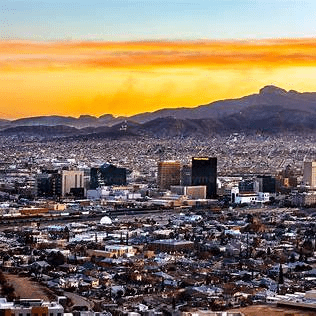
Healthy Eating on a Budget in El Paso, TX

Tips and Holistic Support from ChiroMed
In El Paso, Texas, people often ask how to eat healthy without spending a lot. Food prices are going up, and life is busy, so it’s a big deal. Healthy eating is about choosing foods that support your body, like fruits, veggies, whole grains, proteins, and dairy, while keeping costs low. This can help avoid issues like diabetes, heart problems, and being overweight. With good planning and smart choices, you can make good meals that don’t cost much. This article gives simple tips for shopping, cooking, and eating well in El Paso. It also shows how ChiroMed – Integrated Medicine Holistic Healthcare aligns with holistic care to support your health goals.
Plan Meals to Cut Costs
An ideal way to eat healthy and save money is by planning meals. Think about your week’s food, then list what to buy. This means you get only what’s needed and skip things that might spoil. Planning uses what you have at home, like stuff in your fridge or cabinets. Mix in fruits, veggies, grains, proteins, and dairy for balance.
Easy steps for planning:
- Look in your kitchen: Use items close to expiring first.
- Choose simple recipes: Ones with cheap things like beans or rice.
- Add snacks: Prep fruits or veggies for quick grabs.
- Stay flexible: Switch sale items.
In El Paso, where groceries can add up, this keeps bills down. For one person, you might spend about $64 per week, but planning helps you stay under. Use apps like MyFitnessPal to track needs.
Shop Smart for Cheap, Healthy Foods
Smart shopping makes healthy eating affordable. In El Paso, check local stores, markets, and discounts. Shop with a list, and after eating, skip impulse buys. Start in the outer aisles for fresh items, then move to the inner aisles for canned or frozen items.
- Get seasonal produce: In Texas, seasonal fruits and veggies are fresh and low-cost. Like summer blueberries.
- Pick frozen or canned: As tasty as fresh, and they last longer. Choose fruits in water or juice and low-salt veggies. These options are ideal for use in smoothies or soups.
- Visit farmers’ markets: Fresh items are cheap in El Paso. Find via the National Farmers Market Directory.
- Hunt sales and coupons: Use flyers, apps, and rewards. Bulk buy non-spoilers like rice.
- Check prices: Unit prices show deals. Generics match brands but are cheaper.
Stores like Grocery Outlet in El Paso have healthy deals. Skip convenience stores for lower prices. Stock up on nutritious food without going over budget.
Pick Affordable Nutritious Foods
You don’t need fancy foods for health. Choose cheap options from each group. Fill half your plate with fruits and veggies for vitamins, and they’re affordable. Whole grains like brown rice fill you up cheaply.
For protein, try beans, lentils, and eggs over meat sometimes. Cheap, healthy, and long-lasting. Do plant-based 1-2 days weekly in El Paso to save. Low-fat dairy adds calcium at a low cost.
- Fruits/veggies: Colorful, like carrots and apples. Frozen for stir-fries.
- Grains: Whole-wheat bread, pasta. Popcorn snacks.
- Proteins: Canned beans, water tuna.
- Dairy: Plain yogurt, add fruit yourself.
Batch cook for lasting meals. Make a large soup with vegetables and beans, then freeze some portions. Less waste, time. Try rice-bean salad or veggie stir-fry.
Local El Paso Resources for Healthy Eats
El Paso offers help for cheap healthy eating. Farmers’ markets offer low-priced produce; some accept SNAP. Eat Well El Paso adds healthy menu options, especially for kids. Better eating out without more cost.
Pantries and programs give free/low-cost food. Paso del Norte Health Foundation funds nutrition/cooking classes. SNAP, WIC, and school meals aid nutritious buys.
- Farmers’ markets: Seasonal, local support.
- Eat Well spots: Like Andale Mexican or Good Luck Café, healthy picks.
