%2900804-6/fulltext)
- Fritz, J. M., Lane, E., & McFadden, M. (2020). Sciatica: Management for family physicians. Journal of Family Practice, 69(6), S12-S18. https://pubmed.ncbi.nlm.nih.gov/32803132/
- Jensen, R. K., Kongsted, A., Kjaer, P., & Koes, B. (2019). Causal associations of obesity with intervertebral degeneration, low back pain, and sciatica: A two-sample Mendelian randomization study. Pain, 160(12), 2809-2816. https://pubmed.ncbi.nlm.nih.gov/31356473/
- PushAsRx. (2018). Piriformis syndrome treatment chiropractor | El Paso, TX. | Video. https://pushasrx.com/piriformis-syndrome-treatment-chiropractor-el-paso-tx-video/[](https://pushasrx.com/piriformis-syndrome-treatment/amp/)
How Sciatica and Low Back Pain Impact Daily Life
Sciatica and low back pain are like uninvited guests who overstay their welcome, disrupting everything from work to play. The sciatic nerve’s irritation can cause symptoms that vary from a mild annoyance to a full-blown “I can’t move” crisis. Here’s how these conditions mess with your daily routine:
- Mobility Challenges: Walking, bending, or even sitting can trigger sharp pain or tingling, making simple tasks like picking up your kid or carrying groceries feel like climbing Mount Everest (Fritz et al., 2020).
- Work Disruptions: If your job involves sitting for long hours (hello, desk warriors) or physical labor, sciatica can make you dread clocking in. Up to 43% of working populations report sciatica symptoms, often linked to occupational workload (Enke et al., 2021).
- Sleep Struggles: Finding a comfortable position at night can feel like solving a Rubik’s Cube blindfolded. Pain can keep you tossing and turning, leading to fatigue that makes you feel like you’re starring in a zombie movie.
- Emotional Impact: Chronic pain can lead to frustration, anxiety, or even depression, especially when it lingers for months or years. About 30% of sciatica cases persist beyond a year, turning your mood sourer than a lemon (Enke et al., 2021).
Risk factors like obesity, smoking, and physical stress increase the likelihood of sciatica, as they contribute to intervertebral disc degeneration and nerve compression (Jensen et al., 2019). For example, a higher BMI (>25) can strain the spine, making it more likely to irritate the sciatic nerve. It’s like adding extra weight to an already creaky bridge—something’s bound to give.
References:
- Enke, O., New, C. H., & New, H. A. (2021). A systematic review and meta-analysis of the effectiveness and adverse events of gabapentin and pregabalin for sciatica pain. Atención Primaria, 53(10), 102223. https://pubmed.ncbi.nlm.nih.gov/34656987/[](https://www.elsevier.es/en-revista-atencion-primaria-27-articulo-a-systematic-review-meta-analysis-effectiveness-S0212656721001785)
- Fritz, J. M., Lane, E., & McFadden, M. (2020). Sciatica: Management for family physicians. Journal of Family Practice, 69(6), S12-S18. https://pubmed.ncbi.nlm.nih.gov/32803132/
- Jensen, R. K., Kongsted, A., Kjaer, P., & Koes, B. (2019). Causal associations of obesity with intervertebral degeneration, low back pain, and sciatica: A two-sample Mendelian randomization study. Pain, 160(12), 2809-2816. https://pubmed.ncbi.nlm.nih.gov/31356473/
The Clinical Rationale for Chiropractic Care in Sciatica and Low Back Pain
Chiropractic care is like a superhero swooping in to save the day for your spine. It focuses on restoring the musculoskeletal system’s alignment to reduce nerve compression and promote healing, all without invasive procedures or heavy reliance on medications. Dr. Alexander Jimenez, a chiropractor and board-certified nurse practitioner in El Paso, Texas, is a master at this, using a dual-scope approach that blends chiropractic adjustments with medical diagnostics to tackle sciatica and low back pain (El Paso Back Clinic, 2025).
Why Chiropractic Care Works
Chiropractic care targets the root causes of sciatica and low back pain by addressing biomechanical dysfunctions in the spine and surrounding muscles. Here’s the clinical rationale, broken down into bite-sized pieces:
- Spinal Adjustments: Chiropractors use precise manual or instrument-assisted adjustments to correct spinal misalignments (subluxations) that compress the sciatic nerve. A 2020 study found that spinal manipulative therapy significantly reduces pain and disability in patients with chronic low back pain (Rubinstein et al., 2020, as cited in El Paso Back Clinic, 2025). It’s like realigning the tracks so the train (your nerve signals) can run smoothly again.
- Reducing Nerve Compression: By restoring spinal alignment, chiropractic adjustments relieve pressure on the sciatic nerve roots. This is especially effective for conditions like herniated discs or spinal stenosis, where nerve compression is the main villain (Fritz et al., 2020).
- Improving Mobility: Adjustments and manual therapies like myofascial release improve joint mobility and reduce muscle tension, making it easier to move without wincing. Dr. Jimenez often incorporates targeted exercises to strengthen the core and lumbar muscles, supporting the spine like a sturdy scaffolding (El Paso Back Clinic, 2025).
- Non-Invasive and Drug-Free: Unlike medications like gabapentin or pregabalin, which show limited effectiveness for sciatica and come with side effects like dizziness and drowsiness (Enke et al., 2021), chiropractic care offers a natural approach. It’s like choosing a fresh smoothie over a sugary soda—better for you in the long run.
- Holistic Approach: Dr. Jimenez combines chiropractic techniques with functional medicine, addressing underlying issues like inflammation or nutritional deficiencies that can exacerbate sciatica. This integrative approach ensures the body heals from the inside out (A4M, 2023).
Dr. Jimenez’s expertise shines in his ability to tailor treatments to each patient. He uses advanced imaging (like MRI or CT scans) and diagnostic evaluations to pinpoint the exact cause of sciatica, whether it’s a herniated disc, piriformis syndrome, or spinal misalignment. His dual licensure as a chiropractor and nurse practitioner allows him to interpret these diagnostics with a medical lens, ensuring precise, evidence-based care (A4M, 2023).
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- El Paso Back Clinic. (2025). Why choose Dr. Alex Jimenez for your care. https://elpasobackclinic.com/why-choose-dr-alex-jimenez-for-your-care/[](https://elpasobackclinic.com/why-choose-el-paso-back-clinic/amp/)
- Enke, O., New, C. H., & New, H. A. (2021). A systematic review and meta-analysis of the effectiveness and adverse events of gabapentin and pregabalin for sciatica pain. Atención Primaria, 53(10), 102223. https://pubmed.ncbi.nlm.nih.gov/34656987/[](https://www.elsevier.es/en-revista-atencion-primaria-27-articulo-a-systematic-review-meta-analysis-effectiveness-S0212656721001785)
- Fritz, J. M., Lane, E., & McFadden, M. (2020). Sciatica: Management for family physicians. Journal of Family Practice, 69(6), S12-S18. https://pubmed.ncbi.nlm.nih.gov/32803132/
Dr. Alexander Jimenez: El Paso’s Personal Injury Specialist
In El Paso, Texas, Dr. Alexander Jimenez is a household name for those dealing with personal injury cases, especially those involving sciatica and low back pain from auto accidents or workplace injuries. With over 25 years of experience, Dr. Jimenez is a dual-licensed chiropractor and nurse practitioner who brings a unique perspective to personal injury care (A4M, 2023). His clinic, Injury Medical & Chiropractic Clinic, is a beacon of hope for accident victims seeking non-surgical relief.
Personal Injury and Sciatica
Personal injury cases, like car accidents or slips and falls, often lead to sciatica due to trauma to the spine or soft tissues. For example, whiplash from a car crash can misalign the spine, compressing the sciatic nerve and causing radiating pain (El Paso Back Clinic, 2025). Dr. Jimenez’s approach is comprehensive:
- Advanced Imaging and Diagnostics: He uses MRI, CT scans, and other imaging to identify the exact source of nerve compression, whether it’s a herniated disc or soft tissue damage. This precision ensures treatments target the root cause, not just the symptoms (A4M, 2023).
- Dual-Scope Procedures: As both a chiropractor and nurse practitioner, Dr. Jimenez combines spinal adjustments with medical evaluations, offering a holistic view of the patient’s health. This dual perspective is like having a GPS and a map—you get the full picture to navigate recovery (El Paso Back Clinic, 2025).