- Food banks: Central Texas tips and distributions.
- Classes: Free from groups like Common Threads.
Makes eating well easy on a budget in El Paso.
Holistic Care at ChiroMed for Health and Nutrition
Healthy eating links to full wellness. In El Paso, ChiroMed – Integrated Medicine Holistic Healthcare offers holistic help, including nutrition counseling. At 11860 Vista Del Sol Dr, Suite 128, they focus on whole-person care with spinal adjustments, rehab, and coaching to fix root issues.
Established in 1996, ChiroMed uses goal-oriented care with honesty and integrity. They mix conventional and alternative methods in personal plans. Services cover chiropractic, nutrition, physical rehab, naturopathy, acupuncture, nurse care, and injury/chronic pain rehab. They help with back/neck pain, migraines, sciatica, scoliosis, herniated discs, fibromyalgia, and stress.
The team includes Dr. Alex Jimenez (chiropractor and PT since 1999), Helen Wilmore (massage), Kristina Castle (PT), and Anthony Wills (chiropractor). They collaborate for outcomes.
Dr. Alex Jimenez notes that poor nutrition causes inflammation, pain, and chronic issues like diabetes or back problems. He suggests inexpensive foods like probiotic yogurt and veggies to reduce inflammation and aid healing. He combines chiropractic care with functional medicine to create affordable diet plans.
Care helps sciatica or arthritis by improving nerve function and using cheap proteins like beans. This approach teaches the importance of nutrition for maintaining spinal health, a crucial aspect of overall wellness. Fiber-rich foods save money, support digestion, and align with chiropractic principles.
In El Paso, this empowers affordable, healthy eating while addressing pain or movement issues. ChiroMed promotes natural healing and affordable options for a better life.
Make It Last for Good Health
In El Paso, budget-friendly healthy eating requires planning, smart shopping, and local support. Use frozen veggies, beans, and home cooking. Add ChiroMed’s holistic care for food-body links. Start one habit weekly, and get the family in. Leads to health without high costs.
References
American Heart Association. (n.d.). Cooking healthy on a budget
Scripps Health. (n.d.). How to eat healthy on a budget
UCSF Nutrition and Food Services. (n.d.). How to eat healthy on a budget
Lone Star Circle of Care. (2024). Eating healthy on a budget
Government of Canada. (n.d.). Healthy eating on a budget
Paso del Norte Health Foundation. (n.d.). Healthy eating and active living
City of El Paso. (n.d.). Eat Well El Paso
Queensland Health. (n.d.). How to stay healthy when you’re on a budget
American Heart Association. (n.d.). Grocery shopping tips
Tripadvisor. (n.d.). Healthy restaurants in El Paso
American Academy of Anti-Aging Medicine. (n.d.).
Alex Jimenez – Injury Medical & Chiropractic Clinic
Dr. Alex Jimenez. (n.d.). El Paso’s guide to probiotics and chiropractic healing
Impastato Chiropractic. (n.d.). Integrative chiropractor
Mount Carmel Health. (n.d.). 10 tips for eating healthy on a budget
American Heart Association. (n.d.). Eat healthy on a budget by planning ahead
ChiroMed. (n.d.). Integrated medicine holistic healthcare
Mayo Clinic Health System. (n.d.). Eating healthy on a budget
Tri County Clinic of Chiropractic. (n.d.). Why chiropractic care is the key to lasting wellness
Central Texas Food Bank. (n.d.). Shopping smart: Budget tips for nutritious and affordable meals
University of Georgia Health Center. (n.d.). Eating healthy on a budget
RC Chiropractic. (n.d.). Lifestyle advice
Optimize Health Chiropractic Center. (n.d.). Enhancing overall health through wellness care
West Texas Chiropractic Center. (n.d.). Nutrition
El Paso Back Clinic. (n.d.). Integrative chiropractic care benefits in El Paso
Valeo Clinic. (n.d.). Chiropractic techniques
Aktiv Integrative Chiropractic. (n.d.). Chiropractic services
Aktiv Integrative Chiropractic. (n.d.). Welcome to Aktiv Integrative Chiropractic