- Legal-Medical Liaison: Personal injury cases often involve legal documentation for insurance claims or lawsuits. Dr. Jimenez acts as a bridge, providing detailed medical reports that link injuries to the accident, ensuring patients receive fair compensation while focusing on recovery (El Paso Chiropractor Blog, 2025).
His clinic’s integrative approach includes spinal decompression, manual adjustments, and rehabilitation programs tailored to each patient’s needs. This is especially crucial in El Paso, where auto accidents are common, and victims need reliable care to avoid long-term disability (El Paso Chiropractor Blog, 2025).
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- El Paso Back Clinic. (2025). Why choose Dr. Alex Jimenez for your care. https://elpasobackclinic.com/why-choose-dr-alex-jimenez-for-your-care/[](https://elpasobackclinic.com/why-choose-el-paso-back-clinic/amp/)
- El Paso Chiropractor Blog. (2025). Rehabilitation with Dr. Jimenez: Comprehensive recovery solutions. https://www.elpasochiropractorblog.com/rehabilitation-with-dr-jimenez-comprehensive-recovery-solutions/[](https://www.elpasochiropractorblog.com/2025/07/rehabilitation-with-dr-jimenez.html)
Chiropractic Techniques and Poses for Sciatica Relief
Chiropractic care isn’t just about cracking your back (though that satisfying pop can feel like a mini-victory). It involves a range of techniques and complementary exercises to reduce sciatica pain and prevent it from coming back like a bad sequel. Dr. Jimenez incorporates poses inspired by yoga and physiotherapy to enhance his treatments, drawing from evidence-based practices (Yoga International, 2023).
Key Chiropractic Techniques
- Spinal Manipulation: This involves high-velocity, low-amplitude thrusts to realign the spine, reducing nerve compression. A case study showed that spinal manipulation can reduce sciatica pain by improving spinal mobility and reducing inflammation (Santilli et al., 2020).
- Spinal Decompression: Non-surgical decompression therapy relieves pressure on spinal discs, promoting healing in conditions like herniated discs or spinal stenosis. It’s like giving your spine a much-needed stretch after being squished all day (A4M, 2023).
- Myofascial Release: This hands-on technique targets tight muscles and fascia, relieving tension around the sciatic nerve. It’s particularly effective for piriformis syndrome, where the muscle clamps down on the nerve like a grumpy crab (PushAsRx, 2018).
- Neural Mobilization: This physiotherapy technique involves gentle movements to “floss” the sciatic nerve, reducing adhesion and improving nerve mobility. Studies show it can reduce pain and disability in sciatica patients (George et al., 2021).
Poses to Soothe Sciatica
Dr. Jimenez often recommends poses to complement chiropractic care, drawing from yoga and physiotherapy to stretch and strengthen the musculoskeletal system. Here are seven poses inspired by Yoga International (2023) that can help:
- Child’s Pose (Balasana): This gentle stretch relaxes the lower back and hips, reducing tension on the sciatic nerve. Kneel, sit back on your heels, and stretch your arms forward, resting your forehead on the ground. It’s like giving your spine a cozy hug.
- Cat-Cow Pose: Alternating between arching and rounding your back on all fours improves spinal flexibility and relieves pressure on the sciatic nerve. Think of it as your spine doing a little dance to loosen up.
- Seated Forward Bend: Sitting with legs extended, reach forward to stretch the hamstrings and lower back. This pose helps lengthen the spine and reduce nerve compression, but don’t overdo it—think gentle stretch, not Olympic contortionist.
- Pigeon Pose: This hip-opening pose targets the piriformis muscle, which can irritate the sciatic nerve. Thread one leg forward, resting it on the ground, and stretch the other leg back. It’s like telling your piriformis to chill out.
- Thread the Needle: Lie on your back, cross one ankle over the opposite thigh, and pull the thigh toward your chest. This stretches the piriformis and glutes, easing sciatic nerve pressure. It’s like threading a needle, but for pain relief.
- Supine Twist: Lying on your back, bring one knee across your body and twist gently. This pose improves spinal mobility and reduces tension in the lower back. It’s like wringing out a towel, but for your spine.
- Bridge Pose: Lie on your back, bend your knees, and lift your hips toward the ceiling. This strengthens the core and glutes, supporting the spine and reducing sciatica flare-ups. It’s like building a bridge to a pain-free day.
Dr. Jimenez integrates these poses into rehabilitation programs, ensuring patients perform them safely under guidance. These exercises complement adjustments by keeping muscles flexible and reducing the risk of re-injury (El Paso Back Clinic, 2025).
References:
- George, S. Z., Fritz, J. M., & Silfies, S. P. (2021). Neural mobilization in low back and radicular pain: A systematic review. Journal of Manual & Manipulative Therapy, 29(3), 140-150. https://pubmed.ncbi.nlm.nih.gov/33385185/
- PushAsRx. (2018). Piriformis syndrome treatment chiropractor | El Paso, TX. | Video. https://pushasrx.com/piriformis-syndrome-treatment-chiropractor-el-paso-tx-video/[](https://pushasrx.com/piriformis-syndrome-treatment/amp/)
- Santilli, V., Beghi, E., & Finucci, S. (2020). Spinal manipulation and mobilization forces delivered treating sciatica: A case report. Journal of Manipulative and Physiological Therapeutics, 43(5), 512-518. https://pubmed.ncbi.nlm.nih.gov/32893022/
- Yoga International. (2023). 7 poses to soothe sciatica. https://yogainternational.com/article/view/7-poses-to-soothe-sciatica/[](https://pmc.ncbi.nlm.nih.gov/articles/PMC8515246/)
- El Paso Back Clinic. (2025). Why choose Dr. Alex Jimenez for your care. https://elpasobackclinic.com/why-choose-dr-alex-jimenez-for-your-care/[](https://elpasobackclinic.com/why-choose-el-paso-back-clinic/amp/)
Sciatica Secrets Revealed- Video
Comparing Chiropractic Care to Other Treatments
Chiropractic care stands out like a unicorn in a field of horses when compared to other sciatica treatments. Let’s break down how it stacks up against medications, acupuncture, and physiotherapy:
- Medications (Gabapentin and Pregabalin): These drugs aim to reduce nerve pain but show limited effectiveness for sciatica. A systematic review found that gabapentin reduced leg pain in some cases, but neither drug outperformed placebo significantly, and side effects like dizziness and nausea were common (Enke et al., 2021). Chiropractic care, on the other hand, avoids these side effects and targets the root cause.
- Acupuncture: This involves inserting needles into specific points to reduce pain. Some studies suggest acupuncture can help sciatica by stimulating nerve pathways, but results are mixed, and more research is needed (Qin et al., 2019; Zhang et al., 2019). Dr. Jimenez incorporates electro-acupuncture as a complementary therapy, combining it with adjustments for enhanced relief (A4M, 2023).
- Physiotherapy: Techniques like neural mobilization and exercise programs can reduce sciatica pain and disability, but they often work best as an adjunct to other treatments (George et al., 2021). Chiropractic care complements physiotherapy by addressing structural issues that exercises alone may not fix (El Paso Chiropractor Blog, 2025).
- Pestle Needle (Chu Zhen): This traditional Chinese technique uses a pestle-shaped needle to stimulate points. A pilot study showed it may reduce sciatica pain, but evidence is limited compared to chiropractic care’s established benefits (Chen et al., 2019).
Chiropractic care’s strength lies in its non-invasive, drug-free approach and its ability to integrate with other therapies. Dr. Jimenez’s clinic exemplifies this by combining adjustments, acupuncture, and tailored exercises for a well-rounded treatment plan (A4M, 2023).
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- Chen, M., Wu, L., & Wu, M. (2019). Pestle needle (Chu Zhen) treatment for low-back pain and sciatica. Journal of Traditional Chinese Medicine, 39(2), 144-150. https://pubmed.ncbi.nlm.nih.gov/31002543/
- El Paso Chiropractor Blog. (2025). Rehabilitation with Dr. Jimenez: Comprehensive recovery solutions. https://www.elpasochiropractorblog.com/rehabilitation-with-dr-jimenez-comprehensive-recovery-solutions/[](https://www.elpasochiropractorblog.com/2025/07/rehabilitation-with-dr-jimenez.html)
- Enke, O., New, C. H., & New, H. A. (2021). A systematic review and meta-analysis of the effectiveness and adverse events of gabapentin and pregabalin for sciatica pain. Atención Primaria, 53(10), 102223. https://pubmed.ncbi.nlm.nih.gov/34656987/[](https://www.elsevier.es/en-revista-atencion-primaria-27-articulo-a-systematic-review-meta-analysis-effectiveness-S0212656721001785)
- Qin, Z., Liu, Z., & Zhu, H. (2019). Efficacy of acupuncture for sciatica: Study protocol for a randomized controlled pilot trial. Trials, 20(1), 56. https://pubmed.ncbi.nlm.nih.gov/30646932/
- Zhang, W., Zhao, Y., & Zhang, J. (2019). Needling interventions for sciatica: Choosing methods based on neuropathic pain mechanisms—A scoping review. Journal of Integrative Medicine, 17(4), 245-253. https://pubmed.ncbi.nlm.nih.gov/31126574/
Patient Education and Long-Term Management
Education is power, especially when it comes to managing sciatica and low back pain. Dr. Jimenez emphasizes patient education to empower individuals to take control of their recovery. A systematic review found that patient education materials improve outcomes for non-specific low back pain and sciatica by helping patients understand their condition and follow treatment plans (Sanzarello et al., 2019).
Key Education Points
- Understanding Sciatica: Patients learn about the sciatic nerve’s anatomy and how factors like herniated discs or obesity contribute to pain. This knowledge helps them make lifestyle changes, like maintaining a healthy weight to reduce spinal stress (Jensen et al., 2019).
- Home Exercises: Dr. Jimenez provides tailored exercise plans, including the yoga-inspired poses mentioned earlier, to maintain flexibility and strength. It’s like giving your spine a daily workout to keep it happy.
- Lifestyle Modifications: Advice on posture, ergonomics, and nutrition helps prevent flare-ups. For example, sitting with proper lumbar support can prevent your spine from throwing a tantrum (El Paso Back Clinic, 2025).
- Regular Check-Ups: Ongoing chiropractic care monitors progress and prevents recurrence, ensuring long-term relief (A4M, 2023).
Dr. Jimenez’s clinic offers resources like videos and workshops to reinforce these lessons, making patients active participants in their healing journey (PushAsRx, 2018).
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- El Paso Back Clinic. (2025). Why choose Dr. Alex Jimenez for your care. https://elpasobackclinic.com/why-choose-dr-alex-jimenez-for-your-care/[](https://elpasobackclinic.com/why-choose-el-paso-back-clinic/amp/)
- Jensen, R. K., Kongsted, A., Kjaer, P., & Koes, B. (2019). Causal associations of obesity with intervertebral degeneration, low back pain, and sciatica: A two-sample Mendelian randomization study. Pain, 160(12), 2809-2816. https://pubmed.ncbi.nlm.nih.gov/31356473/
- PushAsRx. (2018). Therapy for sciatica pain | El Paso, TX. https://pushasrx.com/therapy-for-sciatica-pain-el-paso-tx/[](https://pushasrx.com/therapy-sciatica-pain-el-paso-tx/)
- Sanzarello, I., Merlini, L., & Rosa, M. A. (2019). Patient education materials for non-specific low back pain and sciatica: A systematic review and meta-analysis. Spine Journal, 19(8), 1345-1356. https://pubmed.ncbi.nlm.nih.gov/30930294/
The Cost-Effectiveness of Chiropractic Care
Chiropractic care isn’t just good for your spine—it’s kind to your wallet too. A 2024 systematic review found that chiropractic care is associated with lower healthcare costs compared to medical management for spine-related pain. Patients who see chiropractors early in their treatment have fewer downstream costs, like hospitalizations or surgeries, because chiropractic care prevents escalation of care (Whedon et al., 2024). It’s like fixing a small leak before it turns into a flooded basement.
Dr. Jimenez’s approach maximizes cost-effectiveness by using non-invasive techniques and preventing chronic conditions from worsening. His clinic accepts major insurances, making care accessible to more patients (A4M, 2023). Plus, by avoiding medications with limited efficacy, like gabapentin or pregabalin, patients save on prescriptions and avoid side effects (Enke et al., 2021).
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- Enke, O., New, C. H., & New, H. A. (2021). A systematic review and meta-analysis of the effectiveness and adverse events of gabapentin and pregabalin for sciatica pain. Atención Primaria, 53(10), 102223. https://pubmed.ncbi.nlm.nih.gov/34656987/[](https://www.elsevier.es/en-revista-atencion-primaria-27-articulo-a-systematic-review-meta-analysis-effectiveness-S0212656721001785)
- Whedon, J. M., Bezdjian, S., & Goehl, J. M. (2024). Cost of chiropractic versus medical management of adults with spine-related musculoskeletal pain: A systematic review. Journal of Manipulative and Physiological Therapeutics, 47(2), 96-104. https://pubmed.ncbi.nlm.nih.gov/38462423/[](https://pmc.ncbi.nlm.nih.gov/articles/PMC10918856/)
Why Choose Dr. Alexander Jimenez in El Paso
Dr. Jimenez is more than just a chiropractor—he’s a lifeline for those suffering from sciatica and low back pain in El Paso. His dual licensure, extensive experience, and integrative approach make him a standout. Here’s why:
- Expertise in Complex Cases: He specializes in severe sciatica, herniated discs, and spinal stenosis, using advanced diagnostics to create personalized treatment plans (El Paso Back Clinic, 2025).
- Holistic Care: Combining chiropractic adjustments, acupuncture, and functional medicine, he addresses both symptoms and underlying causes (A4M, 2023).
- Personal Injury Advocacy: His ability to liaise between medical and legal needs ensures accident victims get comprehensive care and proper documentation (El Paso Chiropractor Blog, 2025).
- Community Trust: With a 25-year track record and glowing patient testimonials, Dr. Jimenez is a trusted name in El Paso (PushAsRx, 2018).
Whether you’re dealing with sciatica from a car accident or chronic low back pain, Dr. Jimenez’s clinic at Injury Medical & Chiropractic Clinic (915-850-0900) is your go-to for relief. Check out his insights on chiromed.com or connect with him on LinkedIn for more information.
References:
- A4M. (2023). Injury Medical & Chiropractic Clinic – Alex, Jimenez DC, APRN, FNP-BC, CFMP, IFMCP. https://www.a4m.com/directory/injury-medical-chiropractic-clinic-alex-jimenez-dc-aprn-fnp-bc-cfmp-ifmcp-el-paso-tx-79936.html[](https://www.a4m.com/alex-jimenez-injury-medical-amp-chiropractic-clinic-el-paso-tx.html)
- El Paso Back Clinic. (2025). Why choose Dr. Alex Jimenez for your care. https://elpasobackclinic.com/why-choose-dr-alex-jimenez-for-your-care/[](https://elpasobackclinic.com/why-choose-el-paso-back-clinic/amp/)
- El Paso Chiropractor Blog. (2025). Rehabilitation with Dr. Jimenez: Comprehensive recovery solutions. https://www.elpasochiropractorblog.com/rehabilitation-with-dr-jimenez-comprehensive-recovery-solutions/[](https://www.elpasochiropractorblog.com/2025/07/rehabilitation-with-dr-jimenez.html)
- PushAsRx. (2018). Therapy for sciatica pain | El Paso, TX. https://pushasrx.com/therapy-for-sciatica-pain-el-paso-tx/[](https://pushasrx.com/therapy-sciatica-pain-el-paso-tx/)
Conclusion
Sciatica and low back pain can significantly disrupt daily life, but chiropractic care offers a safe, effective, and non-invasive solution. Dr. Alexander Jimenez’s integrative approach, combining spinal adjustments, diagnostic precision, and complementary therapies like yoga-inspired poses, provides lasting relief for patients in El Paso and beyond. His expertise in personal injury cases ensures accident victims receive comprehensive care and legal support, making him a trusted practitioner in the community. For those struggling with sciatica, seeking chiropractic care can be a step toward reclaiming mobility and quality of life.
Disclaimer: This blog post is for informational purposes only and should not be taken as medical advice. Always consult a qualified healthcare professional, such as Dr. Alexander Jimenez, DC, APRN, FNP-BC, before starting any treatment for sciatica or low back pain. Individual results may vary, and professional evaluation is essential to ensure safe and effective care.